Translate this page into:
Partial unilateral lentiginosis with ipsilateral ocular involvement and seizures
2 Department of Pathology, All India Institute of Medical Sciences, New Delhi, India
Correspondence Address:
Binod K Khaitan
Department of Dermatology and Venereology, All India Institute of Medical Sciences, Ansari Nagar, New Delhi - 110 029
India
| How to cite this article: Gupta V, Taneja N, Khaitan BK, Singh M. Partial unilateral lentiginosis with ipsilateral ocular involvement and seizures. Indian J Dermatol Venereol Leprol 2019;85:130 |
Sir,
A 21-year-old, otherwise healthy female consulted us for asymptomatic, brown-colored “spotty” pigmentation on the right side of her face noticed 5 years back. Cutaneous examination showed multiple round-to-oval discrete, 0.1–0.5-cm sized, dark brown-colored macules distributed in the ophthalmic and maxillary divisions of the trigeminal nerve on the right-side of the face with a sharp midline demarcation [Figure - 1]a. There was no background pigmentation suggestive of a café-au-lait- macule. Eye examination revealed brown-colored macules on the bulbar conjunctiva of the right eye [Figure - 1]b. Conjunctiva on the left side, oral, and nasal mucosa were not affected. Dermoscopic examination of the pigmented macule under nonpolarized as well as polarized light (x10 magnification) showed an accentuated, regular, brown-colored pigment network [Figure - 2]. With the provisional clinical diagnosis of nevus of Ota and segmental lentiginosis, a skin biopsy from one of the pigmented macules was planned. During the biopsy procedure, the patient developed an episode of generalized tonic seizure lasting for less than a minute. The mother informed that she had been experiencing such transient episodes intermittently since the age of 10 years, but these were considered trivial and no medical consultation was ever sought. Histopathological examination showed accentuated epidermal basilar pigmentation with an increase