Translate this page into:
Oral involvement in disseminated superficial porokeratosis
Correspondence Address:
Neena Khanna
Department of Dermatology and Venereology, Room No. 4073, Teaching Block, All India Institute of Medical Sciences, Ansari Nagar, New Delhi - 110 029
India
| How to cite this article: Bhatia R, Gupta V, Khanna N. Oral involvement in disseminated superficial porokeratosis. Indian J Dermatol Venereol Leprol 2017;83:244-246 |
Sir,
Porokeratosis is a clonal disorder of keratinization that clinically manifests as centrifugally expanding, annular plaque(s) with a thready, ridge-like margin (often with a furrow), which histopathologically shows pathognomonic cornoid lamella.[1],[2] We report a clinically typical lesion of porokeratosis in the buccal mucosa of a patient with disseminated superficial porokeratosis.
A 26-year-old man presented with complaints of multiple, asymptomatic lesions involving the face, trunk, extremities and scrotum for 8 years. Individual lesions began as small papules gradually increasing to form small, annular, barely palpable plaques. There was no change in the lesion on sun exposure and no oral symptoms. His brother and maternal uncle also had similar lesions. There was no history suggestive of immunosuppression.
On examination, the face, extensor surfaces of upper and lower extremities, trunk, scrotum, proximal nail fold of the right fourth toe and left heel revealed multiple papules and plaques ranging from 0.5 to 2 cm in diameter [Figure 1a] , [Figure 1b], [Figure 1c]. All the lesions were annular with a thready margin; a furrow was not discernable in most of the lesions and no central atrophy was observed. Oral examination revealed a similar solitary, annular plaque of about 2 cm × 1.5 cm with a thready, white, elevated margin on the left buccal mucosa [Figure 1d]. The centre of the oral lesion was paler than the surrounding mucosa.
 |
| Figure 1a: Annular plaques with thready margin on abdomen |
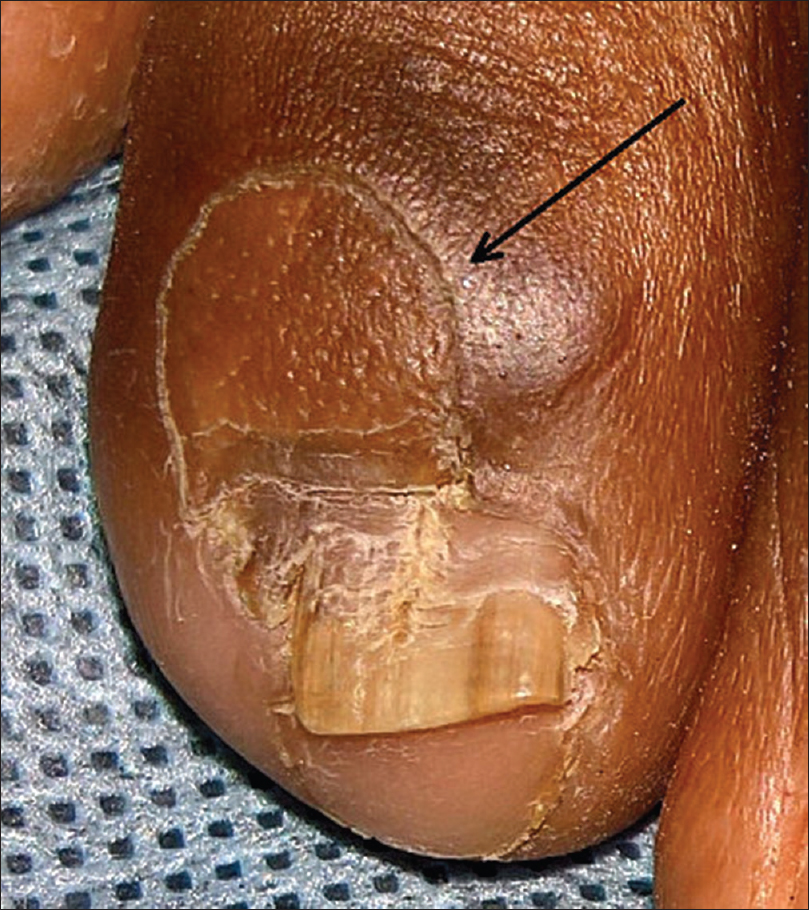 |
| Figure 1b: Annular plaque on the right fourth toe, extending on the proximal nail fold and nail plate |
 |
| Figure 1c: Annular plaque with thready margin on the left heel |
 |
| Figure 1d: Involvement of left buccal mucosa with a similar annular plaque with serpiginous thready margin and paler center than surrounding mucosa |
Biopsy from the annular lesion on the arm showed features of porokeratosis with a focal column of parakeratotic stratum corneum invaginating the epidermis, with lymphocytic exocytosis and a lympho-histiocytic infiltrate in the underlying upper dermis [Figure 2a] and [Figure 2b]. The patient refused biopsy from the oral lesion. Serology for human immunodeficiency virus was non-reactive.
