Translate this page into:
Olmsted syndrome in three sisters in a family
2 Department of Dermatology, Hi-Tech Medical College and Hospital, Bhubaneswar, Odisha, India
Correspondence Address:
Manas Ranjan Puhan
Niki Skin Care, Ranihat, Cuttack - 753 001, Odisha
India
| How to cite this article: Mohanty P, Dash G, Mohapatra L, Puhan MR. Olmsted syndrome in three sisters in a family. Indian J Dermatol Venereol Leprol 2018;84:522 |
Sir,
Olmsted syndrome is a very rare genodermatosis characterized by mutilating palmoplantar keratoderma. Other relevant features include periorificial hyperkeratotic plaques with flexion deformities of the digits, leading to constriction or spontaneous amputation.[1] Till now, around 73 cases have been reported.[2] According to literature, males are predominantly affected and females are only rarely affected. Most of the cases are sporadic, though some familial cases, possibly due to autosomal dominant and X-linked dominant transmission have also been reported.[3] We herein report a family of three siblings, all females, having the features of Olmsted syndrome.
An 11-year-old girl presented with complaints of thickening and scaling of the skin of bilateral soles since 1 year of age, which gradually progressed to become painful, large hyperkeratotic plaques resulting in flexion deformities of the digits [Figure - 1]. Similar lesions appeared on the palms around the age of three and then gradually on the perioral, genital and perianal regions. She developed a constriction band on the right little toe at the age of 8 years, resulting in the loss of toe. All lesions were pruritic. She was born of a non-consanguineous marriage, at term, by normal vaginal delivery. Her general condition was good at birth. She had achieved normal developmental milestones. On examination, the built of the patient was poor with apparently normal intelligence. Diffuse, bilateral symmetrical and thickened hyperkeratotic plaques were present on the palms and soles. Yellowish keratotic lesions were also seen on the angles of the mouth [Figure - 2]. Hair, nail, teeth and mucosa were normal. Similar palmoplantar keratotic lesions were found in her two younger twin sisters, aged 6 years [Figure - 3]. Other family members including parents were normal. There was no history of hyperhidrosis. All routine investigations including serum zinc levels (to rule out acrodermatitis enteropathica) were normal. Potassium hydroxide mount and wet mount of the skin scrapings did not show the presence of any fungus or mites. Histopathologic study revealed marked hyperkeratosis and the presence of parakeratotic columns within the keratin layer [Figure - 4], consistent with palmoplantar keratoderma. The patient was treated with topical urea, lactic acid creams and combination creams of topical steroid with salicylic acid, which resulted in mild improvement of skin lesions followed by reappearance of similar lesions after stopping the treatment. The parents did not give consent for starting oral retinoids. The patient was then referred to plastic surgery department of SCB Medical College, Cuttack, for debulking followed by skin grafting [Figure - 5].
 |
| Figure 1: Painful, massive, hyperkeratotic plaques resulting in flexion deformities of digits and loss of toe |
 |
| Figure 2: Yellowish keratotic lesions on the angles of the mouth |
 |
| Figure 3: Palmoplantar keratotic lesions in all three sisters |
