Translate this page into:
Onychomatricoma on the fourth toenail: A rare tumor in a rare localization
Corresponding author: Dr. Sofia Antunes-Duarte, Department of Dermatology, Hospital De Santa Maria, Floor 5, Avenida Prof. Egas Moniz, 1649-035 Lisbon, Portugal. sofia.duarte.a@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Antunes-Duarte S, Fraga A, Soares-de-Almeida L. Onychomatricoma on the fourth toenail: A rare tumor in a rare localization. Indian J Dermatol Venereol Leprol 2023;89:408-10.
Abstract
Onychomatricoma is a rare benign tumor of the nail matrix, characterized by finger-like projections that invade the nail plate. The fingernails of Caucasian women are most commonly affected. Because this tumor can easily mimic other more prevalent ungual diseases, it is crucial to be acquainted with its characteristic clinical and histopathologic features. The authors present a case of a 40-year-old man with an onychomatrichoma in the fourth left toenail, which was initially misdiagnosed and treated as onychomycosis.
Keywords
Nail disorders
nail tumors
onychomatrichoma
onychomycosis
Introduction
Onychomatricoma is a rare and benign tumor of the nail matrix.1 It predominantly affects the fingernails of Caucasian women during the fifth decade of life and typically is slow-growing and painless.2 Although onychomatricoma has a unique set of clinical and histopathologic features, its rarity and the lack of knowledge about this disease contribute to a frequent mistaken and late diagnosis. Herein, we report a case of a 40-year-old man with an onychomatricoma in an unusual localization, the fourth left toenail which was initially misdiagnosed and treated as onychomycosis.
Case Report
A 40-year-old Caucasian man presented to our outpatient department with a two-year history of asymptomatic discoloration and thickening of the fourth left toenail. He denied any previous local trauma. For the clinical suspicion of onychomycosis, he was treated by his primary care physician with a three-month regimen of oral terbinafine, and topical amorolfine for eight months, without improvement.
Dermatologic examination revealed a hypertrophic and dystrophic nail with longitudinal ridging, transverse and longitudinal over-curvature and brown-yellowish discoloration [Figures 1a and b]. Nail plate dermoscopy demonstrated white longitudinal grooves. All the other toenails and fingernails were unaffected.

- Onychomatricoma on the fourth toenail of the left foot showing a thickened, over-curved, ridged, brown-yellowed nail. Front view

- Onychomatricoma on the fourth toenail of the left foot showing a thickened, over-curved, ridged, brown-yellowed nail. Lateral view
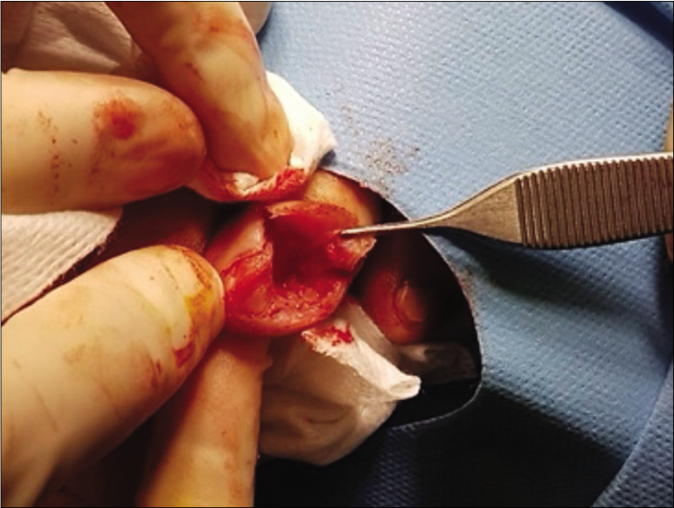
A clinical diagnosis of onychomatricoma was suspected, and we opted to perform an exploratory surgical procedure. A careful avulsion of the nail plate revealed a polypoid tumor with digitiform papillary projections emerging from the nail matrix [Figure 2a]. The ventral view of the extracted nail plate evidenced multiple parallel cavities [Figure 2b], fitting perfectly in the tumor surface. The tumor was completely excised [Figure 2c], and histopathological examination demonstrated a fibroepithelial neoplasm with filiform projections [Figure 3], corroborating onychomatricoma’s clinical diagnosis. Periodic acid-Schiff histochemical staining was negative for fungal organisms.

- Intraoperative photographs of onychomatricoma’s excision. Tumor view showing digitiform projections of the nail matrix

