Translate this page into:
Obese male with linear skin tags: Looking beyond the role of obesity and insulin resistance
Corresponding author: Dr. Shyam Bhanushankar Verma, Nirvan Skin Clinic, 18 AMEE Society, Diwalipura, Vadodara, Gujarat, India. skindiaverma@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Verma SB, Ramamoorthy R, Wollina U. Obese male with linear skin tags: Looking beyond the role of obesity and insulin resistance. Indian J Dermatol Venereol Leprol. 2024;90:356-7. doi: 10.25259/IJDVL_134_2022.
Dear Editor,
A 39-year-old obese man visited one of us for concerns regarding multiple skin coloured and pigmented skin tags clustered on the neck, axillae and medial thighs and measured 2–7 mm. He had associated acanthosis nigricans in the same areas. Skin tags on the medial thighs were distributed bilaterally symmetrically in a linear pattern over acanthosis nigricans in that area [Figure 1]. He also complained of recurrent self-limiting erythema and irritation. He was obese with a body mass index of 34.9. His homeostasis model assessment of insulin resistance (HOMA-IR) level was 6.5, confirming severe insulin resistance. He was euglycemic, hypertensive and his triglyceride levels were 275 mg/dl with an otherwise normal lipid profile. He was a taxi driver driving daily for long hours wearing tight fitting V-shaped underwear, which constantly rubbed against his thighs. Diagnosis of skin tags was confirmed by histology.
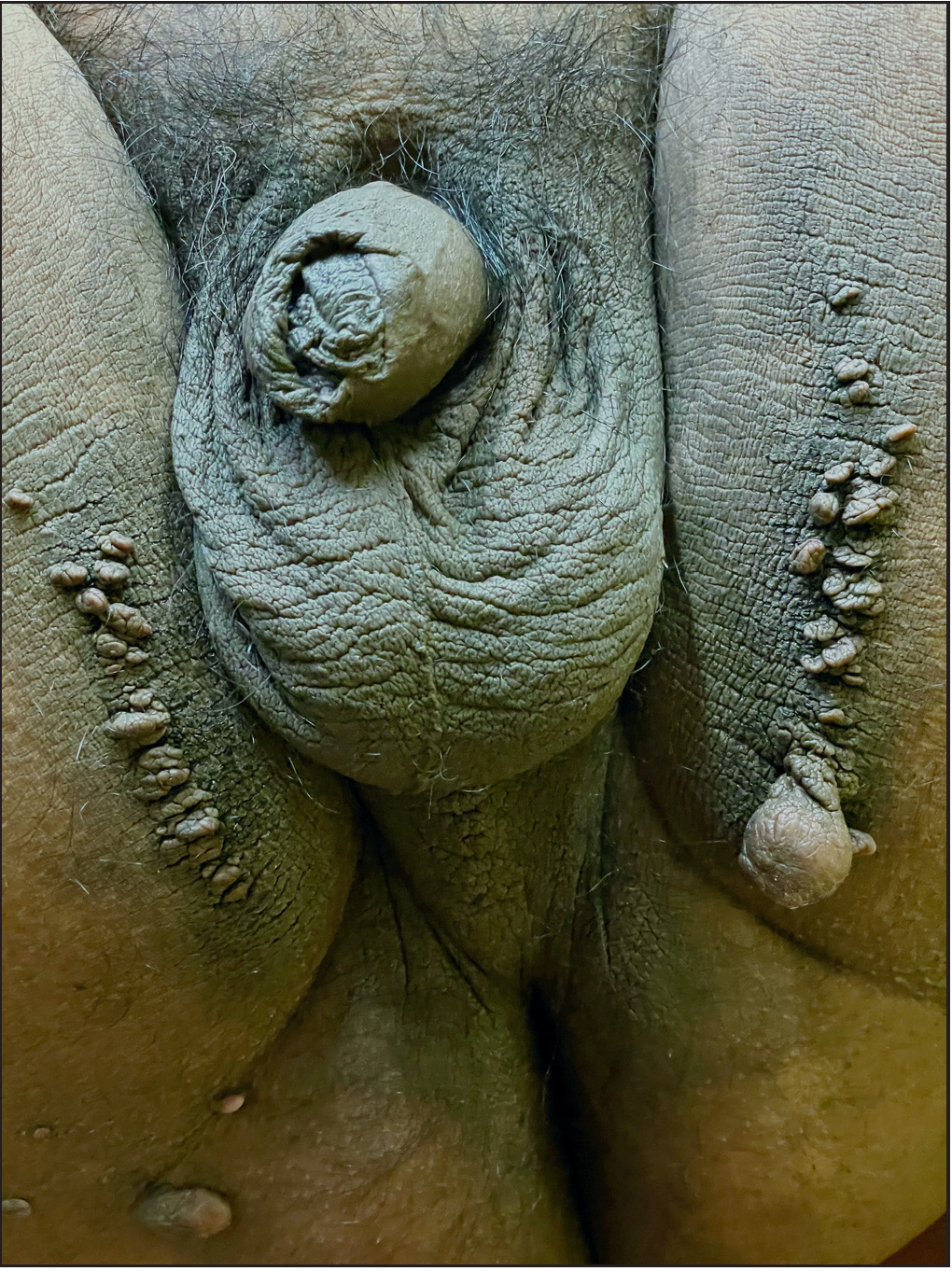
- Bilaterally symmetrical linear skin tags over medial thighs
Skin tags are extremely common benign soft tissue tumours estimated to occur in 46–60% of the population over the age of 50 years. While reviews of skin tags very commonly mention their association with obesity, hyperinsulinemia and diabetes, the role of friction in the pathogenesis of skin tags has received scant attention in dermatologic literature even though flexures where skin tags are most found are subjected to constant friction. A diligent search of the published literature revealed only two case reports of friction-induced skin tags.1,2 We describe a rare case of linear skin tags in an obese man. In addition to the proliferative effect of hyperinsulinemia on Insulin Growth Factor 1 receptors in dermal fibroblasts and keratinocytes, we highlight certain relevant observations regarding frictional trauma and their possible impact on mast cells, keratinocytes and fibroblasts, leading to development of skin tags.
