Translate this page into:
Papulonodular nonalopecic primary follicular mucinosis successfully treated with tacrolimus ointment
Corresponding author: Dr. Biswanath Behera, Department of Dermatology, All India Institute of Medical Sciences, Bhubaneswar, Odisha, India. biswanathbehera61@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Behera B, Manoharan P, Chandrashekar L, Gochhait D. Papulonodular nonalopecic primary follicular mucinosis successfully treated with tacrolimus ointment. Indian J Dermatol Venereol Leprol 2023;89:751-4
Dear Editor,
A 22-year-old man with skin phototype V presented with a 10-day history of multiple itchy facial skin lesions. He denied any topical application, drug intake, or photosensitivity . His systemic and family history were unremarkable. Cutaneous examination showed multiple skin-coloured to mildly erythematous papules and nodules on the face. Few nodules had mild scaling, and few were surrounded by areas of hypopigmentation [Figures 1a and 1b]. Differential diagnoses considered were Jessner lymphocytic infiltration of the skin, polymorphous light eruption, and lupus miliaris disseminatus faciei. Histology revealed moderate epidermal acanthosis, mucin deposition in the outer root sheath of the hair follicles, perivascular, perifollicular, and interstitial lymphohistiocytic infiltration, along with eosinophils. The hair follicles were preserved, and small to medium-sized lymphocytes showed no evidence of pleomorphism [Figure 2a-e]. The diagnosis of primary cutaneous follicular mucinosis was established, and he was treated with tacrolimus 0.1% ointment twice daily. After 1 month, all the lesions healed without any residual changes [Figures 3a and 3b], and he had no recurrence at 1-year follow-up.

- Multiple skin-coloured to mild erythematous papules and nodules on the face

- Multiple skin-coloured to mild erythematous papules and nodules on the face. Note the mild scaling and surrounding hypopigmented macule in a few lesions