- Intraoperative photographs of onychomatricoma’s excision. Ventral face of the nail plate showing parallel cavities
- Intraoperative photographs of onychomatricoma’s excision. After complete resection of the tumor
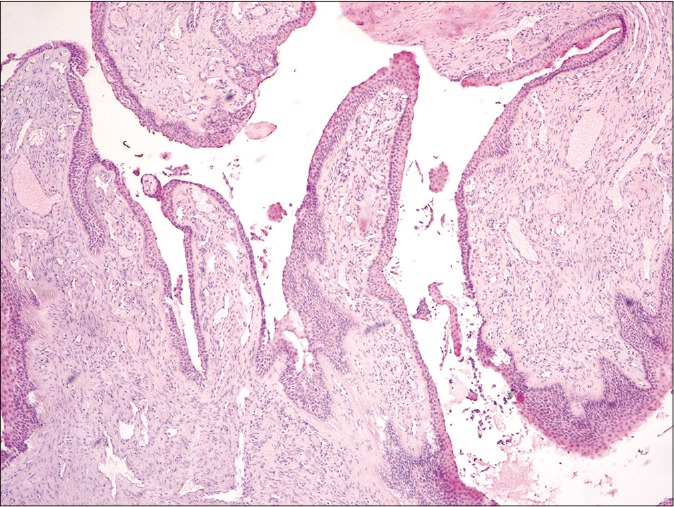
- Filiform projections lined by epithelium emerging from the nail matrix (H and E, ×40)
Discussion
Since the first description of onychomatricoma by Baran and Kint in 1992, fewer than 100 cases have been reported.1 Although etiology remains unknown, nail plate trauma and onychomycosis have been identified as possible predisposing factors of this tumor.3
Fingers are more commonly affected than toes with a prevalence of 64%.4 When the onychomatricoma reaches toenails, most cases are found in the big toe and sometimes in the second or the third toe. In 2015, Di Chiacchio et al. reported a large series of 30 onychomatricoma, where 11 cases were found on the toenails: seven in the big toenail, two in the second toe and two in the third toe.4 In 2016, Coutellier et al. were the first to describe an onychomatricoma on the fifth toe of the left foot in a 68-year-old female.5 We were unable to find any previous reports of onychomatricoma on the fourth toenail.
The classic tetrad signs of onychomatricoma include thickening of the nail plate, transverse or longitudinal over-curvature, xanthonychia and multiple splinter hemorrhages.6,7 Other possible presentations are nail dystrophy, erythronychia, melanonychia, plate fracture, paronychia and dorsal pterygium.7 The clinical diagnosis of onychomatricoma can be challenging because it can easily mimic many other nail tumors and diseases, including the most prevalent ungual disorder—onychomycosis.8 Consequently, onychomatricoma should be considered in the differential diagnosis of patients with onychomycosis-like changes failing to respond to proper antifungal treatment, as in this case. The index of suspicion should increase when a single dystrophic nail is involved. Notably, cases of onychomatricoma with concomitant onychomycosis can also occur, as the channels within the nail plate created in onychomatricoma provide a favorable environment for fungal invasion.6,8
Onychoscopy, nail clipping, ultrasound and confocal microscopy may aid in onychomatricoma’s diagnosis.7 Dermatoscopy criteria include longitudinal parallel white lines, parallel lesion edges, splinter hemorrhages, dark dots, nail pitting and thickening of the free edge.9 However, the gold standard diagnostic method is surgical biopsy with histopathological examination.7 Intraoperatively, a filamentous tumor with digitiform projections that penetrate the nail plate leading to woodworm-like cavities is usually found.10,11 Histopathological evaluation characteristically exhibits a fibroepithelial tumor composed of a proximal pedunculated base and a distal zone with multiple epithelial digitations.2,3 A biphasic fibrous stroma, superficially cellular and deeply collagenized and relatively hypocellular, is present throughout the tumor.2,3
The treatment of choice for onychomatricoma is complete surgical excision and is typically curative.10 Secondary ungual dystrophy and recurrences have been rarely reported.5,10
Conclusion
Onychomatricoma should be kept in mind in the differential diagnosis of nail apparatus changes to avoid misdiagnosis and proper treatment delay. The current case illustrates the importance of suspecting an underlying onychomatricoma toward a single long-standing distorted nail unresponsive to fungicidal treatment. It well highlights onychomatricoma’s described clinical and histopathological features and is of particular interest due to its unusual localization on the fourth toenail.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Onychomatrixoma. Filamentous tufted tumour in the matrix of a funnel-shaped nail: A new entity (report of three cases) Br J Dermatol. 1992;126:510-5.
- [CrossRef] [PubMed] [Google Scholar]
- Onychomatricoma: New clinical and histological eatures. A review of 19 tumors. Am J Dermatopathol. 2010;32:1-8.
- [CrossRef] [PubMed] [Google Scholar]
- Onychomatricoma: An infrequent nail tumor. Indian J Dermatol Venereol Leprol. 2012;78:382-3.
- [CrossRef] [PubMed] [Google Scholar]
- Onychomatricoma: Epidemiological and clinical findings in a large series of 30 cases. Br J Dermatol. 2015;173:1305-7.
- [CrossRef] [PubMed] [Google Scholar]
- Unusual localisation for onychomatricoma on the 5th toenail: A case report and review of the literature. Case Rep Dermatol Med. 2016;2016:1853495.
- [CrossRef] [PubMed] [Google Scholar]
- A case of veiled onychomatricoma. J Eur Acad Dermatol Venereol. 2019;33:e420-e2.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging technique for the diagnosis of onychomatricoma. J Eur Acad Dermatol Venereol. 2018;32:1874-8.
- [CrossRef] [PubMed] [Google Scholar]
- Onychomycosis and onychomatricoma. Skin Appendage Disord. 2016;1:209-12.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopic features of onychomatricoma: A study of 34 cases. Dermatology. 2015;231:177-83.
- [CrossRef] [PubMed] [Google Scholar]
- Onychomatricoma: A rare tumor of nail matrix. Ann Dermatol. 2016;28:237-41.
- [CrossRef] [PubMed] [Google Scholar]
- Onychomatricoma of the nail bed. Skin Appendage Disord. 2019;5:165-8.
- [CrossRef] [PubMed] [Google Scholar]






