Translate this page into:
Papulonecrotic tuberculid with optic neuritis
Correspondence Address:
Zhancai Zheng
Department of Dermatology, China-Japan Friendship Hospital, No. 2, Yinghua East Street, Chaoyang District, Beijing 100029
China
| How to cite this article: Wang Y, Li S, Bai Y, Cui Y, Zheng Z. Papulonecrotic tuberculid with optic neuritis. Indian J Dermatol Venereol Leprol 2020;86:404-406 |
Sir,
Papulonecrotic tuberculid is considered as a hypersensitivity reaction to Mycobacterium tuberculosis or its antigen in individuals with good immunity. Though bacilli are not always identified on special stains and culture, strongly positive tuberculin test and rapid response to antituberculosis therapy show no doubt of tuberculous etiology in papulonecrotic tuberculid.[1] Optic neuritis can occur in infectious diseases like tuberculosis due to direct invasion or immunemediated reaction. We were unable to find any previous reports of papulonecrotic tuberculid associated with optic neuritis. Herein we report one such rare case.
A 16-year-old female presented with a 7-year-history of multiple, recurrent reddish lesions on extremities and back. She also had an acute decline of vision in the left eye for 2 weeks. She denied any history of chronic cough, fever and weight loss. She had no past history of tuberculosis. On examination, multiple erythematous papules distributed symmetrically on her extremities and back with some lesions showing necrosis and crusting, interspersed with atrophic varioliform scars [Figure - 1]a and [Figure - 1]b. Corrected visual acuity was 1.5/1.5 in the right eye and 0.6/1.5 in the left eye. Visual field testing proved normal in the right eye but showed a central scotoma in the left eye. Pattern visual evoked potential testing revealed normal in both eyes. Flash visual evoked potential testing turned normal in right eye but revealed delayed latency in left eye. Head magnetic resonance imaging showed a thinning accompanied by increased signal intensity of the left optic nerve in the intraorbital and canal segments, while the right optic nerve was normal [Figure - 2]a and [Figure - 2]b. Optic neuritis of the left eye was diagnosed based on the clinical features, ophthalmic examination and radiological findings. Tuberculosis interferon-γ release assay was positive and tuberculin test was strongly positive. Tests for antinuclear antibodies, antineutrophil cytoplasmic autoantibody, hepatitis B surface antigen, anti-hepatitis C virus antibody, anti-human immunodeficiency virus antibody and syphilis antibody were negative. Erythrocyte sedimentation rate, cerebrospinal fluid examination, abdominal ultrasonography and chest X-ray were normal. Skin biopsy showed a wedge-shaped area of necrosis involving the epidermis and dermis along with vasculitis at the base of the necrosis. The fibrinoid necrosis was surrounded by moderately dense lymphohistiocytic infiltrate [Figure - 3]a, [Figure - 3]b, [Figure - 3]c, [Figure - 3]d. Based on the clinical features, histopathology and laboratory examinations, a diagnosis of papulonecrotic tuberculid was rendered. Thus with the diagnosis of papulonecrotic tuberculid and optic neuritis she was started on antituberculosis medications. After 6 months of treatment, her lesions disappeared leaving some atrophic scars, but her vision did not improve. Then, she was given 40mg methylprednisolone daily. After 4-week treatment, the dose of methylprednisolone was reduced 8mg every two weeks until dose was 16mg daily. Then the dose was reduced by 4mg every 2 to 4 weeks. After 2 months of treatment, her vision improved. The steroids was completely stopped after 5-month therapy. In the follow-up period of 4 years her skin lesions did not reappear, but her vision declined intermittently and had a good response to steroids.
