Translate this page into:
Oculosporidiosis presenting as an under-eye swelling
2 Department of Otolaryngology, J.L.N Hospital & Research Center, Bhilai Steel Plant, Bhilai, India
3 Department of Ophthalmology, J.L.N Hospital & Research Center, Bhilai Steel Plant, Bhilai, India
4 Department of Pathology, J.L.N Hospital & Research Center, Bhilai Steel Plant, Bhilai, India
Correspondence Address:
A Ghorpade
Bhilai - 490006, Chhattisgarh
India
| How to cite this article: Ghorpade A, Gurumurthy J, Banerjee P K, Banerjee A K, Bhalla M, Ravindranath M. Oculosporidiosis presenting as an under-eye swelling. Indian J Dermatol Venereol Leprol 2007;73:196-197 |
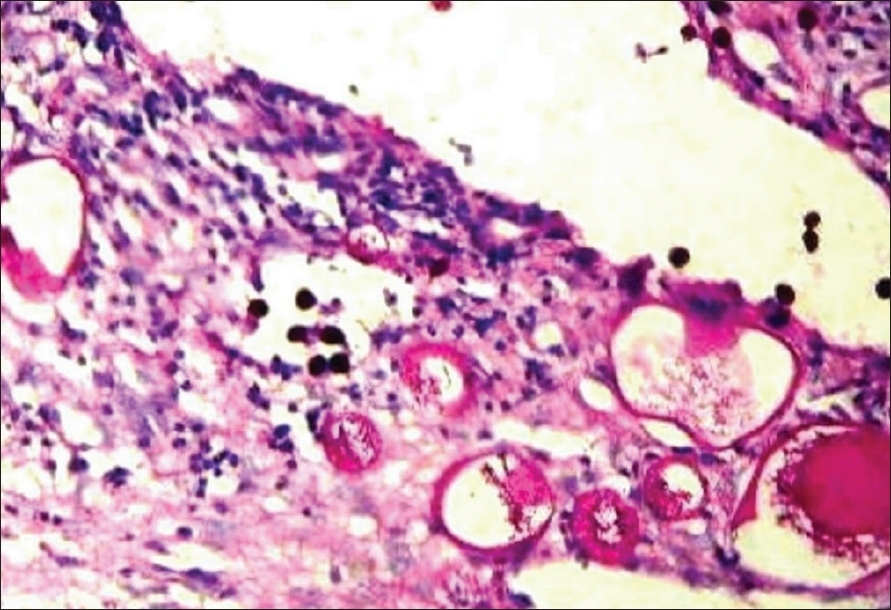 |
| Figure 2: Histopathology showing multiple sporangia in various developmental stages, some with endospores (H and E, x100) |
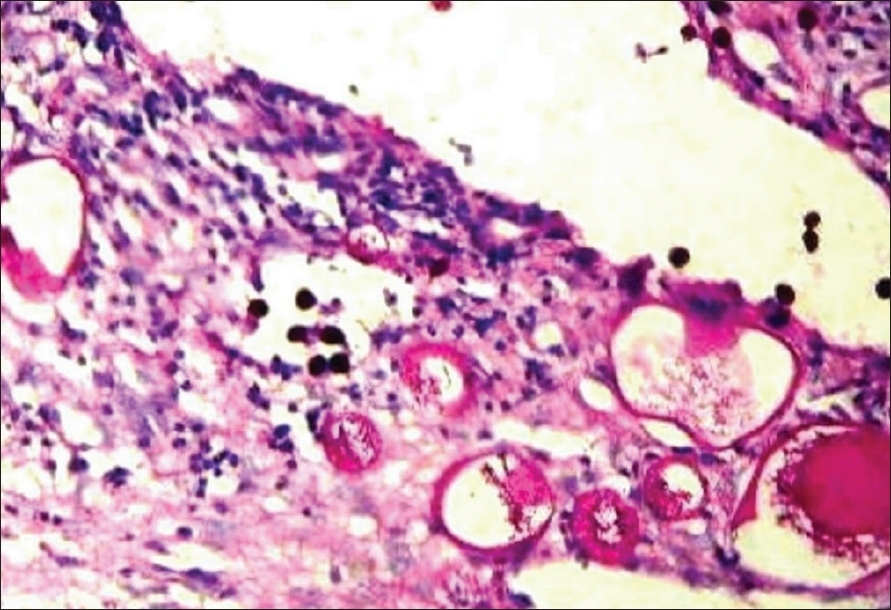 |
| Figure 2: Histopathology showing multiple sporangia in various developmental stages, some with endospores (H and E, x100) |
 |
| Figure 1: Skin colored swelling on the medial canthus of the right eye showing the orange peel appearance |
 |
| Figure 1: Skin colored swelling on the medial canthus of the right eye showing the orange peel appearance |
Sir,
Rhinosporidiosis is a chronic granulomatous infection of mucous membranes caused by Rhinosporidium seeberi , which presents usually to the otolaryngologist for vascular friable polyps. Several cases of rhinosporidiosis have been reported from Bhilai and neighborhood in the Chhattisgarh state. [1],[2],[3],[4] We came across a patient with ocular rhinosporidiosis who presented to the dermatology outpatient department with eyelid swelling. An 18-year-old male patient from a small village near Bhilai, was referred by an ophthalmologist for a gradually progressive swelling under the right eye of 8 months duration. He felt pain in the swelling since the last two weeks. A history of bathing regularly in the village pond with buffaloes was present. He had scanty bloody nasal discharge for 6 months, but had not consulted any doctor. There was no family history of similar complaints.