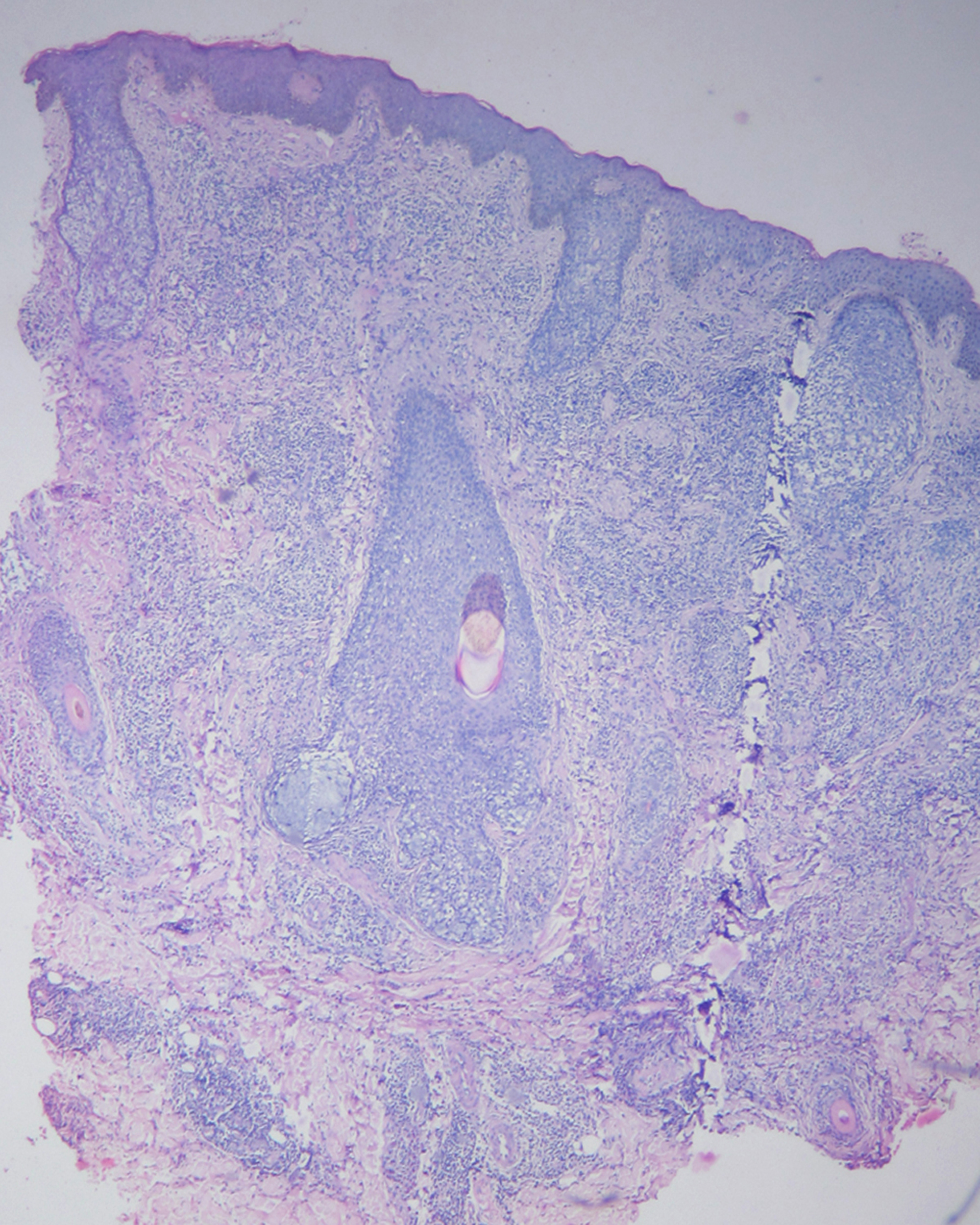
- Mild acanthotic epidermis, perivascular, perifollicular, and interstitial lymphohistiocytic infiltration. Note the absence of epidermal spongiosis (H & E, ×50)
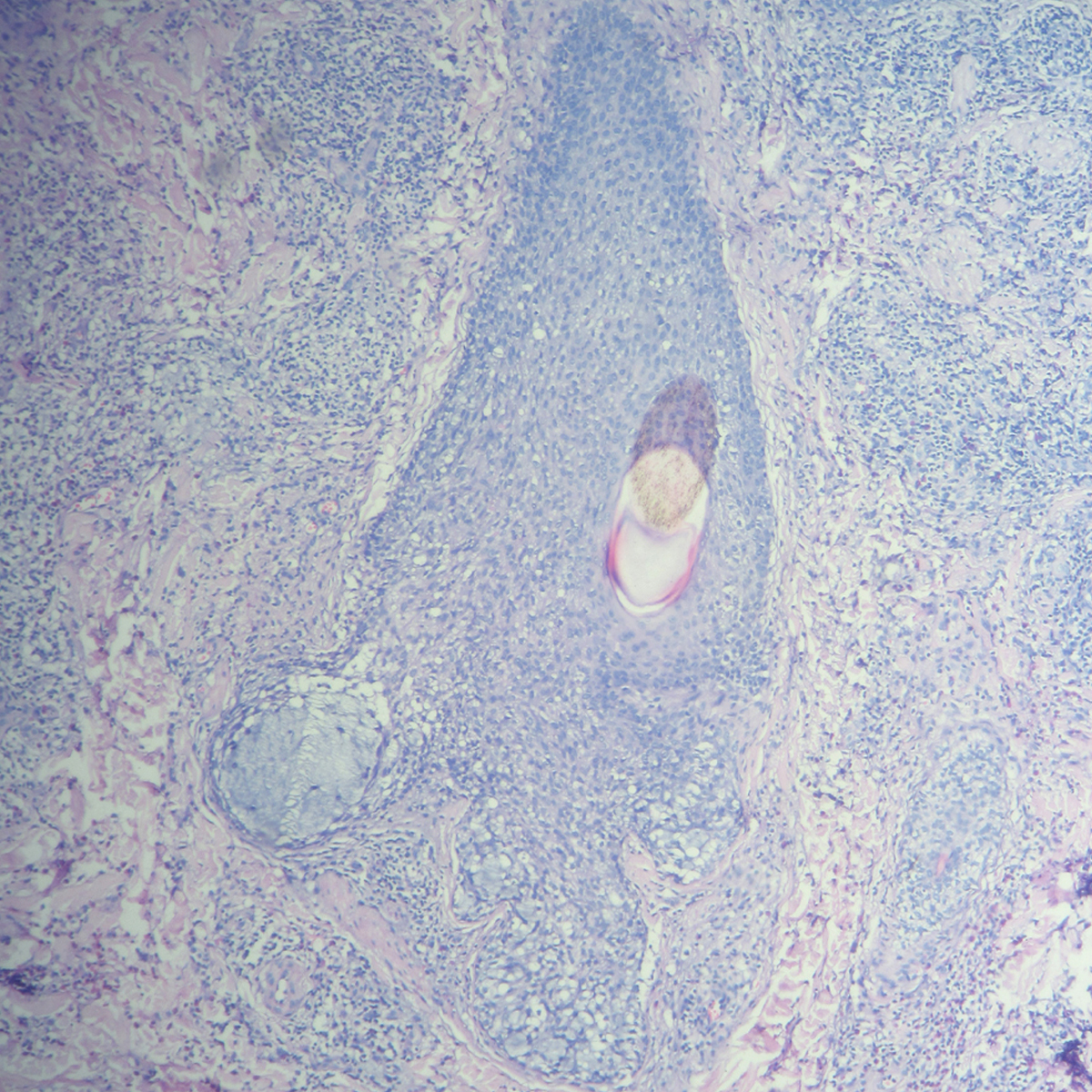
- Mucin within hair follicles and perivascular lymphohistiocytic and eosinophil infiltration (H & E , ×100)
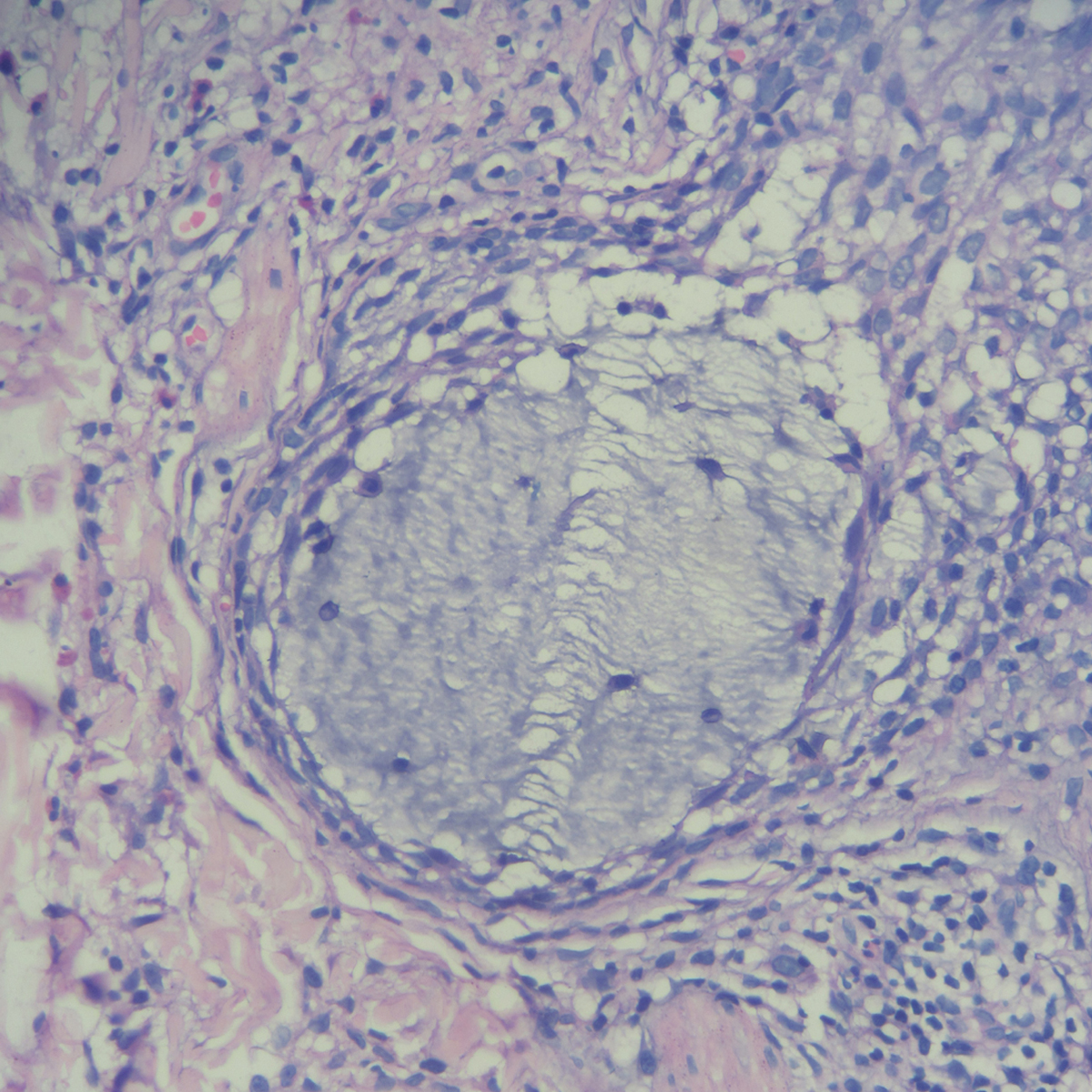
- Follicular mucin (H & E, ×400)
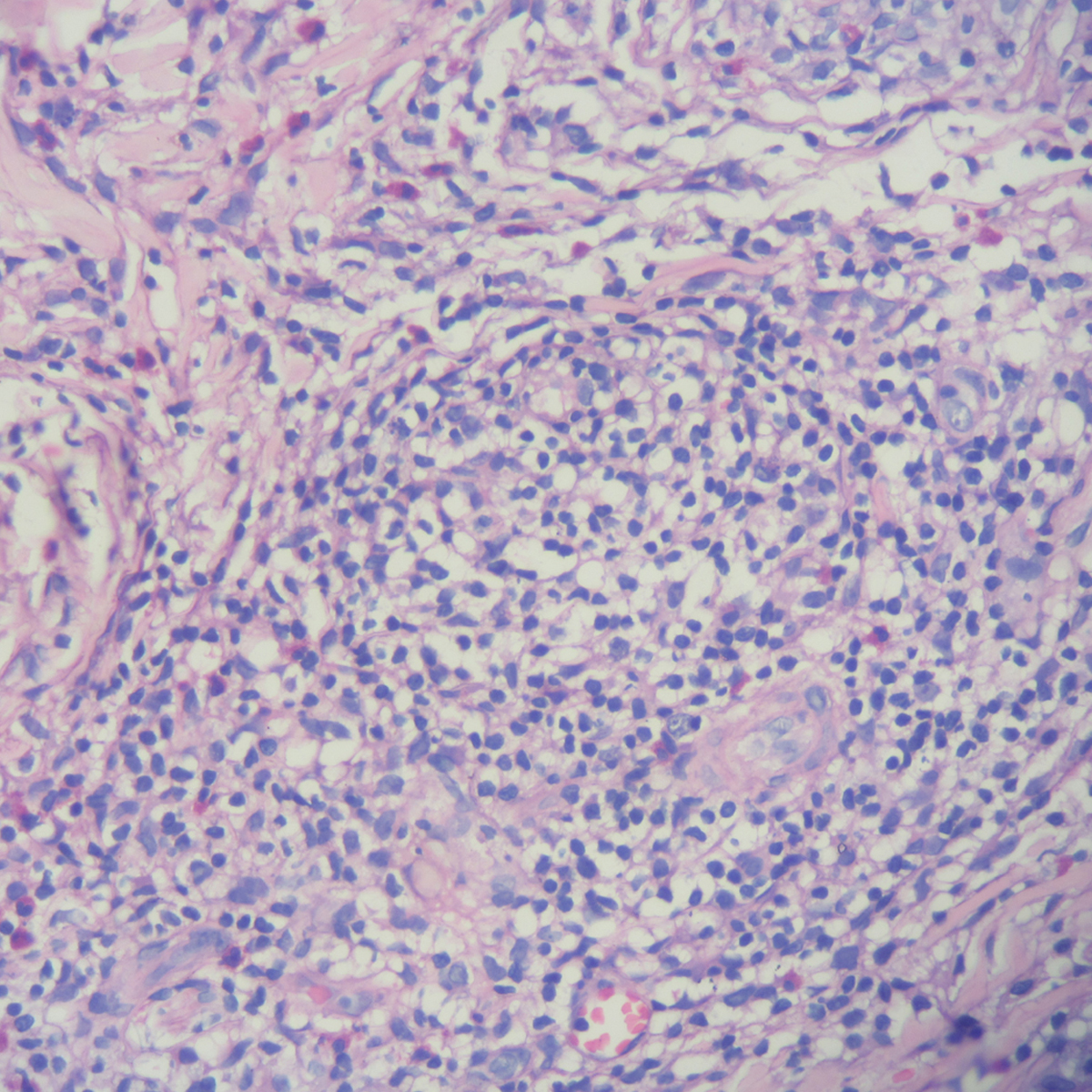
- Small to medium-sized lymphocytes without any evidence of atypia (H & E, ×400)

- A good number of eosinophils in the inflammatory infiltrate and sparing the hair follicle (H & E, ×400)

- Complete resolution of the papules and nodules

- Complete resolution of the papules and nodules without sequelae
Follicular mucinosis, a rare epithelial reaction pattern, results from mucin deposition in the hair follicle. Follicular mucinosis is broadly divided into two subtypes; primary and secondary. The former commonly occurs in children and young adults and has a benign clinical course. The latter is commonly associated with mycosis fungoides and Sezary syndrome and rarely with B-cell lymphoma, Hodgkin lymphoma, acute myelogenous leukemia, chronic myelomonocytic and lymphocytic leukemia, and adult T-cell leukemia-lymphoma. 1
Follicular mucinosis usually presents as an erythematous infiltrated or desquamative plaque with follicular prominence. It may or may not be associated with alopecia. An expression of mucin during clinical examination, called mucinorrhea, is an additional clue to the diagnosis. Head and neck are usually favoured locations. Other morphological variations of mycosis fungoides include hypopigmented, acneiform, urticarial, eczematous, cystic, and pregnancy-associated follicular mucinosis. 1–4 The diagnosis of follicular mucinosis is challenging in the absence of follicular prominence, alopecia and mucinorrhea, atypical morphology and unusual location.
