Translate this page into:
Palmoplantar keratoderma with honeycombing: A case of loricrin keratoderma with heterozygous frameshift mutation in LOR gene, from India
Corresponding author: Dr. Bushra Muna, Department of Dermatology, Venereology and Leprosy, Mahatma Gandhi Medical College and Research Institute, Pillayarkuppam, Puducherry, India. bushramuna@mgmcri.ac.in
-
Received: ,
Accepted: ,
How to cite this article: Muna B, Neerukonda P, Shanmugam S. Palmoplantar keratoderma with honeycombing: A case of loricrin keratoderma with heterozygous frameshift mutation in LOR gene, from India. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_327_2024
Dear Editor,
Diffuse palmoplantar keratoderma (PPK) presenting in a honeycomb pattern can be seen in loricrin keratoderma and Vohwinkel syndrome. Loricrin keratoderma or Camisa syndrome is also considered a variant of Vohwinkel syndrome.
A 6-week-old male infant born to non-consanguineous parents presented with diffuse thickening of palms having a honeycomb pattern [Figure 1a]. On examination, the presence of light brown polygonal scales over extensors of extremities suggesting mild ichthyosis was also noted. A dermoscopic furrow ink test of the proband’s thumb revealed an irregular cobblestone pattern. There was a history of collodion membrane at birth but the rest of the antenatal and birth history was unremarkable. There was also the history of similar palmo-plantar lesions with hypohidrosis in the mother and maternal grandfather. On examination of the mother there was honeycomb pattern of transgradient palmoplantar keratoderma with pseudoainhum and knuckle pads [Figure 1b and 1c], rippled pattern of hyperkeratotic plaques over flexures and medial aspect of knees [Figure 1d] and light to dark brown polygonal ichthyotic scales involving extensor aspects of limbs and face [Figure 1e]. An audiometry examination of the mother showed no significant hearing loss. Whole exome sequencing was done using nuclear and mitochondrial DNA which was obtained from the peripheral blood sample of the proband. We identified a heterozygous frameshift variant, c.678_679insG in Exon 2 of the LORICRIN gene resulting in the amino acid substitution p.Ser229fs*86. A final diagnosis of Loricrin keratoderma was made based on clinical findings and genetic testing. The patient was started on acitretin 0.5 mg/kg/day with regular anthropometric, lipid, and liver function monitoring for 9 months and a drug-free period of 3 months. There was clinical improvement and the patient is currently maintained with general protective measures and topical emollients. The mother was started on acitretin recently and reported improvement in hypohidrosis and skin lesions.
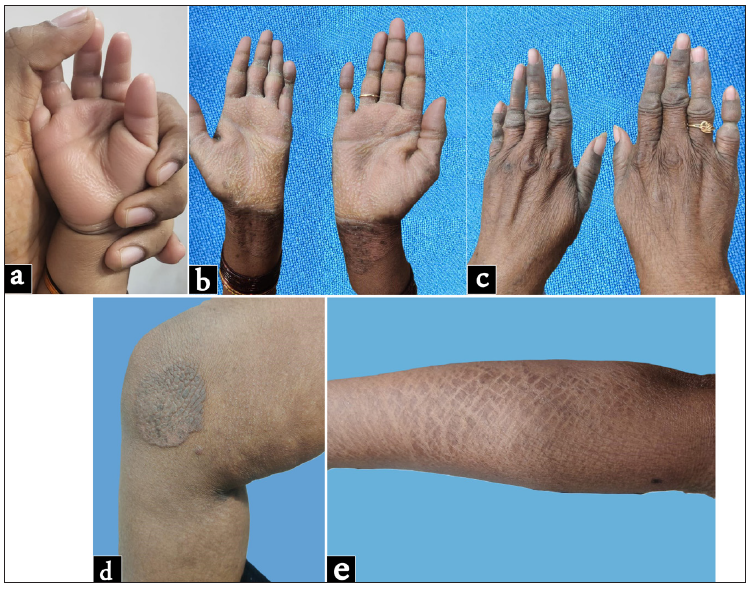
- (a) Honeycomb pattern of palmoplantar keratoderma in proband at 6 weeks; (b) Honeycomb pattern of palmar keratoderma with pseudo-ainhum of proband’s mother; (c) Knuckle pads on the hands of proband’s mother; (d) Hyperkeratotic rippled plaque seen on the medial aspect of knees of proband’s mother; (e) Ichthyosis seen over the extensor aspect of the forearm of the proband’s mother.
