Translate this page into:
Papules, pock-like scars, and hoarseness of voice
2 Department of Histopathology, Postgraduate Institute of Medical Education and Research, Chandigarh, India,
Correspondence Address:
C Vijay Krishna
46, Arbor circle, Philadelphia, Pennsylvania, USA
| How to cite this article: Parmar NV, Krishna C V, De D, Kanwar AJ, Saikia UN. Papules, pock-like scars, and hoarseness of voice. Indian J Dermatol Venereol Leprol 2013;79:136 |
Case Report
A 6-year-old boy presented with hoarseness of voice and recurrent episodes of blisters and erosions on the scalp, face, trunk, and extremities since 6 months of age. The erosions healed with scarring. Most lesions were spontaneous in onset although some were post-traumatic. There was no developmental delay. There was neither history of photosensitivity nor of similar family history. His parents were non-consanguineous.
Mucocutaneous examination revealed multiple pearly beaded papules on the margins of bilateral upper and lower eyelids [Figure - 1]. Multiple "pock-like" scars were present on the face, trunk, and extremities. Few crusted erosions were present on the scalp and extensors of forearms. Lips were enlarged, their mucosal surface revealing yellowish indurated papules. Tongue was enlarged, firm on palpation and the boy had difficulty in protruding it [Figure - 2]. Patches of scarring alopecia were present on the occiput and vertex of scalp.
 |
| Figure 1: Multiple pearly papules over eyelid margins of both eyes |
 |
| Figure 2: Enlarged tongue with difficulty in protrusion |
Histopathological examination of the lower lip revealed periodic acid Schiff (PAS)-positive deposits, but diastase-resistant pale eosinophilic hyaline material in the papillary and deep dermis [Figure - 3]. Congo red stain was negative. There was marked atrophy of adnexal structures [Figure - 4] with few blood vessels showing onion skinning [Figure - 5]. Direct laryngoscopy revealed thickened but mobile vocal cords with surface nodulations.
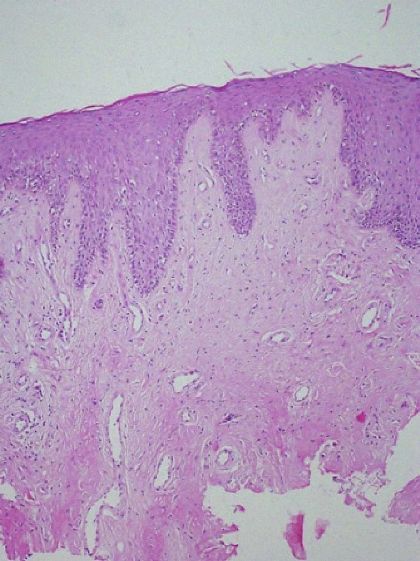 |
| Figure 3: PAS-positive and diastase-resistant deposits in upper and deep dermis (H and E, ×100) |
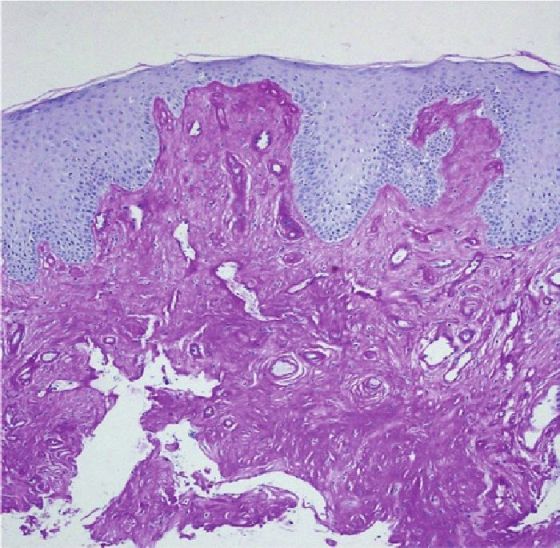 |
| Figure 4: Marked atrophy of adnexae with few blood vessels showing onion skinning (H and E, ×40) |
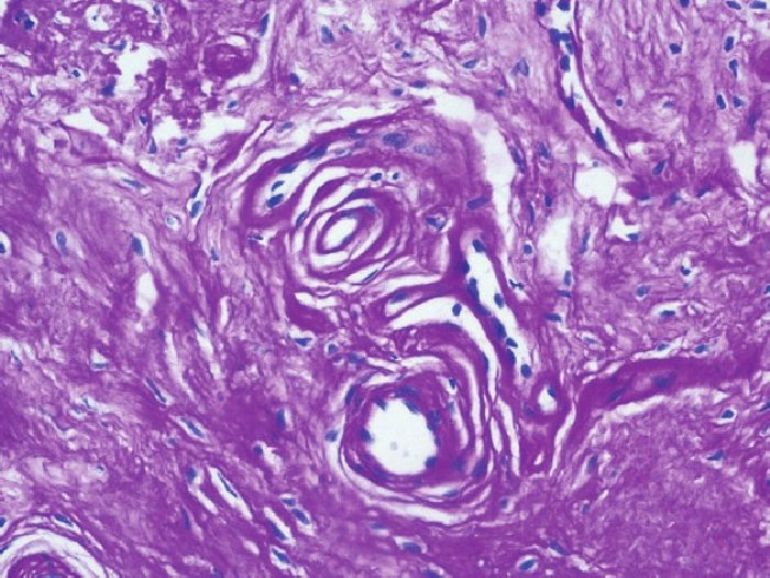 |
| Figure 5: Onion skinning of blood vessels with PAS-positive and diastase-resistant deposits in deep dermis (H and E, ×200) |
What is your diagnosis?
| 1. |
Urbach E, Wiethe C. Lipoidosis cutis et mucosae. Virchows Arch Pathol Anat 1929;273:285-319.
[Google Scholar]
|
| 2. |
Sercu S, Zhang M, Oyama N, Hansen U, Ghalbzouri AE, Jun G, et al. Interaction of extracellular matrix protein 1 with extracellular matrix components: ECM1 is a basement membrane protein of the skin. J Invest Dermatol 2008;128:1397-408.
[Google Scholar]
|
| 3. |
Aroni K, Lazaris AC, Papadimitriou K, Paraskevakou H, Davaris PS. Lipoid proteinosis of the oral mucosa: Case report and review of the literature. Pathol Res Pract 1998;194:855-9.
[Google Scholar]
|
| 4. |
Bahadir S, Cobanoðlu U, Kapicioðlu Z, Kandil ST, Cimþit G, Sönmez M, et al . Lipoid proteinosis: A case with ophthalmological and psychiatric findings. J Dermatol 2006;33:215-8.
[Google Scholar]
|
| 5. |
Dogramaci AC, Celik MM, Celik E, Bayarogullari H. Lipoid proteinosis in the eastern Mediterranean region of Turkey. Indian J Dermatol Venereol Leprol 2012;78:318-22.
[Google Scholar]
|
| 6. |
Buchan NG, Kemble JV. Successful surgical treatment of lipoid proteinosis. Br J Dermatol 1974;90:561-6.
[Google Scholar]
|
| 7. |
Gruber F, Manestar D, Stasic A, Grgurevic Z. Treatment of lipoid proteinosis with etretinate. Acta Derm Venereol 1996;76:154-5.
[Google Scholar]
|
Fulltext Views
3,728
PDF downloads
2,330