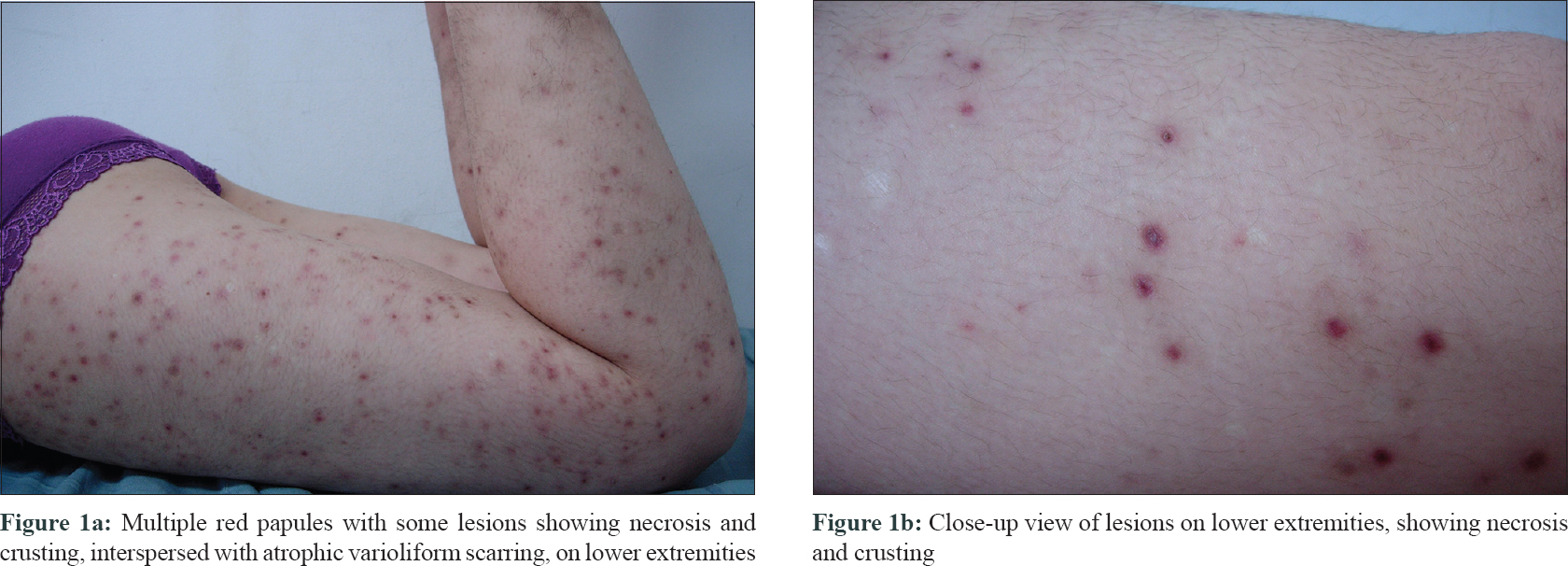 |
| Figure 1: |
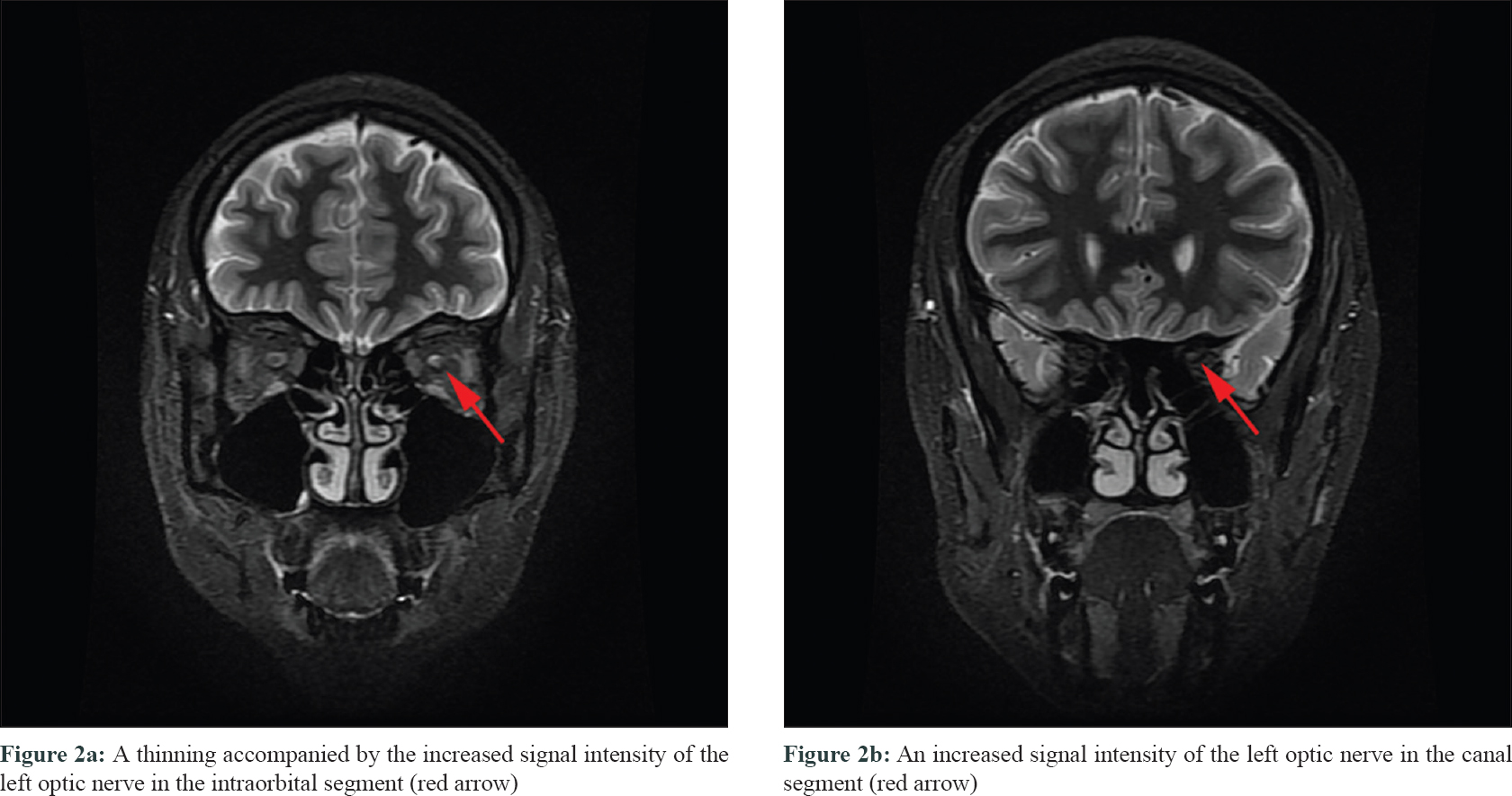 |
| Figure 2: |
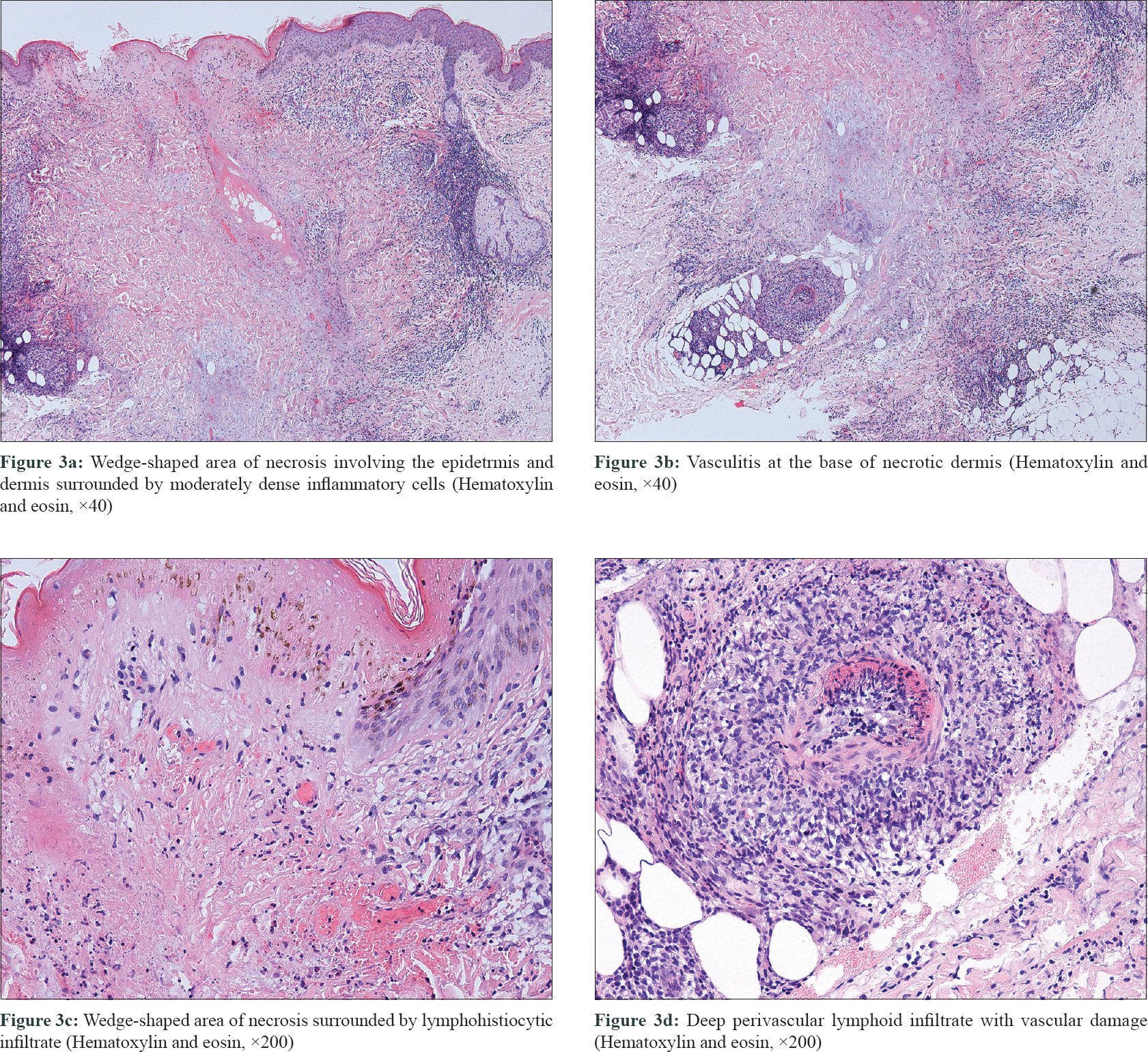 |
| Figure 3: |
Tuberculous focus cannot be demonstrated in all cases of papulonecrotic tuberculid and Mycobacterium bacilli are usually not detected in it.[2] Advanced techniques like polymerase chain reaction have improved the positive detection rate of bacilli, but negative result does not exclude the diagnosis of papulonecrotic tuberculid. Papulonecrotic tuberculid is diagnosed on the basis of clinical features, histopathology, evidence of underlying focus of tuberculosis, strongly positive tuberculin test and adequate response to antitubercular treatment.[3] Infectious optic neuritis can be caused by direct spread of pathogenic organism or result from pathogen-induced immune allergic reaction to optic nerve where anti-infection treatment or systemic steroid therapy is recommended respectively.