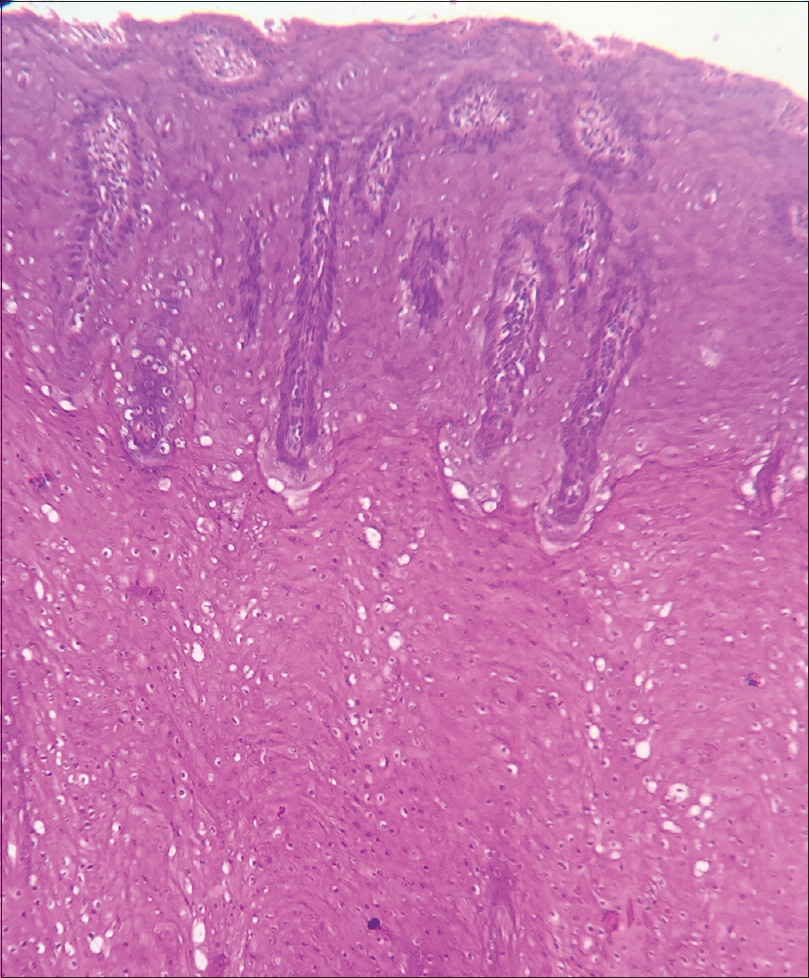 |
| Figure 4: Marked hyperkeratosis with parakeratotic columns in the keratinous layer (H and E, ×400) |
 |
| Figure 5: One month after debulking, followed by skin grafting |
H.C. Olmsted first described this syndrome in the year 1927 in a 5-year-old boy.[4] It is a rare congenital condition characterized by the development of periorificial keratotic plaques and bilateral palmoplantar transgradient keratoderma, which are the two characteristic signs that distinguishes it from other keratodermas including Mal de Meleda and Vohwinkel syndrome. It is usually seen in early childhood when the child starts to walk and grasp. Fissuring around the toes that heals with a constricting band of tissue, leading to autoamputation of the digits, has been reported. Keratotic papules around orifices develop later and then on the neck, axilla, cubital fossa, inguinal region and gluteal region. In long-standing cases, progression to squamous cell carcinoma and malignant melanoma has been reported. Atherton et al. in 1990, Cambiaghi et al. in 1995, Yaghoobi et al. in 2007 and Bukharia et al. in 2016 reported familial cases of the disease.[5] Our patient had symmetrical massive palmoplantar keratoderma without extension on to the dorsal hand, as well as some keratotic plaques on perioral, genital, perianal area and angle of mouth. She also had a history of constricting ring around right little toe (pseudoainhum) followed by the loss of the finger. Similar lesions were also found in her two twin sisters. There were no abnormalities of the nails, hair, oral mucosa, teeth or joints. All these findings were consistent with Olmsted syndrome.
There is no satisfactory treatment for this condition. Topical treatments offer only symptomatic relief of pain and fissuring by reducing the thickness of the keratotic palmoplantar skin lesions. Various topical agents have been tried with varying success. Systemic retinoids (acitretin 0.5 mg/kg) are purported to produce a significant improvement. Etretinate has been reported to result in partial improvement but is ineffective in arresting the progressive course. Debulking surgery followed by skin grafting has been tried in some patients with flexion contractures, but recurrence has been noted. In our case, the older sister has undergone debulking surgery followed by skin grafting and the same is planned in the other sisters too, followed by topical medication. The present case is reported due to the rare occurrence of the disease in all three sisters in a family, including the twins.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Kumar P, Sharma PK, Kar HK. Olmsted syndrome. Indian J Dermatol 2008;53:93-5.
[Google Scholar]
|
| 2. |
Duchatelet S, Hovnanian A. Olmsted syndrome: Clinical, molecular and therapeutic aspects. Orphanet J Rare Dis 2015;10:33.
[Google Scholar]
|
| 3. |
Yaghoobi R, Omidian M, Sina N, Abtahian SA, Panahi-Bazaz MR. Olmsted syndrome in an Iranian family: Report of two new cases. Arch Iran Med 2007;10:246-9.
[Google Scholar]
|
| 4. |
Tao J, Huang CZ, Yu NW, Wu Y, Liu YQ, Li Y, et al. Olmsted syndrome: A case report and review of literature. Int J Dermatol 2008;47:432-7.
[Google Scholar]
|
| 5. |
Bukharia A, Komal S, Sudhanan VM, Chaudhary SS. Olmsted syndrome: Rare occurrence in four siblings. Indian J Dermatol 2016;61:347.
[Google Scholar]
|
Fulltext Views
9,324
PDF downloads
2,316





