Translate this page into:
Palmoplantar hyperhidrosis: A paradoxical presentation of acquired idiopathic generalized hypohidrosis
Correspondence Address:
Hong Liang Tey
National Skin Centre, 1 Mandalay Road, 308205
Singapore
| How to cite this article: Kong YL, Tey HL. Palmoplantar hyperhidrosis: A paradoxical presentation of acquired idiopathic generalized hypohidrosis. Indian J Dermatol Venereol Leprol 2017;83:480-481 |
The etiology of palmoplantar hyperhidrosis is primary in the vast majority of cases and the secondary causes, comprising drugs, neurological or endocrine disorders, are rare. Acquired idiopathic generalized anhidrosis is an uncommon disorder characterized by widespread anhidrosis in the absence of sweat gland pathology or neurologic symptoms.[1],[2],[3],[4] Impaired ability to sweat can predispose the affected individuals to hyperthermia, heat stroke and even death. We report a patient with acquired idiopathic generalized anhidrosis who presented with palmoplantar hyperhidrosis.
A 20-year-old Chinese man presented with a history of progressively worsening palmoplantar hyperhidrosis since his teenage years which interfered with his daily activities. He also recalled a concurrent decreased ability to sweat on his trunk during physical activity with symptoms of heat intolerance (manifesting as light headedness) on physical exertion necessitating cessation of the activity. There were no symptoms of thyroid, autonomic or neurological dysfunction and no history of dry eyes or mouth. His past medical history was not significant and he was not on any medications. Family and travel history was not significant.
On examination, sweat droplets were seen on his palms and soles, while elsewhere, his skin was generally dry. Hair, nails and joints were normal and there were no hypopigmented patches or thickened peripheral nerves. There were no fine tremors, anterior neck masses or eye signs, suggestive of hyperthyroidism. Neurological examination was unremarkable with the patient demonstrating normal tone, power and tendon reflexes in the upper and lower extremities as well as intact cranial nerves and a normal sensory system. Blood pressure was normal and there was no postural hypotension.
His laboratory investigations including blood counts, renal, liver and thyroid function tests were unremarkable. Erythrocyte sedimentation rate and serum immunoglobulin E were normal and autoimmune markers were negative. Minor starch-iodine sweat test (using the methodology we previously described)[5] revealed hyperhidrosis on both palms [Figure - 1], with anhidrosis affecting about 80% of his trunk [Figure - 2]. High-definition optical coherence tomography imaging of the palms demonstrated the presence of sweat glands [Figure - 3].
 |
| Figure 1: Starch iodine test: An admixture of starch-iodine powder was applied to dry hands of patient which turned purple within a minute. Notably, there was an absence of sweating proximal to the wrist crease (powder was still brown) |
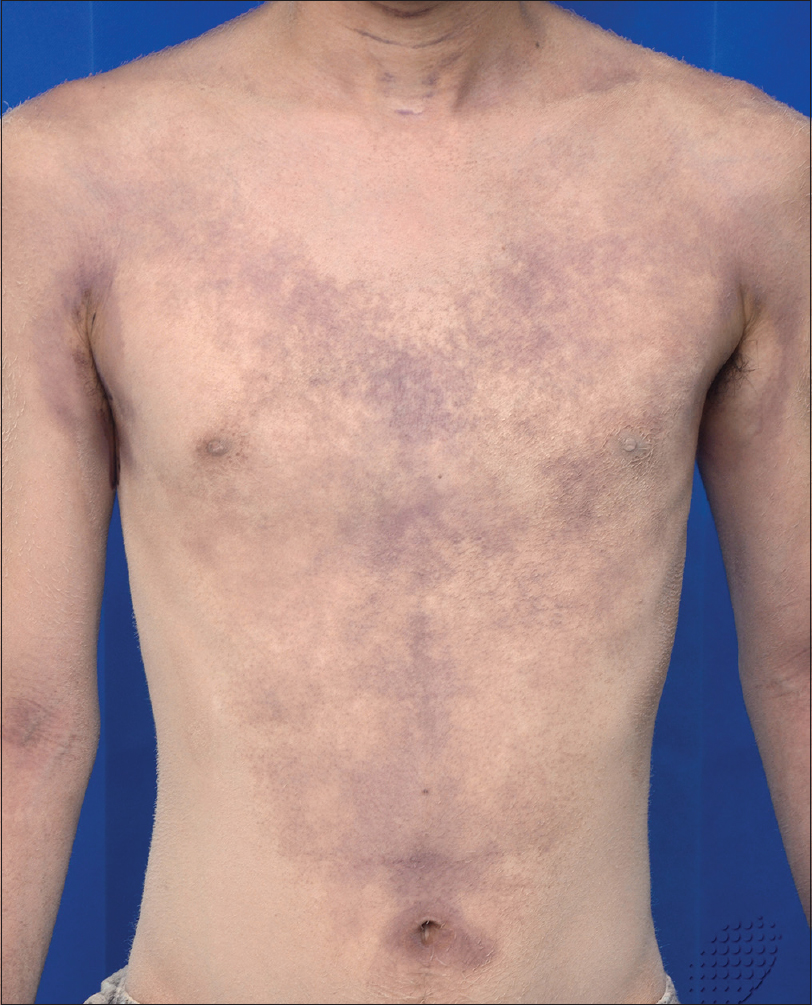 |
| Figure 2: Patchy and markedly reduced sweating on the trunk demonstrated by starch-iodine test |
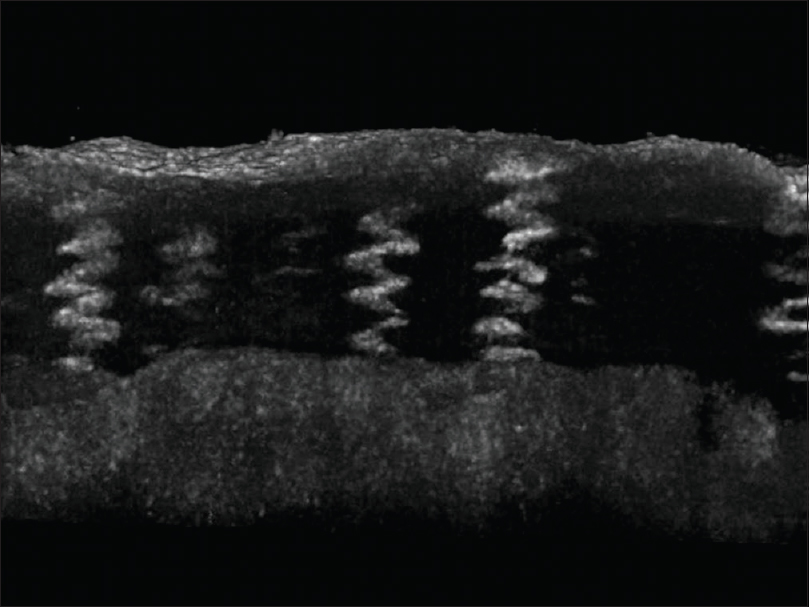 |
| Figure 3: Reconstructed high definition optical coherence tomography image of the palm demonstrating normal acrosyringium |
A diagnosis of acquired idiopathic generalized anhidrosis with compensatory palmoplantar hyperhidrosis was made. His palmoplantar sweating improved significantly upon the initiation of twice weekly sessions of iontophoresis. For his anhidrosis, he was given a trial of oral steroidswhich were discontinued due to giddiness. The patient was counseled to avoid conditions with high ambient temperatures, as well as heavy physical exertion.