[4] In our case, the vision of the patient improved with steroids, supporting the diagnosis of immune-mediated tuberculous optic neuritis. The patient developed optic neuritis after suffering from papulonecrotic tuberculid for 7 years and this points towards the importance of an early diagnosis of papulonecrotic tuberculid. Papulonecrotic tuberculid is rarely associated with ophthalmic disease. The only reported ocular association of papulonecrotic tuberculid is uveitis which manifested as unilateral redness of eye.[5] The association between papulonecrotic tuberculid and optic neuritis as reported in our case gives us a new understanding of the complication of papulonecrotic tuberculid. Thus, we should pay more attention to ocular manifestations of the patients with papulonecrotic tuberculid.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Barbagallo J, Tager P, Ingleton R, Hirsch RJ, Weinberg JM. Cutaneous tuberculosis: Diagnosis and treatment. Am J Clin Dermatol 2002;3:319-28.
[Google Scholar]
|
| 2. |
Degitz K, Steidl M, Thomas P, Plewig G, Volkenandt M. Aetiology of tuberculids. Lancet 1993;341:239-40.
[Google Scholar]
|
| 3. |
Singh SK, Rai T. Papulonecrotic tuberculid in a patient with pulmonary tuberculosis. Indian Dermatol Online J 2014;5:72-3.
[Google Scholar]
|
| 4. |
Miller NR, Subramanian PS, Patel VR. Optic neuritis. In: Miller NR, Subramanian PS, Patel VR, editors. Walsh and Hoyt's Clinical Neuro-Ophthalmology the Essentials. 3rd ed. Baltimore: Lippincott Williams and Wilkins; 2016. p. 130-44.
[Google Scholar]
|
| 5. |
Singh PY, Sinha P, Baveja S, Sood A. Immune-mediated tuberculous uveitis – A rare association with papulonecrotic tuberculid. Indian J Ophthalmol 2019;67:1207-9.
[Google Scholar]
|
Fulltext Views
4,090
PDF downloads
1,428