in the number of melanocytes, consistent with a lentigo [Figure - 3]. No features of dermal melanocytosis were seen. A computerized tomographic scan of the brain, electroencephalogram, and ophthalmological examination were within normal limits. A final diagnosis of partial unilateral lentiginosis with ipsilateral ocular involvement was made. The patient was started on oxcarbazepine for seizures after neurological evaluation, and is being planned for Q-switched Nd: YAG laser for lentigines.
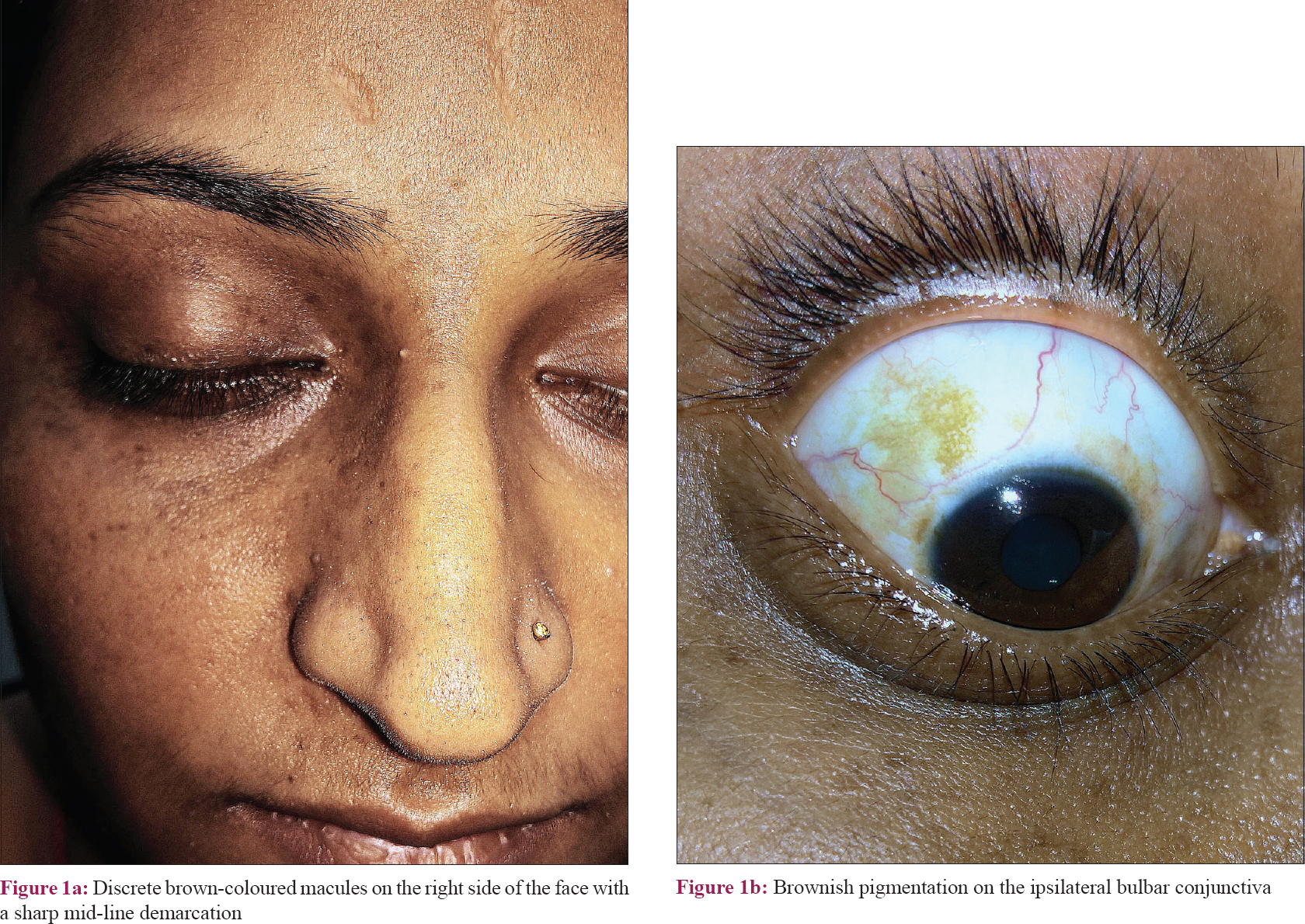 |
| Figure 1 |
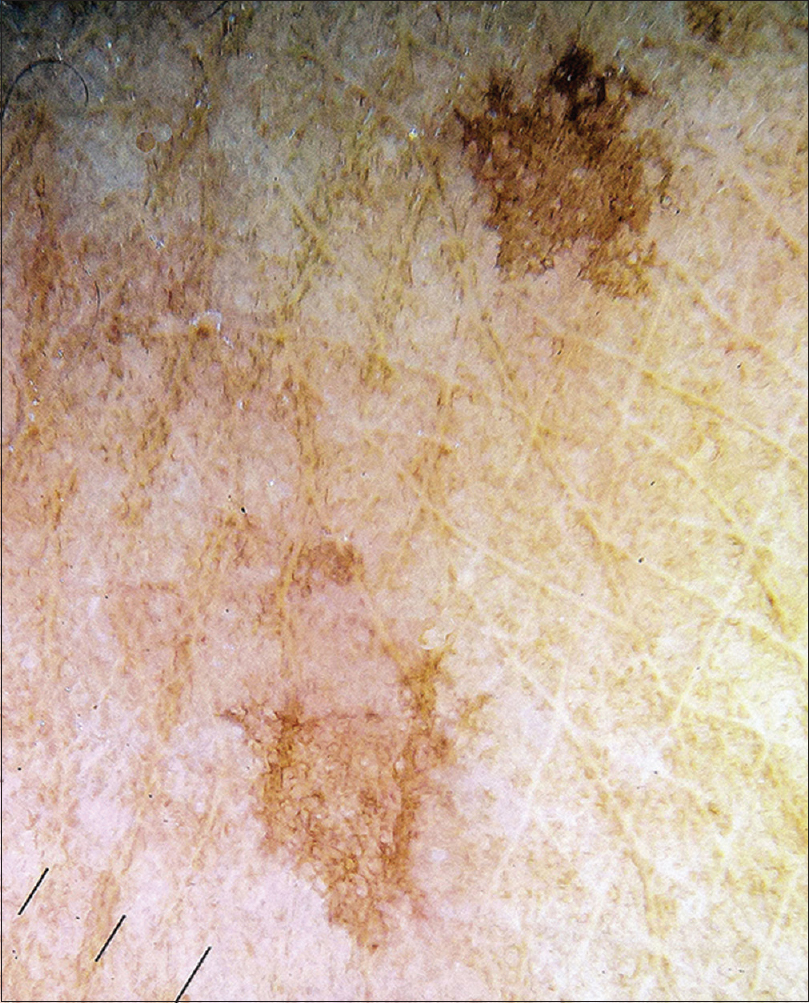 |
| Figure 2: Dermoscopic examination under non-polarized light showing an accentuated brown-coloured regular pseudoreticular pigment network |
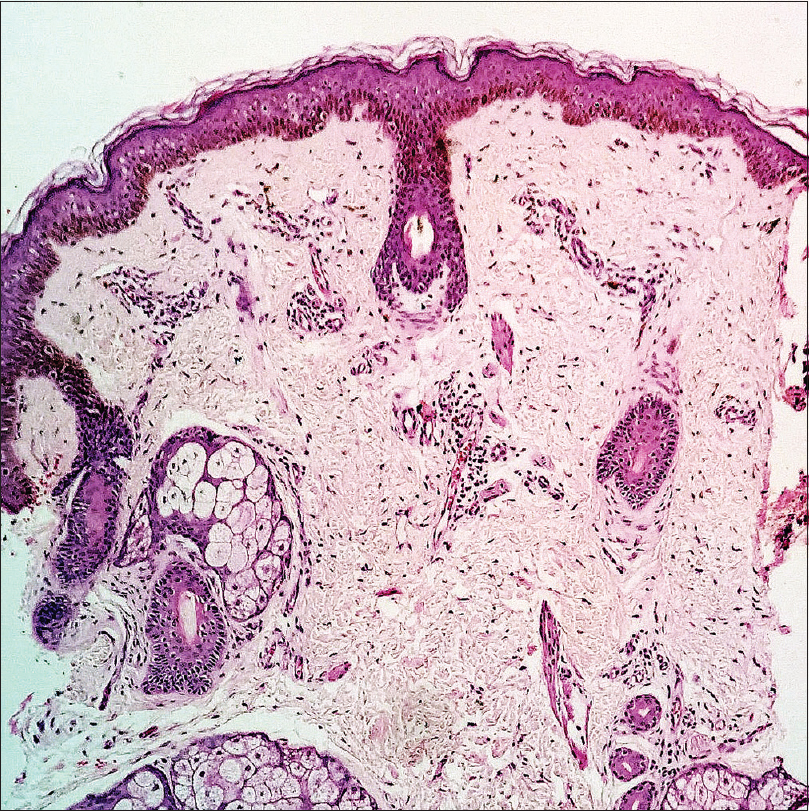 |
| Figure 3: Photomicrograph showing increased basilar pigmentation with an increase in the number of melanocytes (H and E, ×100) |
Partial unilateral lentiginosis is an unusual pigmentary disorder characterized by multiple lentigines clustered over a localized area with a sharp midline demarcation, usually confined to one or more dermatomes. The onset is usually in childhood, and any body site can be affected. When on the face, partial unilateral lentiginosis can be mistaken for nevus of Ota, especially if ocular pigmentation is present, like in our patient. Interestingly, ocular pigmentation has been reported in a few patients with partial unilateral lentiginosis as well.[1],[2],[3] However, unlike the mottled blue-gray pigmentation in nevus of Ota, the pigmentation in partial unilateral lentiginosis is brown-colored, both in the skin as well as the eye. Histopathology can distinguish between the two, showing features of lentigo in partial unilateral lentiginosis and dermal melanocytosis in nevus of Ota.
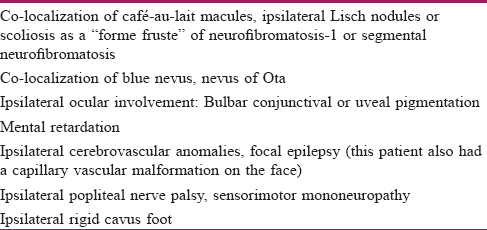
