Translate this page into:
Oral cutaneous fistula associated with intestinal Behçet’s disease and mucous membrane pemphigoid: A case report
Corresponding author: Prof. Meng Pan, Department of Dermatology, Shanghai Jiao Tong University Medical School Affiliated Ruijin Hospital, Shanghai. China. pm10633@rjh.com.cn
-
Received: ,
Accepted: ,
How to cite this article: Wu H, Wang J, Xu H, Zhao X, Li X, Pan M. Oral cutaneous fistula associated with intestinal Behçet’s disease and mucous membrane pemphigoid: A case report. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_111_2024
Dear Editor,
Behçet’s disease (BD) is an autoinflammatory syndrome characterised by recurrent oral and genital ulcers, uveitis, and skin lesions. Several autoimmune diseases, such as Sjögren’s syndrome, systemic lupus erythematosus, Graves’ disease, and Hashimoto’s thyroiditis, were reported to be associated with BD.1 Mucous membrane pemphigoid (MMP) is an autoimmune mucosal blistering disease characterised by a subepidermal split. To our knowledge, the concurrence of the two disorders has not been reported. Herein, we described a patient presenting with a disfiguring oral cutaneous fistula (OCF) and a severe irrecoverable mouth-opening limitation associated with both entities.
A 50-year-old Chinese woman with a 12-year history of recurrent oral ulcers presented with a painful OCF for a one-year duration. The OCF had developed from an inflamed nodule, which ulcerated and led to perforation. She had undergone a radical right hemicolectomy six years earlier for a large ileocecal ulcerative mass found on endoscopy. Physical examination showed a perioral elliptic fistula with inflamed borders on the right side [Figure 1a], cicatrices formation of the oral mucosa, and severe mouth-opening limitation [Figure 1b]. The right angle of her mouth, which comprised the anterior border of the fistula, got destroyed spontaneously and disappeared during hospitalization [Figure 1c]. She did not have any other cutaneous eruption, genital ulcer, or gastrointestinal symptoms. A specific ocular examination showed no abnormality. The pathergy test was negative. Odontogenic fistula was ruled out through a panoramic radiograph [Figure 2a], and confirmed by maxillofacial magnetic resonance imaging and contrast-enhanced computed tomography (CT). The CT enterography revealed a volcano-like deep ulcer at the anastomotic site [Figure 2b]. The malignancy screening was negative. A mucosal biopsy taken from the labial mucosa showed ulcer formation with acute and chronic inflammatory cells, and focal hyperplasia of granulation and fibrous tissues. Immunological findings in serum by enzyme-linked immunosorbent assay showed positive anti-BP180 IgG [12 U/mL, normal range (NR) < 9], anti-BP180 IgA [15 U/mL, NR < 8], anti-laminin 332 IgG [46 U/mL, NR < 11] and anti-integrin β4 IgG [101 U/mL, NR < 14] autoantibodies. And the indirect immunofluorescence on the salt-split skin showed positive with linear roof-bounded IgG [Figure 2c]. Eventually, the diagnosis of intestinal BD and MMP was established based on the diagnostic criteria proposed by Cheon et al.2 and the presence of cicatrices formation, along with supporting evidence from serologic findings, respectively. The patient was treated with prednisone 20 mg/day and methotrexate 10 mg/week. The painful ulcer and inflammatory lesions were controlled within 10 days [Figure 3a]. The dose of prednisone was tapered gradually after 2 months. The patient presented with a persistent stable disease until the last follow-up 2 years later [Figure 3b], though the limitation of mouth-opening had no improvement.

- A perioral elliptic fistula with inflamed borders on the right side.
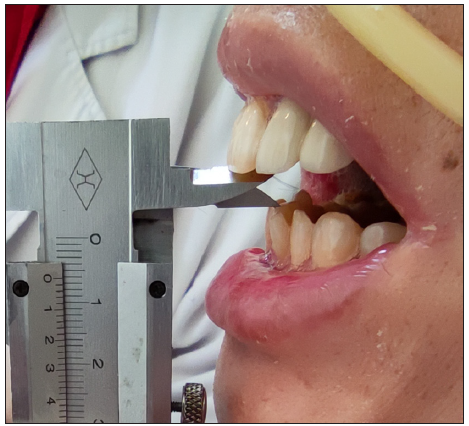
- Mouth opening was severely limited and the distance between upper and lower central incisors was 6 mm.

