Translate this page into:
Oral magnesium chloride: A novel approach in the management of Hailey–Hailey disease
Correspondence Address:
Nitin G Barde
Department of Skin and VD, Indira Gandhi Government Medical College, C.A. Road, Nagpur - 440 018, Maharashtra
India
| How to cite this article: Barde NG, Mishra DB, Ingole SO. Oral magnesium chloride: A novel approach in the management of Hailey–Hailey disease. Indian J Dermatol Venereol Leprol 2017;83:259-262 |
Sir,
Familial benign chronic pemphigus or Hailey–Hailey disease is a rare autosomal dominant acantholytic disorder clinically characterized by flaccid bullae and erosions in the intertriginous areas, mainly the axillary and inguinal region. We report the unexpected, dramatic and persistent clinical improvement in long-standing cases of Hailey–Hailey disease, with daily intake of a solution containing magnesium chloride.
Case 1: A 34-year-old woman presented with macerated fissured plaques in the axilla and the groin, bilaterally, for 3–4 years with increased severity for the past 2–3 months. She also had a few crusted lesions in the angle of the mouth for 2 months. The cutaneous lesions started as tiny flaccid vesicles on an erythematous base, which ruptured easily and had a tendency to spread peripherally, producing a circinate plaque with crusting and fissures. These lesions were associated with burning sensation and malodor. There were multiple episodes of exacerbation of these lesions, especially in summer. Her mother and brother suffered from similar lesions. The patient had been treated in the past with various oral and topical antibiotics and antifungals, with no response. The general physical examination of the patient revealed erythematous, macerated plaques with multiple fissures and crusts in the axillary and inguinal areas and slight crusting near the angle of mouth [Figure - 1] and [Figure - 2]. Other areas of the skin, mucosal surfaces and nails were normal. All the routine hematological and biochemical investigations were normal. A potassium hydroxide smear for fungal elements was negative, whereas Tzanck smear showed some acantholytic cells. Biopsy taken from the axilla demonstrated intraepidermal acantholysis resulting in a dilapidated brick wall appearance [Figure - 3]. Direct immunofluorescence testing was not done. The final diagnosis of Hailey–Hailey disease was made on the basis of history, clinical and histopathological features. The patient was treated with 70 ml of oral magnesium chloride solution containing approximately 300 mg of elemental magnesium, which was prepared by dissolving 33 g of magnesium chloride in 1 L of distilled water. The magnesium solution was taken before breakfast every day. Clotrimazole dusting powder and fusidic acid cream were continued. A significant improvement in the skin lesions was noted after 15 days of treatment and an almost complete remission of signs and symptoms was obtained after 4 weeks [Figure - 4] and [Figure - 5]. No side effects were reported by the patient, except for the unpleasant taste of the solution. The patient's quality of life significantly improved. The pre- and post-treatment serum levels of electrolytes, in particular, calcium, magnesium and zinc, were within normal limits. The patient is still on treatment for 4 months, with sustained remission. We plan to continue the magnesium chloride solution for 6 months and then taper the dose.
 |
| Figure 1: Macerated plaque with painful fissures of the axilla |
 |
| Figure 2: Macerated plaque with painful fissures of the groin |
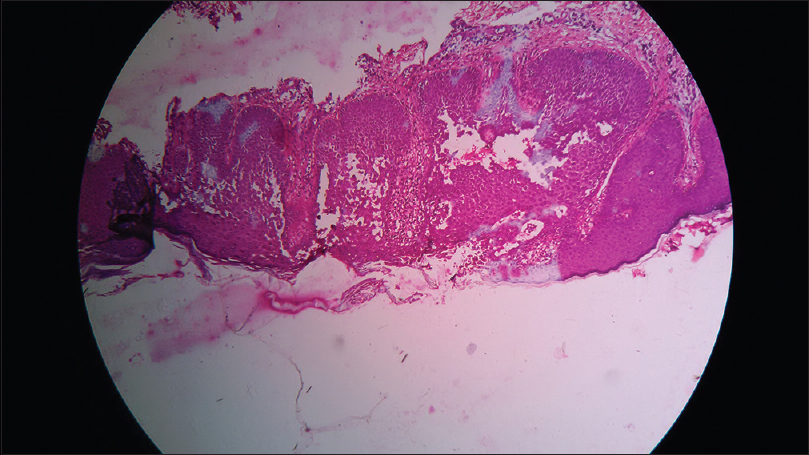 |
| Figure 3: Characteristic intraepidermal separation with dilapidated brick wall appearance (H and E, ×400) |
 |
| Figure 4: Clearing of maceration at the end of a month in the axilla |
 |
| Figure 5: Clearing of maceration at the end of a month's treatment in the groins |
Case 2: The 40-year-old brother of the first patient presented with multiple erosions developing on and off in both axillae for 9 years, with itching and burning sensation [Figure - 6]. No other flexural areas were involved. He was taking oral dapsone 100 mg along with topical steroid and antifungal creams for 6 months, with no relief. He was also investigated with a skin biopsy, potassium hydroxide and Tzanck smear. The skin biopsy obtained was consistent with Hailey–Hailey disease. All the routine hematological and biochemical investigations were within normal limits.
 |
| Figure 6: Fissuring with erythema in the axilla of the second patient |
He was also treated with 70 ml oral magnesium chloride solution after stopping dapsone and the steroid cream. He responded well within 15 days, with almost complete healing of erosions and did not complain of any adverse effect of magnesium chloride solution. His biochemical parameters after 1 month were within normal limits. The patient is still continuing treatment without any relapse [Figure - 7].
 |
| Figure 7: Healing of fissure with postinflammatory hyperpigmentation in the axilla of the second patient |
Hailey–Hailey disease is inherited as an autosomal dominant trait with incomplete penetrance. A positive family history is obtained in about two-thirds of patients. The disease, which typically occurs between the second and fourth decades of life, usually around puberty, has a chronic fluctuating course with remissions and relapses triggered by friction, stress, sweating, heat, moisture, superinfection, ultraviolet radiation or tissue damage. The fingernail alterations, when present are highly typical, while mucosal involvement, including the vulvovaginal area, is rare but possible.
