Translate this page into:
Non-venereal genital dermatoses and their impact on quality of life—A cross-sectional study
Corresponding author: Dr. P. S. S. Ranugha, Department of Dermatology, Venereology and Leprosy, JSS Academy of Higher Education and Research, MG Road, Mysore - 570 004, Karnataka, India. renukaderm@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Vinay N, Ranugha PSS, Betkerur JB, Shastry V, Ashwini PK. Non-venereal genital dermatoses and their impact on quality of life—A cross-sectional study. Indian J Dermatol Venereol Leprol 2022;88:354-9.
Abstract
Background:
Lesions on the external genitalia could be venereal or non-venereal. Non-venereal genital dermatoses are common and may cause considerable anxiety to patients, particularly if noticed after sexual intercourse. However, this aspect has not been studied much till now.
Objectives:
Our study proposes to describe the profile of non-venereal genital dermatoses and determine their impact on quality of life both social and sexual, using the dermatology life quality index questionnaire.
Methods:
We recruited patients aged 18 years and above, who were diagnosed to have non-venereal genital dermatoses during the study period. A detailed history was obtained and clinical examination done with relevant investigations when necessary. The dermatology life quality index was assessed and graded in all patients using Finlay dermatology life quality index questionnaire.
Results:
A total of 293 patients with non-venereal genital dermatoses were seen and 25 different dermatoses were observed. Men 242(82.6%) outnumbered women. The commonest age group affected was 31–50 years 144(50%). Chronic inflammatory dermatoses 135(41.6%) constituted the majority of cases. Scrotal dermatitis 46(15.7%), lichen simplex chronicus 37(12.6%), vitiligo 31(10.6%) were seen most frequently. In the study group, 111(37.9%) patients had moderate and 133(45.4%) had large impact on the quality of life. Erectile dysfunction was seen in 48(19.8%) men and 9(3.7%) had premature ejaculation. A significant effect on dermatology life quality index was found with increasing age (P = 0.007), positive marital status (P = 0.006), history of unprotected sex (P < 0.001), history of recurrences (P = 0.002) and venereophobia. (P = 0.008).
Limitations:
The number of women in the study group was less compared to men and we could not ascertain the type of sexual dysfunction in them.
Conclusion:
Non-venereal genital dermatoses are common, more so among men. They have a significant impact on the quality of life of the individual. Recognizing and addressing this problem will help in managing these patients effectively.
Keywords
Dermatology life quality index
genital psoriasis
genital vitiligo
non-venereal genital dermatoses
scrotal dermatitis
venereophobia
Introduction
A number of developmental, physiological, infective (venereal and non-venereal) / noninfective, traumatic or tumorous conditions can affect the genitalia.1 Non-venereal genital dermatoses may cause considerable anxiety to patients, particularly if noticed after sexual intercourse.1 Assessing the effect of these dermatoses on quality of life can help in providing appropriate treatment and counseling services. Our study describes the profile of non-venereal genital dermatoses and tries to determine their impact on quality of life both social and sexual, using the dermatology life quality index questionnaire.