Central nervous system manifestations have been rarely reported in nevus of Ota and partial unilateral lentiginosis, though the association with nevus of Ota as meningeal melanocytomas and intracranial melanomas is more well-documented in the literature.[4] Our patient had brown-colored macules on one side of her face and ipsilateral bulbar conjunctiva and skin biopsy showed features of a lentigo. She also had a seizure disorder which had been so far unrecognized. There are only a few earlier cases of partial unilateral lentiginosis associated with central nervous system abnormalities. Schaffer et al.[1] reviewed previously reported cases of partial unilateral lentiginosis and their associations [Table - 1].[1],[3],[5] Though the majority of the reported “associations” were regarded as coincidental, central nervous system abnormalities were considered to have a possible association explained by a common developmental defect in the neural crest. We cannot be certain whether the seizures in our patient represent a true association or a mere coincidence. Nonetheless, we report this case to increase the awareness among dermatologists regarding the ocular involvement in partial unilateral lentiginosis, and its possible association with central nervous system abnormalities.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Schaffer JV, Lazova R, Bolognia JL. Partial unilateral lentiginosis with ocular involvement. J Am Acad Dermatol 2001;44:387-90.
[Google Scholar]
|
| 2. |
Kim EH, Kang HY. Partial unilateral lentiginosis with ocular involvement. Eur J Dermatol 2006;16:582-3.
[Google Scholar]
|
| 3. |
Serarslan G. Partial unilateral lentiginosis with ipsilateral ocular nevus. J Eur Acad Dermatol Venereol 2007;21:281-3.
[Google Scholar]
|
| 4. |
Franceschini D, Dinulos JG. Dermal melanocytosis and associated disorders. Curr Opin Pediatr 2015;27:480-5.
[Google Scholar]
|
| 5. |
González-Sixto B, De la Torre C, Posada C, Sevillano C. Partial unilateral lentiginosis associated with nevus of Ota. J Am Acad Dermatol 2010;63:353-5.
[Google Scholar]
|
Fulltext Views
2,161
PDF downloads
4,298