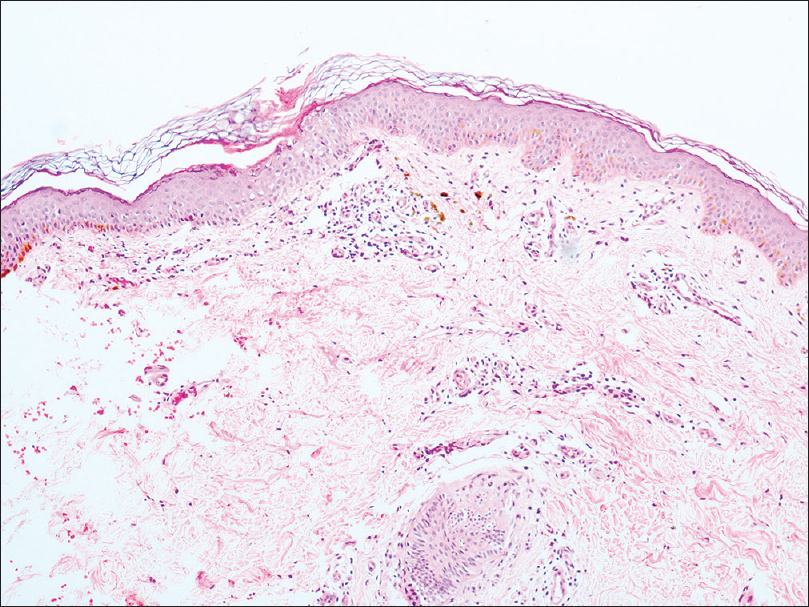 |
| Figure 2a: Skin biopsy showing focal invagination of epidermis by a column of stratum corneum (H and E, ×100) |
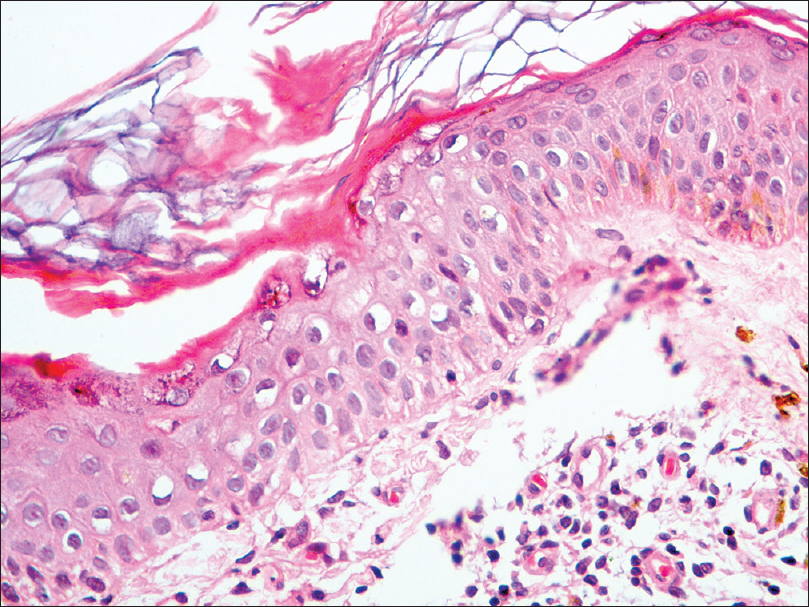 |
| Figure 2b: Invagination of epidermis by a parakeratotic column (cornoid lamella), lymphocytic exocytosis and underlying focal upper dermal infiltration of lymphocytes and histiocytes (H and E, ×400) |
Porokeratosis is a genetic disorder that manifests clinically as annular plaques with a thready elevated border, often with a furrow. Depending on the location, size and distribution of lesions, several clinical variants including and porokeratosis of Mibelli, punctate porokeratosis, porokeratosis palmaris plantaris et disseminata linear porokeratosis disseminated superficial porokeratosis and its actinic variant are described. All these variants are unified histologically by the presence of a parakeratotic column (cornoid lamella) invaginating the epidermis.[1] Disseminated superficial porokeratosis and its actinic variant are the most common types of porokeratosis with the former characterized by the involvement of both sun-protected (trunk, genitals, palms and soles) and sun-exposed areas of the body and the latter by occurrence of lesions predominantly on sun-exposed sites.[1] Unlike the actinic variant which usually occurs in the third decade of life, disseminated superficial porokeratosis occurs more often in children and immunocompromised patients.[1] Our patient had a later onset and there was no evidence of immunosuppression.
