Translate this page into:
Painful ulcer of the pinna in an immunocompromised patient
2 Department of Pathology, Hospital Regional Universitario de Málaga, Malaga, Spain
3 Department of Infectious Disease, Hospital Regional Universitario de Málaga, Malaga, Spain
Correspondence Address:
E Gómez Moyano
Plaza Hospital Civil, 29009 Malaga
Spain
| How to cite this article: Moyano E G, Blanca M A, Oñate F J, Pilar L M. Painful ulcer of the pinna in an immunocompromised patient. Indian J Dermatol Venereol Leprol 2018;84:369-372 |
A 35-year-old man living in Malaga, South of Spain, with Crohn's disease presented with a 1 year old history of a painful cutaneous lesion on his right ear and dysacusis [Figure - 1]a. He had applied topical corticosteroids and antibiotics without response. He was being treated for Crohn's disease with mesalazine, adalimumab and azathioprine. The general examination was within normal limits. On physical examination, we observed an erythematous–edematous, ulcerated plaque with superficial desquamation on his right ear with purulent discharge. Otoscopy showed a stenosis of the ear canal without involvement of the tympanic membrane. No regional lymphadenopathy was recorded. Skin biopsy was taken at the margins of the lesion [Figure - 2].
 |
| Figure 1 |
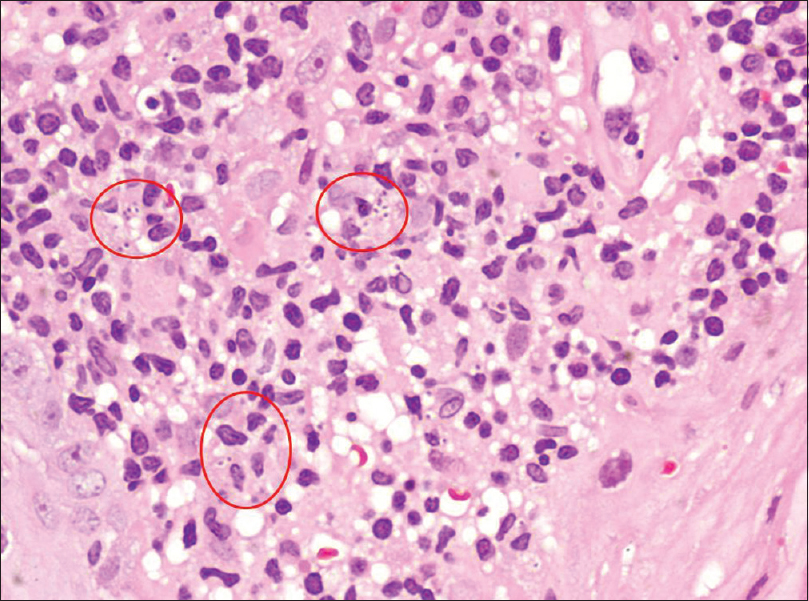 |
| Figure 2: Skin biopsy showing intracellular amastigote forms of Leishmania sp (H and E, ×200) |
Question
What is your diagnosis?
Answer
Cutaneous leishmaniasis.
Discussion
Skin biopsy demonstrated the presence of dense infiltrate in the whole dermis, consisting mainly of histiocytes, lymphocytes and plasma cells. Several intracellular, oval, small amastigotes were noted [Figure - 2]. Polymerase chain reaction analysis identified Leishmania donovani. All laboratory blood tests were within normal ranges and serology for human immunodeficiency virus, hepatitis B virus, hepatitis C virus and syphilis was negative. Leishmania antigen was not detected in urine. No visceral enlargement was noted on ultrasonography of the abdomen. The patient had no evidence of systemic involvement.
With the diagnosis of cutaneous leishmaniasis, treatment was started with liposomal amphotericin B at doses of 4 mg/kg/day during first 7 days and followed by 4 mg/kg/week for 1 month with complete resolution of the lesion at the end of treatment and recovery of hearing loss [Figure - 1]b.
Leishmaniasis comprises a group of diseases caused by a protozoan parasite belonging to the genus Leishmania and transmitted by the bite of infected female sand flies.[1]
The incidence of leishmaniasis as an opportunistic disease has increased because of the growing number of patients with immune suppression secondary to chronic illness, neoplasm, transplant and human immunodeficiency virus infection, thereby constituting a public health problem.[1] Some authors argue that cutaneous leishmaniasis is a “great imitator” of other conditions.[2] The ear is an exceptional location of cutaneous leishmaniasis in the Mediterranean area, while it is more common in Mexico, where it is known as “chiclero's ear.”[3] Chiclero's ear is usually caused by Leishmania mexicana and less frequently by Leishmania braziliensis. However, in our patient, L. donovani was the causative organism
This variety of cutaneous leishmaniasis is common among lumberjacks (chicleros) involved in collecting rubber, from which they extract the “chicle” latex used to produce chewing gum, characterized clinically by an ulcer, especially on the ear lobe, that can last for years and cause scarring and deformities.[4]
Other clinical presentations include edema and diffuse hyperemia of the external ear, erythematous and ulcerated areas on the helix, the antihelix or the external auditory canal without involvement of the tympanic membrane, intense pruritus and painful swelling of the involved areas.[5],[6],[7] However, atypical cases can result in a misdiagnosis, even in endemic regions.
