Translate this page into:
Old world leishmaniasis presenting as a nasal mass
2 Department of Pathology, Imam Reza Hospital, Mashhad University of Medical Sciences, Mashhad, Iran
3 Department of Parasitology, Qaem Hospital, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran
4 Cutaneous Leishmaniasis Research Center, Department of Dermatology, Qaem Hospital, Mashhad University of Medical Sciences, Mashhad, Iran
Correspondence Address:
Pouran Layegh
Cutaneous Leishmaniasis Research Center, Department of Dermatology, Qaem Hospital, School of Medicine, Mashhad University of Medical Sciences, Mashhad
Iran
| How to cite this article: Bakhshaee M, Shabani S, Farzadnia M, Shamsian SA, Layegh P. Old world leishmaniasis presenting as a nasal mass. Indian J Dermatol Venereol Leprol 2014;80:145-147 |
Abstract
Mucosal leishmaniasis is a major problem in Latin America but has been rarely noticed in our region. Although there have been a few reports of mucosal involvement especially in the oral cavity from Southwest Iran, yet none have been presented from the Northeast where Leishmania tropica is the major concern. We report a patient with endonasal leishmaniasis due to L. tropica, an extremely rare entity in immunocompetent patients in our region. He presented with a mass in the left nasal vestibule causing a sense of obstruction on the same side, accompanied by occasional rhinorrhea and mild epistaxis. This case exemplifies the need for considering leishmaniasis as a differential diagnosis for nasal obstruction in this endemic area.Introduction
Leishmaniasis is a disease caused by protozoan parasites that belong to the genus Leishmania. It is classified into three major clinical types: Cutaneous mucocutaneous, and visceral. It is noteworthy that in humans, different species of the parasite are associated with different forms of the disease. [1]
Mucocutaneous leishmaniasis (espundia), which is a form of tegumentary leishmaniasis, usually occurs in Latin America where it is caused by L. braziliensis and less commonly by L. panamensis/L. guyanensis. Except for L. infantum and rarely L. aethiopica, L. donovani,[2] and L. peruviana, mucosal involvement is not a common presentation in old world cutaneous leishmaniasis (CL) especially due to L. tropica or L. major. In such cases, if the lesion is situated around the oral or nasal cavity, it may spread across the mucocutaneous margins and expand along the lips or nose without causing the severe destruction usually seen in American mucocutaneous leishmaniasis. [3]
Although mucosal involvement mostly in the oral cavity has been previously presented in a few reports from the Southwest of Iran, in this paper, we report a case of endonasal leishmaniasis, an extremely rare entity in immunocompetent patients and especially in this endemic area. [4]
Case Report
A 14-year-old boy from the Khaje Rabee region of Mashhad, Northeast of Iran was referred to the otolaryngology clinic for a left-sided nasal mass. The patient complained of feeling a mass in the left nasal vestibule causing a sense of obstruction on the same side, accompanied by occasional rhinorrhea and mild epistaxis from 2 months prior to referral. On nasal examination a bright red, 1.5 cm nodule was observed located in the anterior part of the left nasal vestibule. This nodule was covered with serosanguinous crusts, was moderately infiltrated and bled easily [Figure - 1]. Endoscopy of both nasal cavities revealed no other mucosal lesions. On physical examination of other body parts, two skin lesions were noted on the left forearm [Figure - 2]a and the left oral commissure [Figure - 2]b, a sign of the cutaneous leishmaniasis diagnosed 2 years earlier. The disease had been initially treated with intralesional pentavalent antimoniate (glucantime) and as the response was unsatisfactory, he had also received an intramuscular course of the drug resulting in complete resolution. Biochemical tests and the humoral and cell-mediated immunity panel were all normal.
 |
| Figure 1: Endoscopy of the left nasal fossa showing an infiltrated erythematous nodule in the anterior part of the left septum |
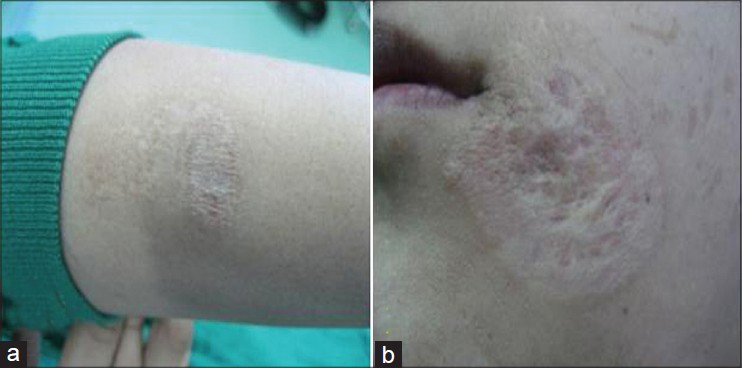 |
| Figure 2: (a) Atrophic scar on the left forearm skin (b) Atrophic scar on the left oral commissure |
A lesional smear was taken and stained with Giemsa which highlighted numerous intra- and extracellular basophilic bodies of Leishmania. Endoscopic biopsy showed a dense infiltration of histiocytes with numerous intracellular and extracellular Leishmania amastigotes in addition to lymphocytes, plasma cells and a few eosinophils [Figure - 3]a and b.
