Translate this page into:
Oleogranulomas of the breast treated with hydroxychloroquine
2 Department of General Surgery, Taksim Training and Research Hospital, Istanbul, Turkey
Correspondence Address:
Ilteris Oguz Topal
Department of Dermatology, Okmeydani Training and Research Hospital, Istanbul
Turkey
| How to cite this article: Topal IO, Kocaturk E, Duman H, Topal Y. Oleogranulomas of the breast treated with hydroxychloroquine. Indian J Dermatol Venereol Leprol 2016;82:545-547 |
Sir,
An oleogranuloma is a foreign body granuloma that results from the injection of an oily substance into the skin or subcutaneous tissue. [1]
A 44-year-old man presented to the department of dermatology with indurated, purulent draining nodules on both the breasts since 4 years. Past medical history was non-contributory. He had been previously admitted in the department of general surgery where drainage of the breast abscesses was performed but was followed by recurrence. He denied any history of trauma or injection into the involved areas.
Dermatological examination revealed multiple, erythematous indurated nodules on both breasts extending to the thoracic wall. Several nodules exuding purulent material through sinus tracts were observed [Figure - 1]a. Diffuse sclerosis was evident in the thorax and abdomen. No palpable axillary lymph nodes were found.
 |
| Figure 1: (a) Multiple, erythematous and indurated draining nodules on both breasts and thoracic wall. (b) Significant improvement of the lesions after 2 months of therapy with hydroxychloroquine |
Laboratory tests revealed elevation in the levels of aspartate aminotransferase (68 U/L), alanine transaminase (38 U/L), alkaline phosphatase (255 U/L), lactate dehydrogenase (342 U/L), gamma glutamyl transferase (165 U/L) and C-reactive protein (20.3 mg/L). He also had anemia (hemoglobin: 9.5 g/dL) and a red blood cell count of 3.45 × 106/µL. Serological tests for human immunodeficiency virus and hepatitis virus B and C were negative.
Chest X-ray revealed small pleural effusions. Contrast-enhanced computed tomography of the chest showed extensive edema and soft tissue swelling in the anterior chest wall. The differential diagnoses considered at this point were idiopathic granulomatous mastitis, tuberculous mastitis and malignancy.
Smears and cultures of the purulent exudates and tissue biopsy material were negative for bacteria, fungi and acid-fast microorganisms. The tuberculin skin test and polymerase chain reaction for Mycobacterium tuberculosis were negative.
An incisional biopsy was performed from the breast nodule. Which revealed multiple cystic spaces in the dermis surrounded by foamy histiocytes, giant cells of the foreign body and Langhans types, mixed inflammatory cells and small calcifications [Figure - 2]. Areas of hemosiderin deposition were also noted. The cystic spaces contained an unstained bubbly material that did not exhibit birefringence on polarized light microscopy. These histological features were consistent with a foreign body reaction, probably attributable to the injection of an exogenous fluid. Further examination revealed no evidence of malignancy or tuberculosis. We considered that the etiology of the condition might be exogenous. Eventually, after several long hospital stays, the patient admitted that his transgender friends had injected sunflower oil into his breasts.