Methods
This is a descriptive study done from November 2015 to May 2017 after institutional ethical committee approval. Consecutive new cases aged 18 years and above, attending the dermatology outpatient department of our hospital with genital complaints and clinically diagnosed to have dermatoses involving the genitalia were included after informed written consent. Patients with sexually transmitted infections were excluded. A detailed history regarding the evolution of lesions, treatment and sexual contact was taken. Clinical examination findings were noted on a preformed pro forma. Relevant investigations were done as and when necessary. We assessed the dermatology life quality index in all patients using Finlay dermatology life quality index questionnaire and graded it as shown in Figure 1.2
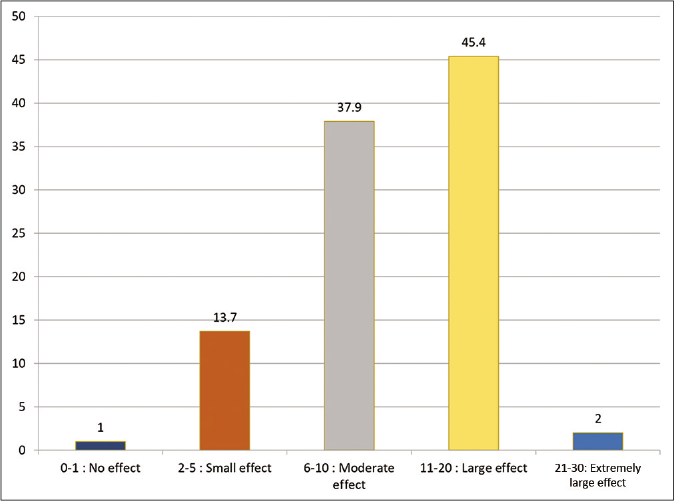
- Grading of dermatology life quality index in study subjects
Statistics
The data were tabulated as mean, median, standard deviation and proportions. Inferential statistics were done using oneway ANOVA. We used SPSS version 22 for statistical analysis. P < 0.05 was considered statistically significant.
Results
Out of 93,015 dermatology out-patients examined during the 18-month study period, the total number of patients, who came with genital complaints was 517, of which 166 (32.1%) were sexually transmitted infections, 293(56.7%) non-venereal genital dermatoses and 58 were inconclusive. Two hundred and ninety-three non-venereal genital dermatoses cases were included in the study. There were 242 (82.6%) males, who formed the majority of the study group with a men to women ratio of 4.8:1. The demographic details are given in Table 1. History of sexual contact with a non-regular partner was positive in 105(35.8%) (10 unmarried and 95 married) patients. Of these 105 cases, a history of sexual contact with a known person and commercial sex worker was present in 63(60%) and 42(40%) cases, respectively. Forty-one (39%) cases gave a history of contact with multiple partners. Of the 293 patients, 128(77.5%) were treated outside with inadequate or no response to treatment while 37(22.5%) gave a history of recurrences. The majority of our cases had isolated genital involvement 271(92.5%). In males, the scrotum was the most common site involved 131(54.1%), followed by penis in 82(33.9%) and both in 29(12%). Labia majora was the commonest site involved in women. Among 242 men with non-venereal genital dermatoses, 48(19.8%) had erectile dysfunction and 9(3.7%) had premature ejaculation. This was attributed to the skin lesion by the patient. A few females reported sexual difficulties; however, the type of sexual dysfunction could not be ascertained.
| Number of cases, n (%) | |
|---|---|
| Gender | |
| Male | 242 (82.6) |
| Female | 51 (17.4) |
| Age (years) | |
| 18-30 | 58 (19.8) |
| 31-50 | 144 (49.1) |
| 51-70 | 83 (28.3) |
| >70 | 89 (2.7) |
| Area | |
| Urban | 117 (39.9) |
| Rural | 176 (60.1) |
| Occupation | |
| Agriculture | 75 (25.6) |
| Housewives | 42 (14.3) |
| Self-employed | 70 (23.9) |
| Laborers | 25 (8.5) |
| Office/desk job | 57 (19.5) |
| Students | 24 (8.2) |
| Marital status | |
| Married | 257 (87.7) |
| Unmarried | 36 (12.3) |
We diagnosed 25 different non-venereal genital dermatoses in the study subjects as shown in Table 2 and Figures 2 and 3. They were categorized into inflammatory dermatoses (acute and chronic), tumors and others for the sake of convenience and a better understanding of results. Chronic inflammatory dermatoses 135(46.1%) formed the largest category, followed by other dermatoses 98(33.4%). Scrotal dermatitis 46(19%) [Figure 2a] was the most common non-venereal genital dermatoses among men and genital pruritus 19(37.3%) in women.