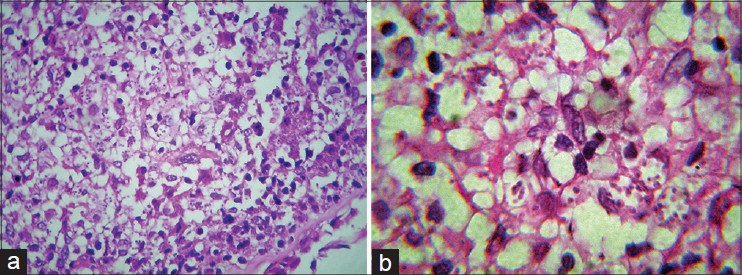 |
| Figure 3: (a and b) Endoscopic endonasal biopsy showing intracellular and extracellular leishmania amastigotes, H and E, ×10, ×40 respectively |
Tissue samples that were studied for protozoa typing by polymerase chain reaction, confirmed the presence of L. tropica complex deoxyribonucleic acid [Figure - 4].
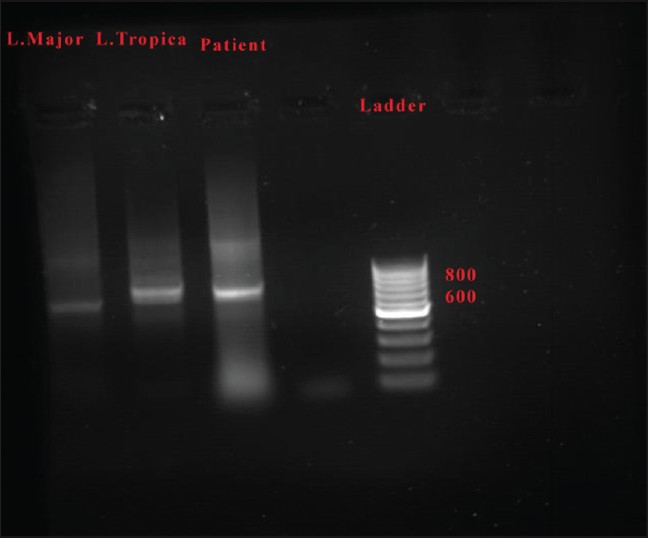 |
| Figure 4: Leishmania species-specific multiplex polymerase chain reaction (PCR). Extracted deoxyribonucleic acid from the specimen was introduced to a species-specific multiplex PCR for L. tropica and L. major. The results indicate the presence of Leishmania tropica in the skin lesion |
On the basis of clinical and laboratory test results, endonasal leishmaniasis was confirmed as the final diagnosis. Treatment was initiated with intramuscular injection of pentavalent antimoniates (Glucantime, Aventis, France) 20 mg/kg/day for 20 days.
Full healing was achieved along with improvement of symptoms without any significant side effects. No recurrence has been observed after 1 year of follow-up.
Discussion
Cutaneous leishmaniasis is a chronic parasitic disease which is endemic in many regions of the world; 90% of all cases occur in seven countries: Afghanistan, Algeria, Brazil, Iran, Peru, Saudi Arabia, and Syria. [5] Leishmaniasis is a diverse and complex disease. Each species can produce more than one clinical form of the disease and each form of the disease could be caused by multiple species. [1] Mucosal leishmaniasis is a major problem in Latin America but has been rarely reported from the Southwest of Iran [6] where all such cases have shown involvement of the oral and not the nasal mucosa. Mashhad located in the Northeast of Iran is endemic for cutaneous leishmaniasis mainly due to L. tropica and less commonly, L. major.[7] Mucosal involvement by these species is rare [8] and to the best of our knowledge, mucosal involvement has not been reported in this area so far. The reason why leishmaniasis patients develop mucosal involvement is not fully understood. It seems that parasite-related factors such as its invasiveness, tropism as well as the host immune response play a role. [9] It is also known that vessels of the anterior nasal septum provide favorable conditions for the development of amastigotes. [10] Some researchers also believe that lower temperatures in the nasal cavity make it more susceptible to parasites. [11]
Progression of the disease from skin to the nose appears to take place through lymphatic dissemination, the hematogenous route, and rarely by direct contact between mucosa and the cutaneous lesion. [10] Mucosal involvement in our case may have been the result of lymphatic and/or hematogenous spread, as the old scar of cutaneous leishmaniasis in the left oral commissure was on the same side as the nasal mass. L. tropica is capable of surviving in a latent state in previously affected tissues and may have spread after the cutaneous lesion healed. [12] Since mucosal involvement due to old world leishmaniasis is not frequent and the few reported cases concern immunocompromised patients, [5] we assessed our patient in this respect. He had no signs of immunodeficiency.