The linear arrangement of skin tags corresponds to the sites subjected to maximum frictional trauma, which may be aggravated by perspiration reducing the threshold to injury following trauma. Keratinocytes subjected to mechanical trauma release alarmins3 like thymic stromal lymphopoietin, tumour necrosis factor α and interleukin (IL)-1 and IL-33. The latter is a powerful inducer for releasing mediators from skin mast cells.3,4 It is constitutively expressed in the nuclei of keratinocytes in abundance and released upon cellular stress with or without cytolysis. It is also found to release profibrotic cytokines such as tumour necrosis factor α, IL 13 and monocyte chemoattractant protein 1 from mast cells in the skin.4 Mast cells get accumulated at the site of skin tags and release pro-fibrotic cytokines, resulting in fibrosis. Tumour necrosis factor α has been incriminated as the key inducer of fibrosis in skin tags5. Linear distribution of skin tags prompts us to propose a role of epidermal alarmins in the genesis of skin tags by activating mast cells to release cytokines that induce fibrosis. Mast cells are concentrated in the papillary dermis, particularly near the dermo-epidermal junction. Physical trauma also directly activates mast cells that undergo transient receptor potential vanilloid-2 dependent degranulation.6 The optimum temperature range for activation of skin mast cells is from 23–30°C. The relevance of this fact in the pathogenesis of skin tags developing in warm locations like flexures needs to be investigated.
Frictional trauma to keratinocytes results in cellular proliferation and epidermal- mesenchymal transition.7 Transcriptional co-activators Yes-Associated Protein/Transcriptional co-activator with PDZ-binding motif (YAP/TAZ) and epidermal growth factor receptors have been identified as crucial players in a mechano-transduction cascade8 following application of mechanical force to keratinocytes and leads to the epidermal hyperplasia in skin tags.
In light of these considerations, we propose that linearly oriented frictional trauma would induce skin tags by releasing epidermal alarmins, keratinocyte proliferation and epidermal mesenchymal transition [Table 1]. The cellular and molecular intricacies involved in repeated low-grade frictional trauma leading to skin tags need to be further investigated.
Trigger factor
Target cell
Mechanism
Reference
1
Physical trauma
Keratinocyte
Epithelial mesenchymal transition
7, 8
2
Physical trauma
Keratinocyte
Alarmin release from keratinocyte
3, 4
3
Physical trauma
Mast cell
Transient receptor potential vanilloid-2-dependent degranulation
6
4
High temperature (>23–30°C)
Mast cell
Degranulation
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Acrochordons caused by friction from crutch use. Actas Dermosifiliogr. 2009;100:80-2.
- [PubMed] [Google Scholar]
- Mast cells and inflammation. Biochim Biophys Acta. 2012;1822:21-33.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Cytokines stimulated by IL-33 in human skin mast cells: Involvement of NF-κB and p38 at distinct levels and potent co-operation with FcκRI and MRGPRX2. Int J Mol Sci. 2021;22:3580.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The possible role of trauma in skin tags through the release of mast cell mediators. Indian J Dermatol. 2011;56:641-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Mast-cell degranulation induced by physical stimuli involves the activation of transient-receptor-potential channel TRPV2. Physiol Res. 2012;61:113-24.
- [CrossRef] [PubMed] [Google Scholar]
- Identification of biomechanical force as a novel inducer of epithelial-mesenchymal transition features in mechanical stretched skin. Am J Transl Res. 2015;7:2187-98.
- [PubMed] [PubMed Central] [Google Scholar]
- Control of cellular responses to mechanical cues through YAP/TAZ regulation. J Biol Chem. 2019;294:17693-706.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]