- Spontaneous destruction of the right angle of mouth.
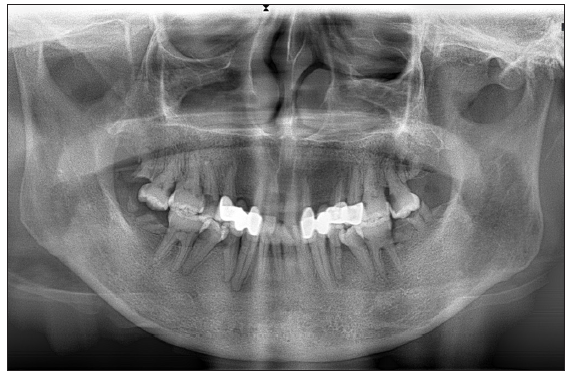
- No evidence of an odontogenic fistula on panoramic radiograph.
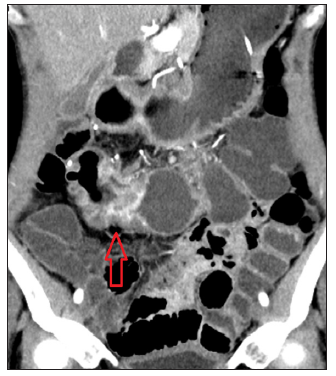
- Computed tomography enterography revealed a volcano-like ulcer in the anastomosis region (red arrow).
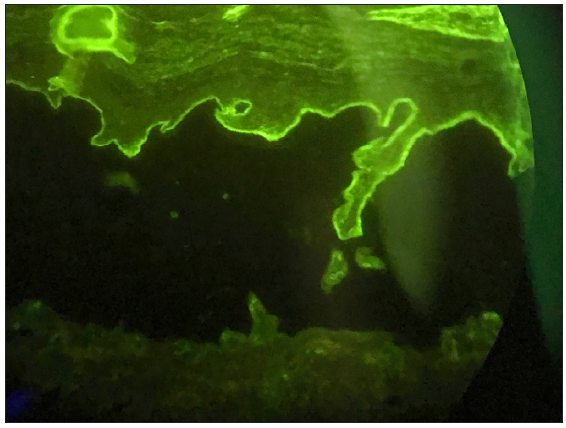
- Indirect immunofluorescence on the salt-split skin showed positive with linear roof-bounded IgG (200x).

- Transformation of the fistula following therapy: The inflammation was controlled within 10 days after the initiation of therapy.

- Transformation of the fistula following therapy: The condition remained stable until the last follow-up in 2 years.
OCF is a pathologic path connecting the oral cavity and cutaneous surface and is most often odontogenic.3 As far as we know, it has not been described in either BD or MMP. Cicatrices in oral mucosa, which resulted in severe mouth-opening limitation, could be seen in both disorders.4,5
The possibility of intestinal BD or Crohn’s disease (CD) was considered in light of the patient’s chronic oral and intestinal inflammation. BD is an idiopathic vasculitis that affects multiple systems, and the intestinal involvement features large, round/oval-shaped, deep ulcers in the ileocecal region.6 CD is a chronic inflammatory disease that can affect any part of the gastrointestinal tract, from the mouth to the anus. The inflammation is typically segmental, asymmetrical, and transmural, hallmarked as ‘skip lesions’, a ‘cobblestone’ appearance.7 The presentations of the two diseases can be similar, and there is currently no gold-standard diagnostic method for them. Cheon et al. had developed novel diagnostic criteria for intestinal BD based on colonoscopic features and clinical manifestations.2 Their findings demonstrated that patients exhibiting typical intestinal ulcers (< 5 ulcers, oval in shape, deep, with discrete borders, located in the ileocecal area) and oral ulcers can be diagnosed with probable intestinal BD. Moreover, the decision to exclude CD in our patient was made following a consultation with an experienced gastroenterologist, given the absence of characteristic features in the clinical presentation, histology, and radiology.
We suspect that both the autoinflammatory process involved in BD and the autoantibody-mediated mucosal damage in MMP contributed to such disfiguring lesions, although further research is needed. Certainly, due to the rarity of this situation, regular follow-up to monitor the disease is ongoing.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
This work received funding from the National Natural Science Foundation of China (82173407).
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that they have used artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript or image creations.
References
- Coexistence of behcet’s disease and autoimmune disease: Clinical features of 11 cases. J Dermatol. 2005;32:614-6.
- [CrossRef] [PubMed] [Google Scholar]
- Development and validation of novel diagnostic criteria for intestinal Behcet’s disease in Korean patients with ileocolonic ulcers. Am J Gastroenterol. 2009;104:2492-9.
- [CrossRef] [PubMed] [Google Scholar]
- Odontogenic cutaneous fistula: A cause of persistent cervical discharge. Case Rep Med.. 2018;2018:3710857.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Extensive oral scarring and bilateral subclavian artery stenosis in pediatric-onset behcet’s disease. J Clin Rheumatol. 2020;26:e91-e2.
- [CrossRef] [PubMed] [Google Scholar]
- Gastrointestinal behcet’s disease: A review. World J Gastroenterol. 2015;21:3801-12.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Typical endoscopic findings and diagnostic criteria for crohn’s disease. In: Hibi T, Hisamatsu T, Kobayashi T, eds. Advances in endoscopy in inflammatory bowel disease. Tokyo: Springer Japan; 2018. p. :77-83.
- [Google Scholar]





