Translate this page into:
Palmoplantar aquagenic urticaria: A case report
2 Department of Endocrinology, Krishna Institute of Medical Sciences, Secunderabad, Telangana, India
Correspondence Address:
Prachi Rakesh Srivastava
Department of Dermatology, Krishna Institute of Medical Sciences, Secunderabad, Telangana
India
| How to cite this article: Srivastava PR, Vaggu AK, Kasoju S, Khare J. Palmoplantar aquagenic urticaria: A case report. Indian J Dermatol Venereol Leprol 2017;83:592-593 |
Sir,
Physical urticarias are a unique subgroup of chronic urticarias, first described by Duke in 1964, in which wheals can be repeatedly induced by the corresponding physical stimuli. They form 19% of all chronic urticarias. Aquagenic urticarias are further rare with a fewer than fifty reported cases.[1] The localized variant is unique with only two cases documented till date.[2] Treatment options include barrier creams, oral antihistamines, acetylcholine antagonists, psoralen combined with ultraviolet A therapy and the recently reported omalizumab.
A 30-year-old woman presented with a 4-year history of development of itchy raised lesions on the palms and soles following contact with water. The lesions began to develop within 5 min of contact with water, were restricted to palms and soles without any other areas of involvement and resolved on application of coconut oil. She had history of atopy as elicited by the Hanifin and Rajka criteria. There was no other significant personal, past or family history.
Cutaneous examination revealed lesions as pruritic wheals ranging in size from 2 to 3 mm with surrounding erythema which developed within 5 min of contact with water. The lesions were restricted to the palms and soles and were independent of the temperature and osmolarity of the water. There were no symptoms on water ingestion. Her complete blood picture, erythrocyte sedimentation rate, renal and hepatic profile were normal. Suspecting aquagenic urticaria, provocation tests were performed with tap water and 0.9M normal saline at room temperature applied for 30 min. The patient developed wheals in 5 min [Figure - 1]; however there was the absence of wheals on the forearm [Figure - 2] thereby confirming the diagnosis of aquagenic urticaria restricted to the palms and soles. She was