The genetics and pathophysiology of Hailey–Hailey disease have been linked to about 100 mutations in the ATP2C1 gene, encoding for the Golgi secretory pathway Ca 2+/Mn 2+-ATPase protein 1.[1]
The Ca 2+/Mn 2+-ATPase protein 1 transports Ca 2+ and Mn 2+ and it sequesters Ca 2+ within the Golgi lumen. The human keratinocytes depend solely on this pump for loading the Golgi stores with Ca 2+. It plays a crucial role in setting up the cytosolic Ca 2+ oscillations known to control many vital cell functions, through cycles of release and re-uptake of internal Ca 2+ stores. The defective Ca 2+/Mn 2+-ATPase protein 1 affects the processing of desmosomal components, leading to the loss of cell–cell adhesion and consequent acantholysis. 2,3 Hence, the main mechanism of acantholysis is due to ATP2C1 mutation which leads to depletion of Ca + in Golgi lumen, which results in impaired processing and reduced concentration of junctional protein, finally leading to acantholysis. Borghi et al. first noted improvement in Hailey–Hailey disease with the use of oral magnesium chloride in a patient who was taking it for arthritis, as suggested by her close friend.[4] The role of Ca 2+ in the disease development is well documented. It regulates the proliferation and the differentiation of keratinocytes as well as the assembly of desmosomes. The Ca 2+-ATPases are key actors in the regulation of Ca 2+ in eukaryotic cells. They comprise three families of phosphorylation-type that contribute to the correct functioning of cell machinery namely: plasma-membrane Ca 2+-ATPases that extrude Ca 2+ out of the cell, and sarcoendoplasmic reticulum Ca 2+-ATPases, and secretory pathway Ca 2+/Mn 2+-ATPase that pump Ca 2+ into the lumen of intracellular stores.[5] The energy required for all Ca 2+ pumps are derived from adenosine triphosphate by catalyzing hydrolysis in two Mg 2+-dependent steps. The Mg 2+ ion regulates the activity of plasma membrane Ca 2+-ATPase, wherein high intracellular Mg 2+ concentration (>2 mM) plays an inhibitory role in human red blood cells.[6] Hence, magnesium supplementation reduces the extrusion rate of Ca 2+ and increases intracellular Ca 2+ sequestration. The intracellular calcium to magnesium ratio varies from 4:1 to 1:1 (calcium/magnesium). The efficiency of magnesium absorption varies inversely with the quantity of magnesium intake. The magnesium is absorbed into the body primarily from the ileum of the small intestine. The recommended dietary intake of magnesium is between 360 and 410 mg a day. Excessive magnesium intake does not usually cause toxicity because the body eliminates the excess amounts. The side effects of excess magnesium intake are nausea, diarrhea, loss of appetite and rarely, change in mental status. The lethal dose of magnesium chloride (LD50) given intravenously is 176 mg/kg in rats.[7]
Treatment with magnesium chloride results in a change in the intracellular calcium hemostasis which may be the molecular basis for the therapeutic response in Hailey–Hailey disease. Wider studies are warranted to assess the consistent efficacy and safety and molecular studies are required to establish the complete mechanism of action of magnesium chloride in this disease.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Szigeti R, Kellermayer R. Autosomal-dominant calcium ATPase disorders. J Invest Dermatol 2006;126:2370-6.
[Google Scholar]
|
| 2. |
Sudbrak R, Brown J, Dobson-Stone C, Carter S, Ramser J, White J, et al. Hailey-Hailey disease is caused by mutations in ATP2C1 encoding a novel Ca(2) pump. Hum Mol Genet 2000;9:1131-40.
[Google Scholar]
|
| 3. |
Desai BV, Harmon RM, Green KJ. Desmosomes at a glance. J Cell Sci 2009;122(Pt 24):4401-7.
[Google Scholar]
|
| 4. |
Borghi A, Rimessi A, Minghetti S, Corazza M, Pinton P, Virgili A. Efficacy of magnesium chloride in the treatment of Hailey-Hailey disease: From serendipity to evidence of its effect on intracellular Ca(2) homeostasis. Int J Dermatol 2015;54:543-8.
[Google Scholar]
|
| 5. |
Brini M, Carafoli E. Calcium pumps in health and disease. Physiol Rev 2009;89:1341-78.
[Google Scholar]
|
| 6. |
Schatzmann HJ, Vincenzi FF. Calcium movements across the membrane of human red cells. J Physiol 1969;201:369-95.
[Google Scholar]
|
| 7. |
Durlach J, Guiet-Bara A, Pagès N, Bac P, Bara M. Magnesium chloride or magnesium sulfate: A genuine question. Magnes Res 2005;18:187-92.
[Google Scholar]
|
Fulltext Views
7,703
PDF downloads
2,790