- Scrotal dermatitis with erythema and thickening of scrotal skin

- Genital vitiligo

- Lichen sclerosus et atrophicus affecting the labia majora and groin

- Angiokeratoma of Fordyce

- Vulval psoriasis
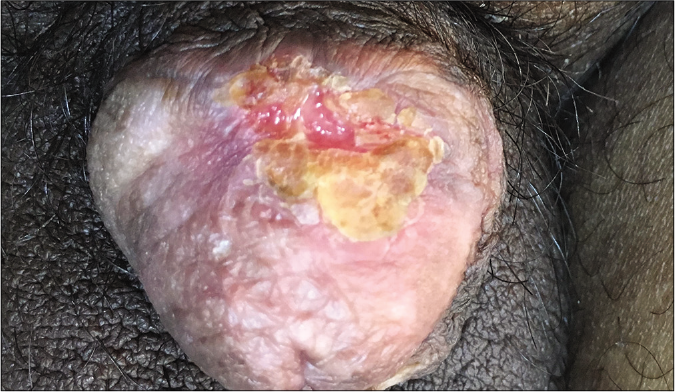
- Squamous cell carcinoma of the glans penis
In the study group, 111(37.9%) patients had moderate and 133(45.4%) had large impact on the quality of life. The median dermatology life quality index score was 10. Mean dermatology life quality index scores in patients with various dermatoses are presented in Table 2. The mean dermatology life quality index of each non-venereal genital dermatosis was compared with others within every category. Irritant contact dermatitis, Zoon’s balanitis, steatocystoma multiplex and traumatic ulcer patients had significantly higher scores than other dermatoses within the group of acute inflammatory, chronic inflammatory, benign tumors and others, respectively [Table 2] The mean dermatology life quality index score of each category/group was calculated and compared. Malignant tumor (squamous cell carcinoma) had the highest dermatology life quality index score when group means were compared [Table 2]. The mean dermatology life quality index was significantly higher in those with increasing age (P = 0.007), in married patients (P = 0.006), in those who had unprotected sex (P < 0.001), those with recurrences (P = 0.002), venereophobia (P = 0.008) and in those who noticed lesions after an act of sex (P = 0.01) [Table 3]. Individuals with a positive sexual contact history and those with multiple sex partners had a higher mean dermatology life quality index, though it was not statistically significant.
| Type | Diagnosis | Number of cases | Percentage | Mean DLQI | 95% CI | Mean DLQI of the group, mean±SD (95% CI) | |||
|---|---|---|---|---|---|---|---|---|---|
| Men | Women | Total | Lower bound | Upper bound | |||||
| Inflammatory dermatoses acute | Irritant contact dermatitis | 3 | 0 | 3 | 1.0 | 20.33±2.30 | 14.597 | 26.070 | 15.33±5.17 (12.76-17.90) |
| Angioedema | 3 | 0 | 3 | 1.0 | 17.33±8.33 | 13.095 | 19.238 | ||
| Pyoderma | 5 | 1 | 6 | 2.0 | 16.16±2.92 | 7.426 | 14.574 | ||
| FDE | 6 | 0 | 6 | 2.0 | 11.00±3.41 | 12.764 | 17.903 | ||
| Inflammatory dermatoses chronic | Zoon’s balanitis | 8 | 0 | 8 | 2.7 | 15.00±2.98 | 12.512 | 17.488 | 11.62±4.11 (10.92-12.32) |
| Scrotal dermatitis | 46 | 0 | 46 | 15.7 | 13.91±3.82 | 12.778 | 15.048 | ||
| LSC | 25 | 12 | 37 | 12.6 | 12.08±3.39 | 10.952 | 13.210 | ||
| Lichen planus | 14 | 2 | 16 | 5.5 | 9.06±2.52 | 7.722 | 10.403 | ||
| Psoriasis | 15 | 1 | 16 | 5.5 | 8.94±1.57 | 8.101 | 9.774 | ||
| LSEA | 0 | 6 | 6 | 2.0 | 7.83±2.23 | 5.495 | 10.172 | ||
| BXO | 3 | 0 | 3 | 1.0 | 6.00±1.73 | 1.697 | 10.302 | ||
| Lichen nitidus | 2 | 0 | 2 | 0.7 | 3.50±2.12 | −15.559 | 22.559 | ||
| Lichen striatus | 1 | 0 | 1 | 0.3 | 2.00 | ||||
| Benign | Skin tags | 1 | 0 | 1 | 0.3 | 10.00 | 6.56±3.83 (5.35-7.77) | ||
| Steatocystoma multiplex | 22 | 0 | 22 | 7.5 | 8.27±3.76 | 6.607 | 9.938 | ||
| Angiokeratoma | 10 | 0 | 10 | 3.4 | 5.80±2.44 | 4.054 | 7.546 | ||
| Nevi | 8 | 0 | 8 | 2.7 | 2.38±1.41 | 1.198 | 3.552 | ||
| Malignant | SCC | 1 | 0 | 1 | 0.3 | 25.00 | 25 | ||