advised to limit water-related chores and water in oil emollient cream before each water exposure along with hydroxyzine 10 mg tablet daily at night. On follow-up after a month the patient reported relief with just the emollient even in the absence of antihistaminic which was then discontinued. The patient is now symptom free on application of the emollient before each water exposure.
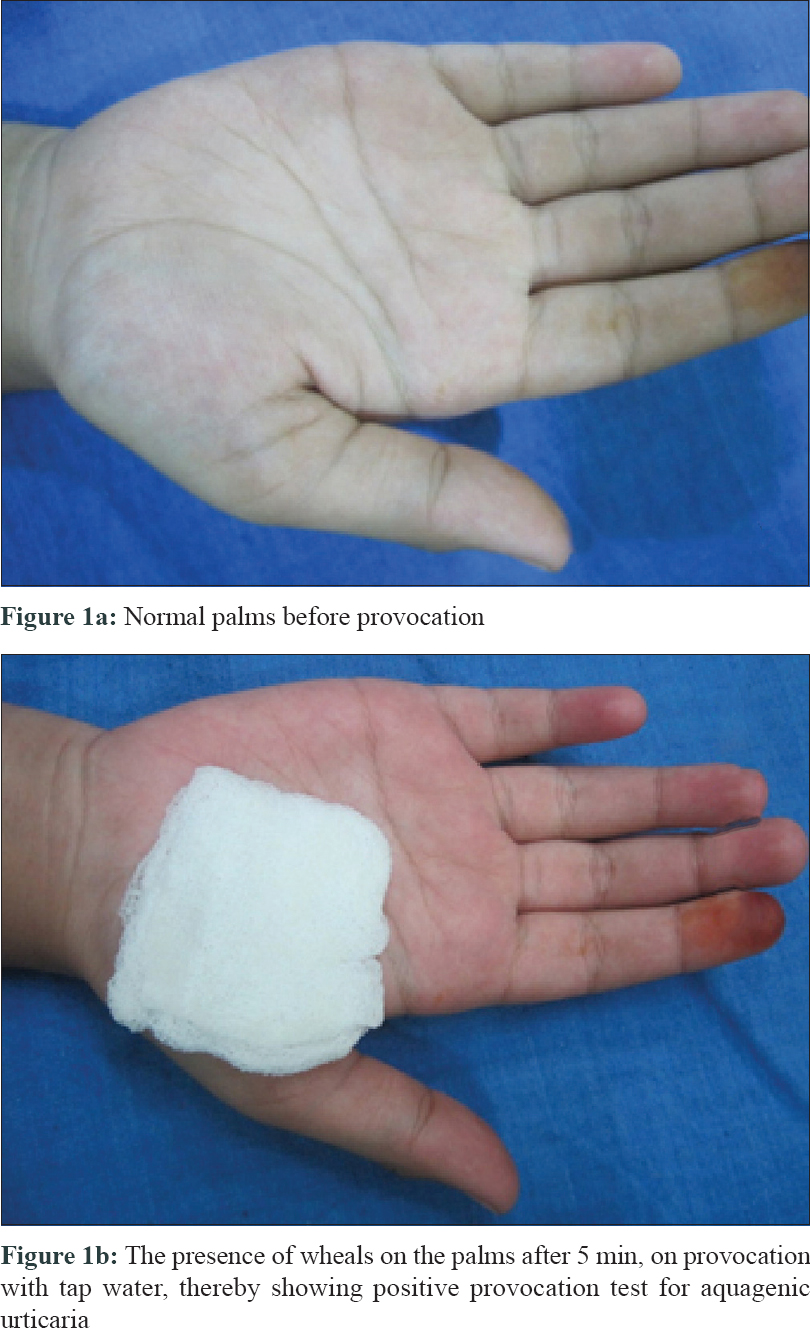 |
| Figure 1 |
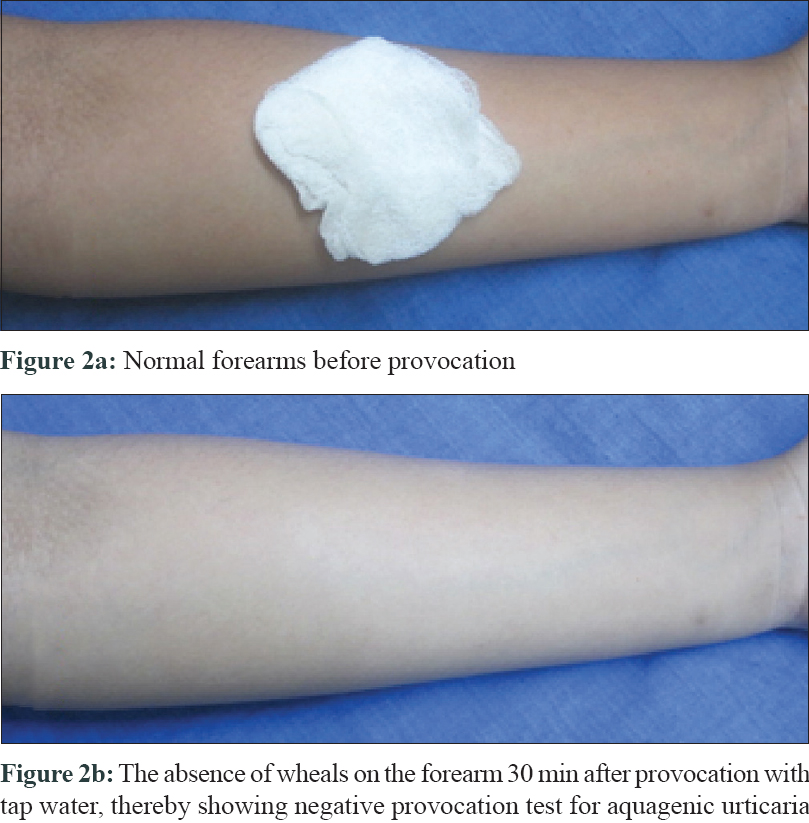 |
| Figure 2 |
Physical urticarias are a unique subgroup of chronic urticarias, in which wheals can be repeatedly induced by the corresponding physical stimuli.[3] Aquagenic urticaria is a rare form of physical urticaria in which contact with water, irrespective of its temperature evokes wheals.[4],[5] Since its first description by Shelley and Rawnsley in 1964, <50 cases have been described.[6],[7] Aquagenic urticaria is more common in females than males and appears during puberty or several years later.[4]
Clinical presentation is in the form of pruritic wheals ranging from 1 to 3 mm in diameter which appear only on areas which come in contact with water. The most commonly reported locations are the neck, upper trunk and arms.[4],[8]
The pathogenesis is still unclear, the hypothesis as put forth by Shelley and Rawnsley suggests that water reacts with a component of the sebum or sebaceous gland to produce a histamine liberator which is absorbed with subsequent discharge of histamine from the perifollicular mast cells.[8] Recent hypothesis by Gallo et al. asserts the role of transient receptor potential 1 vanilloid subtype channel that may play a role in salt-dependent aquagenic urticaria which is now increasingly being described as a separate entity.[6],[9]
Although there are quite a few case reports of aquagenic urticaria, localization of aquagenic wheals to certain parts of the body has rarely been reported with only two documented cases till date.[1] The first case reported localization of wheals to the “V” area of the neck and second to the dorsum of hands with sparing of the palms.