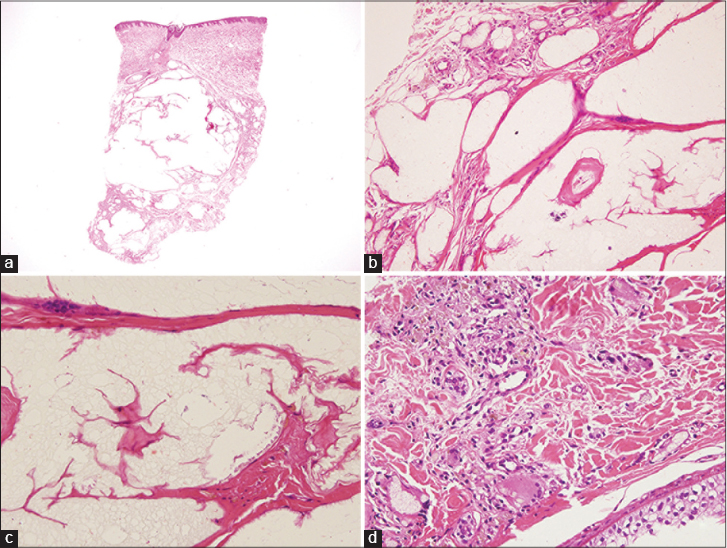 |
| Figure 2: (a) Panoramic view of the punch biopsy. Clear spaces seen largely in the dermal and subcutaneous tissue (H and E, ×20). (b) Close-up from the middle level-left edge. Surrounding the clear spaces, foamy histiocytes, needle-shaped spaces and inflammatory cells are seen (H and E, ×200). (c) The material filling the clear spaces is visible and has a “bubbly” appearance. A foreign body type giant cell can be noticed on the septum (H and E, ×400). (d) Inflammatory infiltrate containing foamy histiocytes and a vacuolated giant cell. Hemosiderin deposits seen on the upper left (H and E, ×400) |
He was prescribed doxycycline 100 mg tablets twice daily for 2 weeks. No clinical improvement was noted. Therefore, after a review of literature, he was started on oral hydroxychloroquine (200 mg twice daily) following ophthalmological clearance. He responded well following this treatment; the purulent exudates rapidly reduced and the lesions resolved within 2 months [Figure - 1]b.
Injection of a wide variety of foreign materials including paraffin oil, petroleum jelly and silicone into the breasts has been reported in the literature.[1] Such substances may trigger tissue reactions and may result in the formation of foreign body granulomas. The etiology of an oleogranuloma is unclear although an immunological mechanism may be responsible. [2]
Two types of oleogranulomatous mastitis are known; suppurative and non-suppurative. Both types of mastitis are characterized by the presence of indurated, firm, painful discrete masses.[2] Differential diagnosis includes infectious disease, lupus vulgaris, atypical mycobacterial infection and malignancy. The history of injection of a foreign substance into the breast is the key to clinical diagnosis.[3] Surgical excision, allopurinol, imiquimod, minocycline, glucocorticoids and low-dose oral retinoids have been used to treat foreign body granulomas.[3],[4]
Hydroxychloroquine is an antimalarial agent with immunosuppressive and anti-inflammatory properties. Recently, antimalarials have been shown to inhibit receptors of toll-like receptor 9 family (TLR9). Inhibition of toll-like receptor 9 signaling by antigen-presenting cells that initiate immune reactions and inhibition of the production of various cytokines seem to prevent granuloma formation.[5]
In summary, various substances can trigger inflammatory and granulomatous reactions when injected into the skin. An oleogranuloma should be considered as a differential diagnosis when examining patients with chronic erythematous nodules on the breasts. We suggest that hydroxychloroquine may be a therapeutic option for this condition.
Acknowledgment
We thank Prof. Dr. Nesimi Büyükbabani for performing the histopathological examination and providing the photographs.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Rosen T, Chen M. Factitious disease of the breast of a male due to injection of liquid plastic. Int J Dermatol 2001;40:743-6.
[Google Scholar]
|
| 2. |
Chae IH, Cha ES, Lee JE, Cheong J, Sungh SH. Interstitial injection mammoplasty mimicking diffuse infiltrative disease in a male patient. J Korean Soc Radiol 2013;68:225-8.
[Google Scholar]
|
| 3. |
Rieder E, Desai S, Mundi JP, Boyd KP, Patel RR, Ramachandran S, et al. Granulomatous dermatitis related to silicone implant. Dermatol Online J 2013;19:20708.
[Google Scholar]
|
| 4. |
Babuna G, Buyukbabani N, Yazganoglu KD, Baykal C. Effective treatment with hydroxychloroquine in a case of annular elastolytic giant cell granuloma. Indian J Dermatol Venereol Leprol 2011;77:110-1.
[Google Scholar]
|
| 5. |
Kalia S, Dutz JP. New concepts in antimalarial use and mode of action in dermatology. Dermatol Ther 2007;20:160-74.
[Google Scholar]
|
Fulltext Views
3,319
PDF downloads
1,092