| Other dermatoses | Traumatic ulcer | 6 | 0 | 6 | 2.0 | 15.83±4.79 | 10.804 | 20.863 | 10.21±4.81 |
| Chronic nonspecific ulcerative disease | 3 | 0 | 3 | 1.0 | 15.33±3.79 | 5.929 | 24.738 | ||
| Genital Pruritus | 9 | 19 | 28 | 9.6 | 13.57±3.71 | 12.134 | 15.009 | ||
| Venereophobia | 7 | 0 | 7 | 2.4 | 13.45±4.08 | 12.934 | 13.923 | ||
| PPP | 15 | 0 | 15 | 5.1 | 8.73±4.69 | 6.132 | 11.335 | ||
| Vitiligo | 21 | 10 | 31 | 10.6 | 6.55±2.66 | 5.574 | 7.523 | ||
| Scabies | 8 | 0 | 8 | 2.7 | 10.25±2.71 | 7.982 | 12.518 | ||
DLQI: dermatology life quality inBalanitis xerotica obliterans, SCC: squamous cell carcinoma, PPP: pearly penile papule, SD: standard deviation
| Parameter (number of cases) | Mean DLQI±SD | Pℽ |
|---|---|---|
| Age (years) | ||
| 18-30 (58) | 8.76±4.44 | 0.007 |
| 31-50 (144) | 11±4.92 | |
| 51-70 (83) | 11.28±4.91 | |
| >70 (89) | 12.63±3.85 | |
| Gender | ||
| Male (242) | 10.6±5.04 | 0.5 |
| Female (51) | 11.04±4.07 | |
| Area | ||
| Rural (176) | 10.49±4.72 | 0.4 |
| Urban (117) | 10.95±5.11 | |
| Occupation | ||
| Agriculture (75) | 11.29±5.55 | 0.06 |
| Housewife (42) | 11.10±4.15 | |
| Self-employed (70) | 10.69±5.07 | |
| Laborer (25) | 11.36±4.64 | |
| Office/desk job (57) | 10.37±4.35 | |
| Student (24) | 8.04±4.16 | |
| Marital status | ||
| Married (257) | 10.97±4.83 | 0.006 |
| Unmarried (36) | 8.58±4.77 | |
| Pre/extramarital sexual contact history | ||
| Yes (105) | 11.05±4.91 | 0.35 |
| No (188) | 10.47±4.87 | |
| Multiple partners | ||
| Yes (41) | 10.98±4.77 | 0.7 |
| No (64) | 10.63±4.91 | |
| Person known/CSW | ||
| Known (63) | 11.27±4.54 | 0.5 |
| CSW (42) | 10.71±5.47 | |
| Barrier contraceptives used | ||
| Yes (141/275) | 10.43±4.88 | <0.001 |
| No (134/275) | 11.37±4.82 | |
| Not applicable (18) | - | |
| Duration of dermatoses | ||
| Acute (<1 month) (34) | 12.09±3.46 | 0.9 |
| Chronic (>1 month) (259) | 10.18±7.49 | |
| Previously treated | ||
| Yes (128) | 12.69±4.26 | <0.001 |
| No (165) | 9.12±4.77 | |
| History of recurrences | ||
| Yes (37) | 12.95±4.24 | 0.002 |
| No (256) | 10.35±4.89 | |
| Erectile dysfunction | ||
| Yes (48/242) | 10.9±4.56 | 0.6 |
| No (194/242) | 10.5±5.13 | |
| Premature ejaculation | ||
| Yes (9/242) | 7.89±4.76 | 0.2 |
| No (233/242) | 10.70±5.02 | |
| Venereophobia | ||
| Yes (20) | 13.45±4.08 | 0.008 |
| No (273) | 10.48±4.88 | |
| Noticed lesions after sex | ||
| Yes (26/275) | 11.23±3.89 | 0.01 |
| No (249/275) | 10.88±4.92 | |
ℽ: One-way ANOVA test with post hoc, DLQI: dermatology life quality index, SD: standard deviation
Discussion
Large-scale studies on the prevalence of non-venereal genital dermatoses are lacking. Karthikeyan et al. reported the prevalence in males to be 14.1 per 10,000.3 In our study, it was 31.5 per 10,000 dermatology outpatients. Men were most commonly affected (82.6%) as has been observed by others4 We had a relatively lesser number of women which could be due to social inhibition and consultation in other departments like gynecology. Maximum number of our patients belonged to the age group of 31–50 years (49.1%), most authors have found these dermatoses to be more common in 21–40 years group.4-7 The larger surface area of scrotum might explain the higher frequency of scrotal involvement found by us, similar to others.3,5 Puri and Puri, however, found penis to be more commonly involved.4
