Translate this page into:
Patterned cicatricial alopecia in two sisters with lamellar ichthyosis
Corresponding author: Dr. Keshavamurthy Vinay, Department of Dermatology, Venereology and Leprology, Postgraduate Institute of Medical Education and Research, Chandigarh, India. vinay.keshavmurthy@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Prarthana T, Mehta H, Saikia UN, Vinay K. Patterned cicatricial alopecia in two sisters with lamellar ichthyosis. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_1067_2024
Dear Editor,
Lamellar ichthyosis (LI) is a non-syndromic, autosomal recessive congenital ichthyosis (ARCI) primarily caused by mutations in the transglutaminase (TGM) 1 gene. It is characterised by plate-like scaling. While LI typically spares hair, nail and teeth development, it can lead to secondary nail dystrophy and scarring alopecia.
Two sisters in their thirties sought a dermatology consultation for the complaints of dryness and scaling all over their bodies since birth, and hair loss over the past four years. Upon examination, they exhibited widespread xerosis with large brown to grey scales, forming a polygonal pattern all over the body. Additionally, there was a noticeable recession of the frontal and retro-auricular hairlines with absent follicular opening and wrinkling, suggestive of scarring alopecia [Figure 1]. Further examination revealed sparse eyebrows, axillary, pubic and body hair. There were no abnormalities in nails or mucous membranes. There was a notable family history of similar lesions in two brothers and they had not received any treatment for their skin condition in the past.
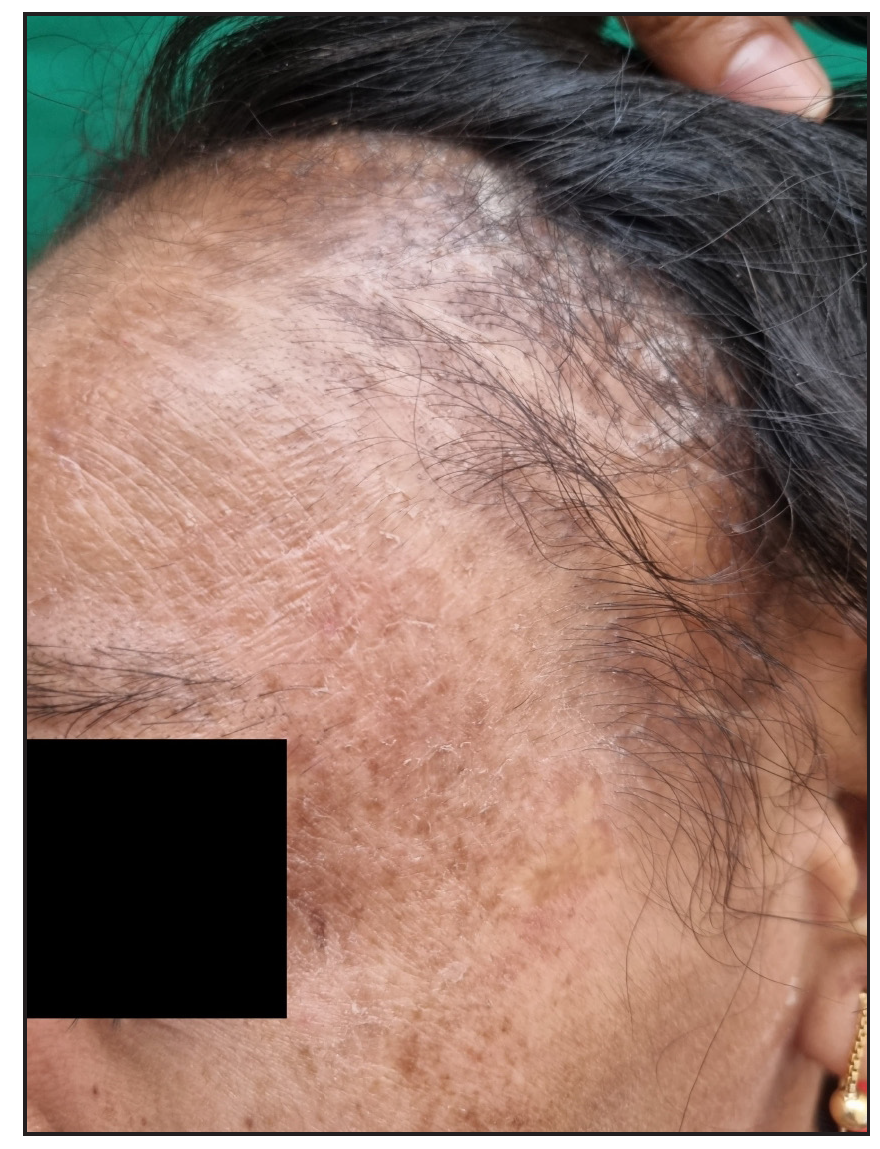
- Clinical images of a patient with lamellar ichthyosis showing recession of frontotemporal hairline with large polygonal brown scales.