Acquired idiopathic generalized anhidrosis typically occurs in otherwise healthy young individuals, usually in the third decade of life.[1],[2] There appears to be preponderance in Asian men, but this observation may be skewed by their greater participation in physical activities compared to women, as well as the mandatory military service for men in many Asian countries.[1]
The underlying pathogenesis of this disorder is heterogeneous. The three subtypes of the condition include idiopathic pure sudomotor failure, sweat gland dysfunction and sudomotor neuropathy, each representing different underlying mechanisms.[1] Most cases seem to represent idiopathic pure sudomotor failure which may be explained by a postsynaptic defect in the cholinergic receptors of eccrine glands.[2] The preservation of sweating on the palms, soles and axillae in the condition supports this theory. as the sweat glands in the palms and soles though eccrine in origin, have been previously shown to be partially under adrenergic innervation.[2] As the ability to sweat on palms and soles is not compromised in this condition, palmoplantar hyperhidrosis may occur as a compensatory mechanism for the body to dissipate heat. Although palmoplantar hyperhidrosis has previously been described to occur as a compensatory mechanism to anhidrosis in patients with leprosy, this is rarely seen in patients with acquired idiopathic generalized anhidrosis.
Treatment of this disorder remains poorly established. Immunosuppressants such as systemic corticosteroids and ciclosporin have been tried as therapeutic options previously with varying success. Ciclosporin is thought to act by inhibiting the activity of T-cells which have been seen to infiltrate the eccrine glands.[3] Masuda et al. suggested that acquired idiopathic generalized anhidrosis is an immunological disorder that may involve autoantibodies and described the successful use of intravenous immunoglobulin in the treatment of two patients with this condition.[4] As response to any treatment remains inconsistent, prevention of heat injury by introducing lifestyle changes is the key and education remains the cornerstone in the management of this disorder.
In conclusion, we describe a patient with compensatory palmoplantar hyperhidrosis secondary to underlying acquired idiopathic generalized hypohidrosis. It is important to consider this unusual diagnosis in the evaluation of patients presenting primarily with palmoplantar hyperhidrosis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Tay LK, Chong WS. Acquired idiopathic anhidrosis: A diagnosis often missed. J Am Acad Dermatol 2014;71:499-506.
[Google Scholar]
|
| 2. |
Nakazato Y, Tamura N, Ohkuma A, Yoshimaru K, Shimazu K. Idiopathic pure sudomotor failure: Anhidrosis due to deficits in cholinergic transmission. Neurology 2004;63:1476-80.
[Google Scholar]
|
| 3. |
Ohshima Y, Yanagishita T, Ito K, Tamada Y, Nishimura N, Inukai Y, et al. Treatment of patients with acquired idiopathic generalized anhidrosis. Br J Dermatol 2013;168:430-2.
[Google Scholar]
|
| 4. |
Masuda T, Obayashi K, Ueda M, Fujimoto A, Tasaki M, Misumi Y, et al. Therapeutic effects and prevention of recurrence of acquired idiopathic generalized anhidrosis via i.v. immunoglobulin treatment. J Dermatol 2016;43:336-7.
[Google Scholar]
|
| 5. |
Lim JH, Choo W, Chang JH, Tey HL, Chong WS. Application of iodinated starch powder using an atomizer spray gun - A new and effective tool to evaluate hypohidrosis. Skin Res Technol 2016;22:370-4.
[Google Scholar]
|
Fulltext Views
4,578
PDF downloads
3,846