There is a paucity of data on sexual contact history in patients with non-venereal genital dermatoses. Sampath et al. reported 46% of their patients as having a positive history of sexual exposure, but they have not described whether it was marital/ contact with a regular partner or extramarital/ contact with a non-regular partner.6 In the present study, 35.8% of cases, including seven women gave positive sexual contact history with a non-regular partner. The majority (83.9%) noticed these dermatoses after an act of intercourse.
A total of 25 different dermatoses were observed in this study of which, scrotal dermatitis (19%) followed by lichen simplex chronicus (10.3%) and steatocystoma multiplex (9%) were found to be common among men. Scrotal dermatitis was the commonest followed by vitiligo and fixed drug eruptions in a study.4 Saraswat et al. found vitiligo to be more common (18%) followed by pearly penile papules and fixed drug eruptions.5 Scabies was the most common genital dermatosis (15 %) in another report.7 However, only 2.7 % had scabies in our study. This might be because we included patients with genital complaints only. Genital pruritus (37.3%) was the commonest non-venereal genital dermatoses in women followed by lichen simplex chronicus (23.5%), vitiligo (19.6%) and lichen sclerosus et atrophicus (11.8%). Very few have studied non-venereal genital dermatoses in females, and one study reported lichen sclerosus et atrophicus to be the commonest.4 Whether the hot, humid climate and clothing habits of south India have any role in a higher incidence of genital pruritus needs to be evaluated further.
Dermatology life quality index is a validated tool to measure health-related quality of life and has been used in various studies to assess changes in quality of life.8 In a recent multicenter study on quality of life in dermatology patients, it was concluded that even the most localized or asymptomatic skin lesion leads to disruption of patient’s wellness at some level.9 Although several studies have been done on the quality of life in sexually transmitted infections and human immunodeficiency virus cases,10-16 there is a lack of data on the impact of non-venereal genital dermatoses on quality of life. There was an extremely large effect on the quality of life in 2%, a large effect in 45.4% and moderate effect in 37.9% cases. The mean dermatology life quality index score was significantly high among married than unmarried. A genital condition may cause pain or discomfort during intercourse or it may remove the desire of having intercourse for fear or shame, particularly when it is thought that the condition might be venereal in origin and also due to a fear that the regular sexual partner might be affected.17 Little or no impact of marital status on quality of life was found in patients having other dermatological disorders like psoriasis.18 Genital localization of the lesions could explain our observation. Higher dermatology life quality index scores in our patients having unprotected sexual contact might be due to anxiety of having contracted sexually transmitted infections or human immunodeficiency virus infection.