[1] Our case is unique as to the strict localization of the wheals to the palms and soles. Furthermore, the osmolarity of the water had no effect on the whealing. The patient responded to barrier creams without requiring oral antihistamine therapy, thereby supporting Shelley's hypothesis of water acting as a carrier for some unknown epidermal antigen. The other treatment options include psoralen combined with ultraviolet A therapy which is thought to work by inducing thickening of skin, acetylcholine antagonists and the most recently reported biological omalizumab which is a monoclonal anti-immunoglobulin E 20 antibody.[7] Antihistamines may be useful, but some patients may not respond or may respond only in high doses.[4]
We are unable to find any previous reported case of aquagenic urticaria localized to the palmoplantar area. We would thus like to bring focus this entity which is under recognized and probably under-reported leading to delay in diagnosis or misdiagnosis and causing significant impairment in quality of lives of patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Prasad PS. Urticaria. Indian J Dermatol Venereol Leprol 2001;67:11-20.
[Google Scholar]
|
| 2. |
Blanco J, Ramirez M, Garcia F, Herrero D, Fuentes M, Pérez R. Localized aquagenic urticaria. Contact Dermatitis 2000;42:303-4.
[Google Scholar]
|
| 3. |
Singh M, Kaur S, Kanwar AJ. Evaluation of the causes of physical urticarias. Indian J Dermatol Venereol Leprol 1990;56:10911.
[Google Scholar]
|
| 4. |
Park H, Kim HS, Yoo DS, Kim JW, Kim CW, Kim SS, et al. Aquagenic urticaria: A report of two cases. Ann Dermatol 2011;23 Suppl 3:S371-4.
[Google Scholar]
|
| 5. |
Bayle P, Gadroy A, Messer L, Bazex J. Localized aquagenic urticaria: Efficacy of a barrier cream. Contact Dermatitis 2003;49:160-1.
[Google Scholar]
|
| 6. |
Gallo R, Gonçalo M, Cinotti E, Cecchi F, Parodi A. Localized salt-dependent aquagenic urticaria: A subtype of aquagenic urticaria? Clin Exp Dermatol 2013;38:754-7.
[Google Scholar]
|
| 7. |
Rorie A, Gierer S. A case of aquagenic urticaria successfully treated with omalizumab. J Allergy Clin Immunol Pract 2016;4:547-8.
[Google Scholar]
|
| 8. |
Shelley WB, Rawnsley HM. Aquagenic urticaria. Contact sensitivity reaction to water. JAMA 1964;189:895-8.
[Google Scholar]
|
| 9. |
Margerin F, Wettlé C, Merklen-Djafri C, Cribier B. Localized salt-dependent aquagenic urticaria: A case report. Ann Dermatol Venereol 2015;142:771-5.
[Google Scholar]
|
Fulltext Views
4,432
PDF downloads
1,259