Though loricrin keratoderma and Vohwinkel syndrome present with diffuse type of PPK in a honeycomb pattern through autosomal dominant mode of inheritance, the former differs clinically from the latter by the absence of sensorineural hearing loss and starfish-shaped keratotic knuckle plaques.1 Genetically, mutation in LOR and GJB2 is seen in loricrin keratoderma and Vohwinkel syndrome, respectively. Collodion membrane is the initial presentation in some cases of loricrin syndrome (46%) as seen in our case and hence it should be considered as one of the differential diagnoses for the cause of collodion membrane in a neonate.2 Later, all patients develop transgradient palmoplantar keratoderma with a characteristic honeycomb-like appearance and 92% displayed generalised non-erythrodermic ichthyosis (fine white scales without underlying erythema) with 19% having flexural involvement as per. As per the review of previously published case reports, prominent knuckle pads (15%) and pseudoainhum (65%) are also features that are seen variably in this condition which were present in our proband’s mother.
Loricrin is a protein consisting of four highly flexible glycine loop domains that are flanked by glutamine and glutamine/lysine rich regions. These regions act as a substrate for transglutaminase mediated N-ε (γ glutamyl) lysine crosslinking of components of the cornified envelope which in addition to disulphide bonds account for the highly insoluble nature of loricrin. A review of the existing literature revealed 14 different mutations reported in 26 unrelated pedigrees. The most frequent mutation is the frameshift insertion mutation (730insG) in the loricrin gene that has been documented in the literature.3 The frameshift mutations in loricrin keratoderma were also seen in our case wherein glycine-rich C-terminus is replaced by arginine-rich nuclear localization signal sequence leading to accumulation of loricrin in the nucleus which hampers the permeability barrier.4 In our case, the frameshift mutation is anticipated to result in delayed termination of codon resulting in protein extension, wherein the final 84 amino acids are substituted with a set of 106 distinct amino acids. Published functional investigations reveal that this altered loricrin variant induces the activation of diverse growth factor receptors and heightened protein kinase B (AK strain transforming kinase) activity. These molecular changes contribute to the observed accelerated keratinocyte proliferation seen in the disorder that results in hyperkeratosis on the palms and soles. A 50-year-old woman diagnosed as loricrin keratoderma with a mutation similar to ours has been reported from Italy who was also diagnosed with breast cancer and showed complete remission of PPK, pseudoainhum, ichthyosis with concomitant tamoxifen chemotherapy.5 The age at which palmoplantar keratoderma has developed varies across the reports ranging from 3 months to 30 years and in our proband, the honeycomb pattern was seen at 6 weeks of life.
Treatment options include emollients, topical keratolytics, and low-dose isotretinoin or acitretin which is used to prevent pseudoainhum formation.6 Revertant mosaicism due to somatic recombination has been documented in loricrin keratoderma.7
Acknowledgement
The authors would like to acknowledge Ms. Simran Thawani for her contribution in genetic analysis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Hereditary palmoplantar keratoderma: A practical approach to the diagnosis. Indian Dermatol Online J. 2019;10:365-79.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Mild collodion baby as a presenting sign of loricrin keratoderma: Report of a case and review of the literature. Clin Exp Dermatol. 2020;45:395-8.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopic furrow ink test of the palmar lesion in loricrin keratoderma. J Dermatol. 2022;49:783-86.
- [CrossRef] [PubMed] [Google Scholar]
- Loricrin keratoderma: a novel disease entity characterized by nuclear accumulation of mutant loricrin. J Dermatol Sci. 2003;31:3-8.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical remission of loricrin keratoderma with tamoxifen: A case report. Acta Derm Venereol. 2020;100:adv00272.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Low-dose isotretinoin prevents digital amputation in loricrin keratoderma (Vohwinkel syndrome with ichthyosis) J Dtsch Dermatol Ges. 2017;15:665-7.
- [CrossRef] [PubMed] [Google Scholar]
- Somatic recombination underlies frequent revertant mosaicism in loricrin keratoderma. Life Sci Alliance. 2019;2:e201800284.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]