Many genital dermatoses have a chronic course with periods of remissions and exacerbations. Lack of response to treatment or recurrence may instill a fear of being affected by an incurable disease which may be the reason for a significant effect on the quality of life in these cases, as observed by us.
We also assessed the dermatology life quality index in relation to various dermatoses. Among the chronic inflammatory dermatoses, scrotal dermatitis, lichen simplex chronicus, Zoon’s balanitis had a large effect on the quality of life. Itching may be a confounding factor in worsening the quality of life in some of these dermatoses. Acute conditions like angioedema, irritant contact dermatitis had a large effect on the quality of life though their prevalence was low. The acute symptoms and signs, causing severe disability in daily activity might explain this. A large effect on the quality of life was also seen in patients with nonspecific genital pruritus and nonspecific ulcerative disease. Among tumors, benign tumors viz. steatocystoma multiplex and skin tags had a moderate effect, whereas an extremely large effect on the quality of life was seen in penile squamous cell carcinoma (mean dermatology life quality index-25). The knowledge of having cancer and the increasing size of the lesion might explain this finding. The mean dermatology life quality index in psoriatics with genital lesions was found to be 8.94 +/− 1.5 by us which is comparable to the values found by Meeuwis et al.19 It has been observed that quality of life and sexual health are more affected in psoriasis and vitiligo patients with genital lesions compared to those without.19-23 However, comparison with patients without genital lesions was beyond the scope of our study.
Venereophobia is an exaggerated or irrational fear of contracting a venereal disease following an isolated or multiple episodes of sexual intercourse that is observed exclusively in men.24 Patients with venereophobia had a higher mean dermatology life quality index score in our study. It is believed that patients attending a venereal disease clinic may have a sexual problem or develop one later.17 There are studies on erectile dysfunction in males with human immunodeficiency virus/acquired immunodeficiency syndrome.25,26 There is a lack of literature on non-venereal dermatoses causing sexual dysfunction. We observed erectile dysfunction in 19.8% and premature ejaculation in 3.7% cases. Genital psoriasis has a significant impact on sexual health in both men and women.20 Genital localization of lesions does not provoke worse sexual function in itself, but may probably have an impact on the subjective experience.27
Limitations
The number of women is relatively less compared to men and the type of sexual dysfunction in them could not be ascertained. Comparison of dermatology life quality index among patients with different dermatoses was not done by us due to the diverse presentations of conditions and interplay of several factors like age, marital status, the severity of itching and attitude of a spouse to the problem.
Conclusion
Non-venereal genital dermatoses are common, more so in men. As dermatologists, we need to be aware that they can have a significant impact on the quality of life. Hence, obtaining sexual contact history and assessment of the dermatology life quality index is essential. Better communication and proper counseling can increase patient’s acceptance of the disease and enhance the therapeutic outcome, thereby, improving their quality of life.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Non-venereological disorders of the genitalia In: Sacchidanand S, Oberai C, Inamdar AC, eds. IADVL Textbook of Dermatology (4th ed). Mumbai: Bhalani Publishing House; 2015. p. :2735-72.
- [Google Scholar]
- Dermatology Life Quality Index (DLQI)-A simple practical measure for routine clinical use. Clin Exp Dermatol. 1994;19:210-6.
- [CrossRef] [PubMed] [Google Scholar]
- Non-venereal dermatoses of male genital region-prevalence and pattern in a referral centre in South India. Indian J Dermatol. 2001;46:18-22.
- [Google Scholar]
- A study on non-venereal genital dermatoses in North India. Our Dermatol Online. 2013;4:304-7.
- [CrossRef] [Google Scholar]
- A study of pattern of nonvenereal genital dermatoses of male attending skin OPD at a tertiary care center. Indian J Sex Transm Dis. 2014;35:129-34.