Mucocutaneous disease is due to extension of local skin disease into the mucosal tissue through direct extension, hematogenous or lymphatic spread from cutaneous lesions. The species mainly responsible for the mucosal form of the disease are L. braziliensis, panamensis and amazoniensis in the New World and Leishmania infantum, L. donovani, Leishmania aethiopica and Leishmania tropica in the Old World.[8] This serious clinical form of human leishmaniasis infection usually does not affect the ears; however, involvement of the rhinopharynx can lead to eustachian tube dysfunction with consequent otitis media with effusion. Conductive hearing loss, tinnitus and dysacusis are the major complaints in such cases, as in the present case.[8]
The differential diagnosis of ulcerative auricular lesions includes pyoderma gangrenosum, bacterial, fungal, atypical mycobacterial or tubercular infections, cutaneous leishmaniasis, lymphoproliferative disorders or neoplasms.[7] The sites of paracoccidioidomycosis on the ear can be confused with other tropical diseases frequently found in the Amazon region such as leishmaniasis, leprosy and lobomycosis. The diagnosis of cutaneous leishmaniasis on the ear requires a high index of suspicion. The detection of antigen of Leishmania in urine samples is a tool for predicting clinical visceral leishmaniasis as well as to monitor parasite clearance during treatment.[9]
The treatment of cutaneous leishmaniasis depends on its clinical manifestations as well as on the location and diameter of the lesion. Treatment includes systemic or intralesional pentavalent antimonials, sodium stibogluconate and meglumine antimonials, amphotericin B and cryotherapy. We chose liposomal amphotericin B because of the extensive involvement and since the patient was already on immunosuppressive therapy with good control of the disease. Liposomal amphotericin B presents similar efficacy with fewer side effects, the limiting factor being cost.
To minimize injection-associated complications, different oral drugs, such as ketoconazole, fluconazole, miltefosine and paromomycin, have been recently proposed.[1],[10]
There are no financial supports or sponsorships.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Marra F, Chiappetta MC, Vincenti V. Ear, nose and throat manifestations of mucocutaneous leishmaniasis: A literature review. Acta Biomed 2014;85:3-7.
[Google Scholar]
|
| 2. |
Sabri A, Khatib L, Kanj-Sharara S, Husseini ST, Nuwayri-Salti N, Semaan R, et al. Leishmaniasis of the auricle mimicking carcinoma. Am J Otolaryngol 2009;30:285-7.
[Google Scholar]
|
| 3. |
Vaira F, Nazzaro G, Pesapane F, Veraldi S. 'Dumbo' ear. Clin Exp Dermatol 2014;39:667-8.
[Google Scholar]
|
| 4. |
Abu-Laban RB. “Chiclero's ulcer”. CMAJ 1986;134:216.
[Google Scholar]
|
| 5. |
Khorsandi-Ashtiani MT, Hasibi M, Yazdani N, Paydarfar JA, Sadri F, Mirashrafi F, et al. Auricular leishmaniasis mimicking squamous cell carcinoma. J Laryngol Otol 2009;123:915-8.
[Google Scholar]
|
| 6. |
Silva Mdos S, Sousa RT, Silva EB, Guerra JA, Gomes NM, Santana RF, et al. Primary lesion of mucocutaneous leishmaniasis simulating external otitis. Braz J Otorhinolaryngol 2012;78:137.
[Google Scholar]
|
| 7. |
Tarkan Ö, Çetik F, Uzun S. Auricular cutaneous leishmaniasis mimicking neoplastic disease. J Laryngol Otol 2012;126:821-4.
[Google Scholar]
|
| 8. |
Lessa MM, Lessa HA, Castro TW, Oliveira A, Scherifer A, Machado P, et al. Mucosal leishmaniasis: Epidemiological and clinical aspects. Braz J Otorhinolaryngol 2007;73:843-7.
[Google Scholar]
|
| 9. |
Islam MZ, Itoh M, Ul Islam MA, Saifuddin Ekram AR, Rahman MA, Takagi H, et al. ELISA with recombinant rKRP42 antigen using urine samples: A tool for predicting clinical visceral leishmaniasis cases and its outbreak. Am J Trop Med Hyg 2012;87:658-62.
[Google Scholar]
|
| 10. |
Veraldi S, Nazzaro G. Successful treatment of cutaneous leishmaniasis of the ear with oral fluconazole. Clin Exp Dermatol 2016;41:315-6.
[Google Scholar]
|
Fulltext Views
4,077
PDF downloads
3,573