Cutaneous examination showed a diffuse, soft, skin colored, non-tender, fluctuant swelling over the right medial canthus, measuring about 4 cm x 3 cm in size [Figure - 1]. The overlying skin had an orange peel appearance albeit without any rise in local temperature. His systemic examination and blood count values were normal. FNAC from the lesion revealed multiple sporangia with endospores, pointing to the diagnosis of rhinosporidiosis. An otolaryngologist found a small pinkish mass in the right inferior meatus. The mass was reached under general anesthesia, through an incision in the right naso-optic sulcus. A pinkish mass with whitish small dots on its surface was found to occupy the lacrimal sac and project into the lacrimal duct. It was extracted from the upper opening of the duct and the part in the inferior meatus was excised separately from the right nasal chamber followed by electrocautery. Histopathology of the excised tissue revealed multiple sporangia with endospores [Figure - 2]. He was administered dapsone 100 mg daily orally, and has not had a recurrence since the last 8 months.
The causative organism of rhinosporidiosis has been now demonstrated to be an aquatic protistan parasite, and is currently included in a new class, the Mesomycetozoea, along with organisms that cause similar infections in amphibians and fish. It is the first known human pathogen from a novel clade of aquatic protistan parasites (Ichthyosporea). [5]
Ocular involvement may be seen in about 15% of cases of rhinosporidiosis. In a large series of oculosporidiosis, conjunctiva and lacrimal sac were found to be the most common structures involved. [6] The conjunctival lesions present as fleshy, pedunculated polyps studded with whitish dots representing mature sporangia. Isolated lacrimal sac rhinosporidiosis has been reported without nasal or conjunctival lesions. [7] In our patient, the lesions might have started in the nose and migrated up through the lacrimal duct into the lacrimal sac. FNAC is an important and easy diagnostic tool in this condition as shown in earlier reports. [1],[2],[3],[4] Meticulous excision with electric cautery remains the mainstay of treatment. Dapsone is known to cause fibrosis and shrinkage of the lesions and may prevent recurrences in some cases. Rhinsporidiosis localized only to the lacrimal sac and nasolacrimal duct, presenting with a swelling under the eye is uncommon. [7]
The term "dermosporidiosis" could be used to denote the cases of rhinosporidiosis presenting with predominant skin lesions, as has been recently suggested by the principal author. [ 3] If the skin lesion happens to be near the eye as in the present patient, a possibility of oculosporidiosis should be considered. Such a presentation may be puzzling for the treating physician unless this possibility is entertained, especially in the patients coming from an endemic region.
| 1. |
Ramanan C, Ghorpade A. Giant cutaneous rhinosporidiosis. Int J Dermatol 1996;35:441-3.
[Google Scholar]
|
| 2. |
Ghorpade A. Polymorphic cutaneous rhinosporidiosis. Eur J Dermatol 2006;16:190-192.
[Google Scholar]
|
| 3. |
Ghorpade A. Giant cutaneous rhinosporidiosis. J Eur Acad Dermatol Venereol 2006;20:88-89.
[Google Scholar]
|
| 4. |
Darbari BS, Gupta RL, Shukla IM, Arora MM. Rhinosporidiosis in Raipur. A clinicopathological study of 348 cases. Ind J Pathol and Bacteriol 1972;15:103-107.
[Google Scholar]
|
| 5. |
Fredricks DN, Jolley JA, Lepp PW, Kosek JC, Relman DA. Rhinosporidium seeberi: A human pathogen from a novel group of aquatic protistan parasites. Emerg Infect Dis 2000;6:273-282.
[Google Scholar]
|
| 6. |
Shreshtha SP, Hennig A, Parija SC. Prevalence of rhinosporidiosis of the eye and its adenexa in Nepal. Am J Trop Med Hyg 1998;59:231-234.
[Google Scholar]
|
| 7. |
Nerurkar NK, Bradoo RA, Joshi AA, Shah J, Tandon S. Lacrimal sac rhinosporidiosis: a case report. Am J Otolaryn 2004;25:423-5.
[Google Scholar]
|
Fulltext Views
2,685
PDF downloads
1,445