Our case had an atypical presentation, with multiple skin-coloured to mild erythematous papules and nodules on the face. It can be easily mistaken for Jessner lymphocytic infiltration, lupus miliaris disseminatus faciei, granulomatous rosacea, granulomatous demodicosis, and lymphomatoid contact dermatitis. The absence of alopecia, follicular prominence, and mucinorrhea were further misleading. Hence the diagnosis of follicular mucinosis was not considered initially.
Demonstrating follicular mucin, intrafollicular lymphocytes, perifollicular lymphocytes, and eosinophils on histopathology, clinched the diagnosis of follicular mucinosis. Immunohistochemistry is needed to support the diagnosis of cutaneous T-cell lymphoma-associated follicular mucinosis, which shows an increased CD 4/CD 8 ratio and loss of CD 7 and CD 5. The presence of eosinophils indicate benign primary follicular mucinosis rather than follicular mycosis fungoides. 1
Treatment of follicular mucinosis is nonspecific and is determined by whether it is primary or secondary subtype. Response to therapy in primary follicular mucinosis is variable and can spontaneously resolve. The efficacy of various agents is limited. Various topical treatment options include corticosteroids, pimecrolimus, imiquimod, sulfacetamide, retinoids, bexarotene, and nitrogen mustard.
1
The presence of multiple lesions on the face prompted us to use tacrolimus instead of a topical corticosteroid. Tacrolimus is a calcineurin inhibitor that binds and blocks the enzyme calcineurin, which is required for the dephosphorylation of the nuclear factor of activated T cells. T cells have been linked to follicular mucinous degeneration. The mechanism of action, in this case, is possibly by inhibition of T cell activation and proliferation and the subsequent mucinous degeneration.
5
Side effects described for topical tacrolimus include local irritation, acne, rosacea-like dermatitis, and reactivation of human papillomavirus. Table 1 lists the cases of follicular mucinosis successfully treated with tacrolimus.
6–8
Our patient responded well to topical tacrolimus, and all the papulonodules resolved in 1 month without any adverse effects or recurrence.
Case report
Disease
Drug (%)
Time to complete remission
Kluk et al.
Follicular mucinosis
Tacrolimus (0.1) twice daily
4 weeks
Narayanan et al.
Follicular mucinosis
Tacrolimus (0.1)
2 months
Pérez-Elizondo et al.
Follicular mucinosis
Tacrolimus (0.1) twice daily
4 months
In conclusion, we describe a rare case of primary follicular mucinosis in a young adult who presented with multiple papulonodules on the face without alopecia and was successfully treated with topical tacrolimus without any sequelae.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
References
- Follicular mucinosis: A review. Int J Dermatol. 2021;60:159-165.
- [CrossRef] [PubMed] [Google Scholar]
- Primary follicular mucinosis in childhood. Int J Dermatol. 2021;60:e197-e199.
- [CrossRef] [PubMed] [Google Scholar]
- Erythematous scaly facial plaques with overlying hair loss. Indian J Dermatol Venereol Leprol. 2019;85:347.
- [Google Scholar]
- Idiopathic follicular mucinosis in childhood. An Bras Dermatol. 2020;95:268-270.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Follicular mucinosis treated with topical 0.1% tacrolimus ointment. Clin Exp Dermatol. 2014;39:227-228.
- [CrossRef] [PubMed] [Google Scholar]
- Erythematous scaly facial plaques with overlying hair loss. Indian J Dermatol Venereol Leprol. 2019;85:347.
- [Google Scholar]
- Primary follicular mucinosis: Presentation of a clinical case. Arch Inv Mat Inf. 2015;7:30-33.
- [Google Scholar]