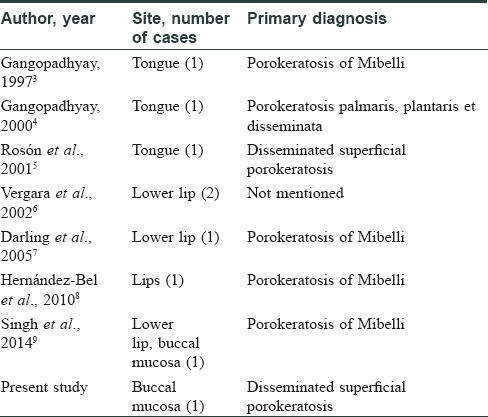
Oral involvement in porokeratosis is extremely uncommon. Of all the variants, it is seen most frequently in porokeratosis of Mibelli in which it has been reported to occur more commonly on the lips and tongue while involvement of buccal mucosa is decidedly rare [Table - 1]. It has also been reported in porokeratosis palmaris, plantaris et disseminata.[10] There is a prior report of oral lesions in a patient with disseminated superficial porokeratosis.[5] This patient had a solitary plaque on the dorsum of the tongue, in addition to multiple small annular plaques in a generalized distribution, including lesions on the scrotum and penis [Table - 1].[5] Our patient also had similar involvement of the trunk, upper and lower limbs, and scrotum. The skin lesions were morphologically like disseminated superficial porokeratosis and the diagnosis was confirmed histologically. Although we could not biopsy the buccal lesion, the morphology of the lesion (annular plaque with a thready elevated margin) was strikingly similar to that on the skin.
Acknowledgment
We are grateful to Prof. M. Ramam, Department of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi, for his help in histopathological diagnosis and providing the photomicrographs.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Sertznig P, von Felbert V, Megahed M. Porokeratosis: Present concepts. J Eur Acad Dermatol Venereol 2012;26:404-12.
[Google Scholar]
|
| 2. |
Schamroth JM, Zlotogorski A, Gilead L. Porokeratosis of mibelli. Overview and review of the literature. Acta Derm Venereol 1997;77:207-13.
[Google Scholar]
|
| 3. |
Gangopadhyay AK. Porokeratosis of mibelli with a mucous membrane lesion. Indian J Dermatol Venereol Leprol 1997;63:53-4.
[Google Scholar]
|
| 4. |
Gangopadhyay AK. Porokeratosis palmaris, plantaris et disseminata with a mucous membrane lesion. Indian J Dermatol Venereol Leprol 2000;66:205-6.
[Google Scholar]
|
| 5. |
Rosón E, García-Doval I, De La Torre C, Losada A, Rodríguez T, Ocampo C, et al. Disseminated superficial porokeratosis with mucosal involvement. Acta Derm Venereol 2001;81:64-5.
[Google Scholar]
|
| 6. |
Vergara G, Bañuls J, Botella R, Silvestre JF, Belinchón I, Betlloch I. Porokeratosis of the lower lip. Eur J Dermatol 2002;12:500-2.
[Google Scholar]
|
| 7. |
Darling MJ, Lambiase MC, Viernes J. Porokeratosis: A solitary oral lesion. J Drugs Dermatol 2005;4:89-91.
[Google Scholar]
|
| 8. |
Hernández-Bel P, Sanmartín-Jimenez O, Sorni-Bröker G, Guillén-Barona C. Labial porokeratosis. Am J Dermatopathol 2010;32:638.
[Google Scholar]
|
| 9. |
Singh N, Chandrashekar L, Kumar N, Kar R, Thappa DM. Classic porokeratosis of mibelli. Indian Dermatol Online J 2014;5 Suppl 2:S130-1.
[Google Scholar]
|
| 10. |
Requena L, Requena C, Cockerell CJ. Benign epidermal tumors and proliferations. In: Bolognia JL, Jorizzo JL, Schaffer JV, editors. Bolognia, Dermatology. 3rd ed. Philadelphia, PA: Elsevier Saunders; 2012. p. 1801-3.
[Google Scholar]
|
Fulltext Views
3,999
PDF downloads
3,175