- [CrossRef] [PubMed] [Google Scholar]
- A clinical study of patterns of non-venereal genital dermatoses of adult males in a tertiary care center. IOSR J Dent Med Sci. 2016;15:47-50.
- [Google Scholar]
- A study of 200 cases of genital lesions of non-venereal origin. Indian J Dermatol Venereol Leprol. 1998;64:68-70.
- [Google Scholar]
- The Children's Dermatology Life Quality Index (CDLQI): Initial validation and practical use. Br J Dermatol. 1995;132:942-9.
- [CrossRef] [PubMed] [Google Scholar]
- The impact of skin diseases on quality of life: A multicenter study. Actas Dermosifiliogr. 2017;108:244-52.
- [CrossRef] [PubMed] [Google Scholar]
- Quality of life, socioeconomic and clinical factors, and physical exercise in persons living with HIV/AIDS. Rev Saude Publica. 2017;51:66.
- [CrossRef] [Google Scholar]
- Human papillomavirus-related psychosocial impact of patients with genital warts in China: A hospital-based cross-sectional study. BMC Public Health. 2014;14:739.
- [CrossRef] [PubMed] [Google Scholar]
- Quality of life and related factors among people living with HIV/AIDS in Guangdong province. Zhonghua Liu Xing Bing Xue Za Zhi. 2014;35:40-4.
- [Google Scholar]
- Health-related quality-of-life of people with HIV in the era of combination antiretroviral treatment: A cross-sectional comparison with the general population. Lancet HIV. 2014;1:e32-40.
- [CrossRef] [Google Scholar]
- More than 20 years of research into the quality of life of people with HIV and AIDS-A descriptive review of study characteristics and methodological approaches of published empirical studies. J Int Assoc Provid AIDS Care. 2013;12:18-22.
- [CrossRef] [PubMed] [Google Scholar]
- Reliability and validity of dermatology life quality index: Assessment of quality of life in human immunodeficiency virus/acquired immunodeficiency syndrome patients with pruritic papular eruption. J Tradit Chin Med. 2013;33:580-3.
- [CrossRef] [Google Scholar]
- Dermatology quality of life impairments among newly diagnosed HIV/ AIDS-infected patients in the University of Ilorin Teaching Hospital (UITH), Ilorin, Nigeria. J Int Assoc Provid AIDS Care. 2013;15:328-31.
- [CrossRef] [PubMed] [Google Scholar]
- Limited role of marital status in the impact of dermatological diseases on quality of life. Eur J Dermatol. 2012;22:672-7.
- [CrossRef] [PubMed] [Google Scholar]
- Quality of life and sexual health in patients with genital psoriasis. Br J Dermatol. 2011;164:1247-55.
- [CrossRef] [PubMed] [Google Scholar]
- Genital psoriasis is associated with significant impairment in quality of life and sexual functioning. J Am Acad Dermatol. 2015;72:978-83.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of vitiligo on quality of life. Actas Dermosifiliogr. 2017;108:637-42.
- [CrossRef] [PubMed] [Google Scholar]
- Depression, anxiety and health-related quality of life in children and adolescents with vitiligo. Clin Exp Dermatol. 2011;36:360-5.
- [CrossRef] [PubMed] [Google Scholar]
- Association between vitiligo extent and distribution and quality-of-life impairment. JAMA Dermatol. 2013;149:159-64.
- [CrossRef] [PubMed] [Google Scholar]
- An approach to venerophobia in males. Indian J Sex Transm Dis AIDS. 2017;38:103-6.
- [CrossRef] [PubMed] [Google Scholar]
- Sexual dysfunction in HIV-positive men is multi-factorial: A study of prevalence and associated factors. AIDS Care. 2007;19:955-65.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and factors associated with erectile dysfunction in a cohort of HIV-infected patients. Int J STD AIDS. 2013;24:712-5.
- [CrossRef] [PubMed] [Google Scholar]
- Experience of sexuality in patients with psoriasis and constitutional eczema. Ned Tijdschr Geneeskd. 1992;136:2175-8.
- [Google Scholar]