In spite of the prolonged course of treatment, the nasal localization of the lesion in our patient neither caused septum perforation nor was resistant to treatment, as described in other reports of cutaneous-mucosal forms of new-world leishmaniasis. Also, there has been no sign of recurrence in the nasal and other mucosal tissues or skin areas after 1 year of follow-up. This rare case of endonasal leishmaniasis caused by L.tropica suggests that a strict separation of different types of leishmaniasis and the species which cause them is not always possible or appropriate for diagnosis. Finally, we suggest that in endemic areas, leishmaniasis should be considered as a differential diagnosis for nasal or oral obstructive masses.
| 1. |
Aliaga L, Cobo F, Mediavilla JD, Bravo J, Osuna A, Amador JM, et al. Localized mucosal leishmaniasis due to Leishmania (leishmania) infantum: Clinical and microbiologic findings in 31 patients. Medicine (Baltimore) 2003;82:147-58.
[Google Scholar]
|
| 2. |
Naik SR, Vinayak VK, Talwar P, Sehgal S, Mehra YN, Dutta BN, et al. Visceral leishmaniasis masquerading as a nasopharyngeal tumour. Report of a case. Trans R Soc Trop Med Hyg 1978;72:43-5.
[Google Scholar]
|
| 3. |
Kharfi M, Fazaa B, Chaker E, Kamoun MR. Mucosal localization of leishmaniasis in Tunisia: 5 cases. Ann Dermatol Venereol 2003;130 (1 Pt 1):27-30.
[Google Scholar]
|
| 4. |
Benmously-Mlika R, Fenniche S, Kerkeni N, Aoun K, Khedim A, Mokhtar I. Primary Leishmania infantum MON-80 endonasal leishmaniasis in Tunisia. Ann Dermatol Venereol 2008;135:389-92.
[Google Scholar]
|
| 5. |
Layegh P, Rahsepar S, Rahsepar AA. Systemic meglumine antimoniate in acute cutaneous leishmaniasis: Children versus adults. Am J Trop Med Hyg 2011;84:539-42.
[Google Scholar]
|
| 6. |
Yaghobi R, Hoghooghi-Rad N. Lip leishmaniasis in the southwest of Iran during the last decade. Iran J Dermatol 1997;1:19-23.
[Google Scholar]
|
| 7. |
Shahbazi F, Shahabi S, Kazemi B, Mohebali M, Abadi AR, Zare Z. Evaluation of PCR assay in diagnosis and identification of cutaneous leishmaniasis: A comparison with the parasitological methods. Parasitol Res 2008;103:1159-62.
[Google Scholar]
|
| 8. |
Schewach-Millet M, Kahana M, Ronnen M, Yuzuk S. Mucosal involvement of cutaneous leishmaniasis. Int J Dermatol 1986;25:113-4.
[Google Scholar]
|
| 9. |
Carvalho EM, Barral-Netto M, Barral A, Brodskyn CI, Bacellar O. Immune regulation in leishmaniasis. J Braz Ass Adv Sci 1994;46:441-5.
[Google Scholar]
|
| 10. |
Lessa MM, Lessa HA, Castro TW, Oliveira A, Scherifer A, Machado P, et al. Mucosal leishmaniasis: Epidemiological and clinical aspects. Braz J Otorhinolaryngol 2007;73:843-7.
[Google Scholar]
|
| 11. |
Scott P. Impaired macrophage leishmanicidal activity at cutaneous temperature. Parasite Immunol 1985;7:277-88.
[Google Scholar]
|
| 12. |
Magill AJ, Grögl M, Gasser RA Jr, Sun W, Oster CN. Visceral infection caused by Leishmania tropica in veterans of Operation Desert Storm. N Engl J Med 1993;328:1383-7.
[Google Scholar]
|
Fulltext Views
3,333
PDF downloads
1,867