The trichoscopic examination of the scalp showed loss of follicular ostia. At the progressive edges of alopecia, there was prominent perifollicular scaling, perifollicular pigmentation and interfollicular scaling. Moreover, there were numerous pigtail hairs and sparse vellus hairs [Figure 2a]. The trichoscopic examination of the axilla and pubic area showed a lack of follicular openings. The histopathological examination of the scalp biopsy revealed hyperkeratosis and acanthosis. In the dermis, there were hair follicles in the anagen phase accompanied by perifollicular fibrosis and lymphocytic inflammation [Figure 2b].
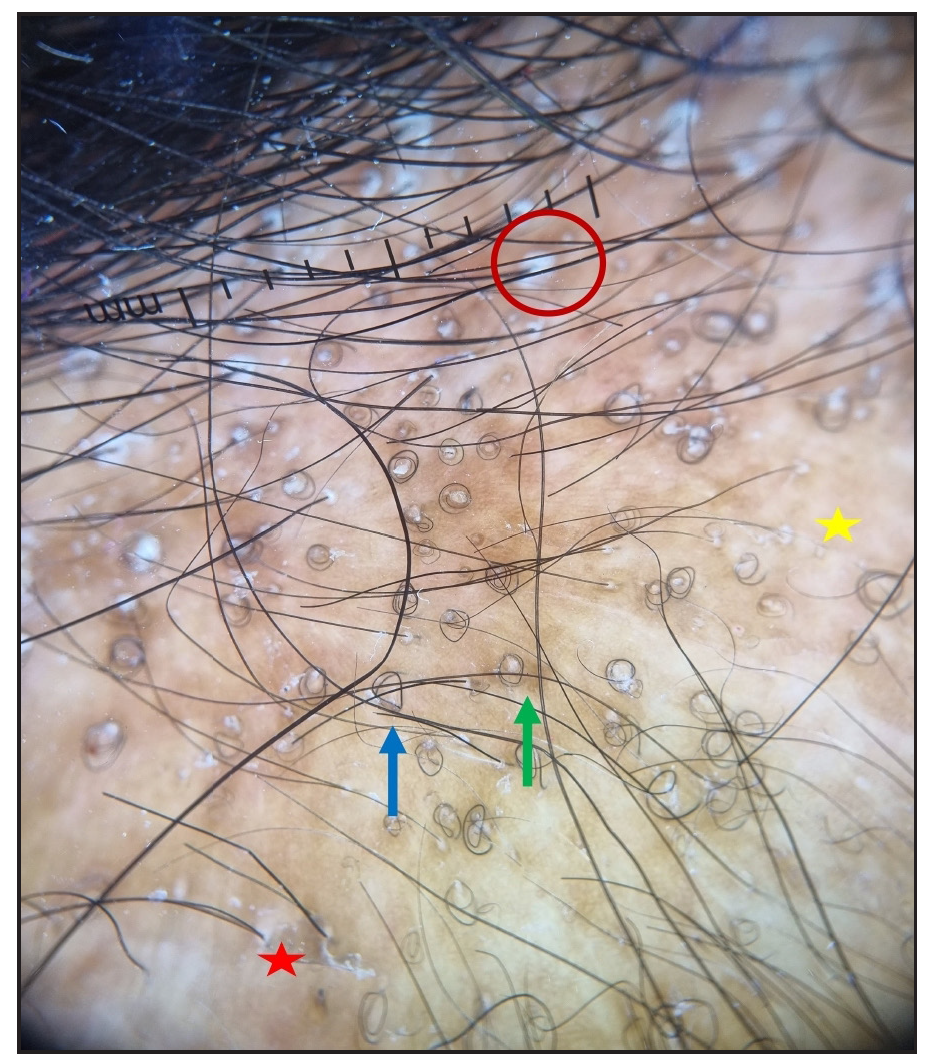
- Trichoscopic image (DermLite DL4, x10) showing perifollicular scale (red circle), coiled hairs (blue arrow), loss of follicular ostia (yellow star), perifollicular pigmentation (green arrow) and interfollicular scaling (red star).
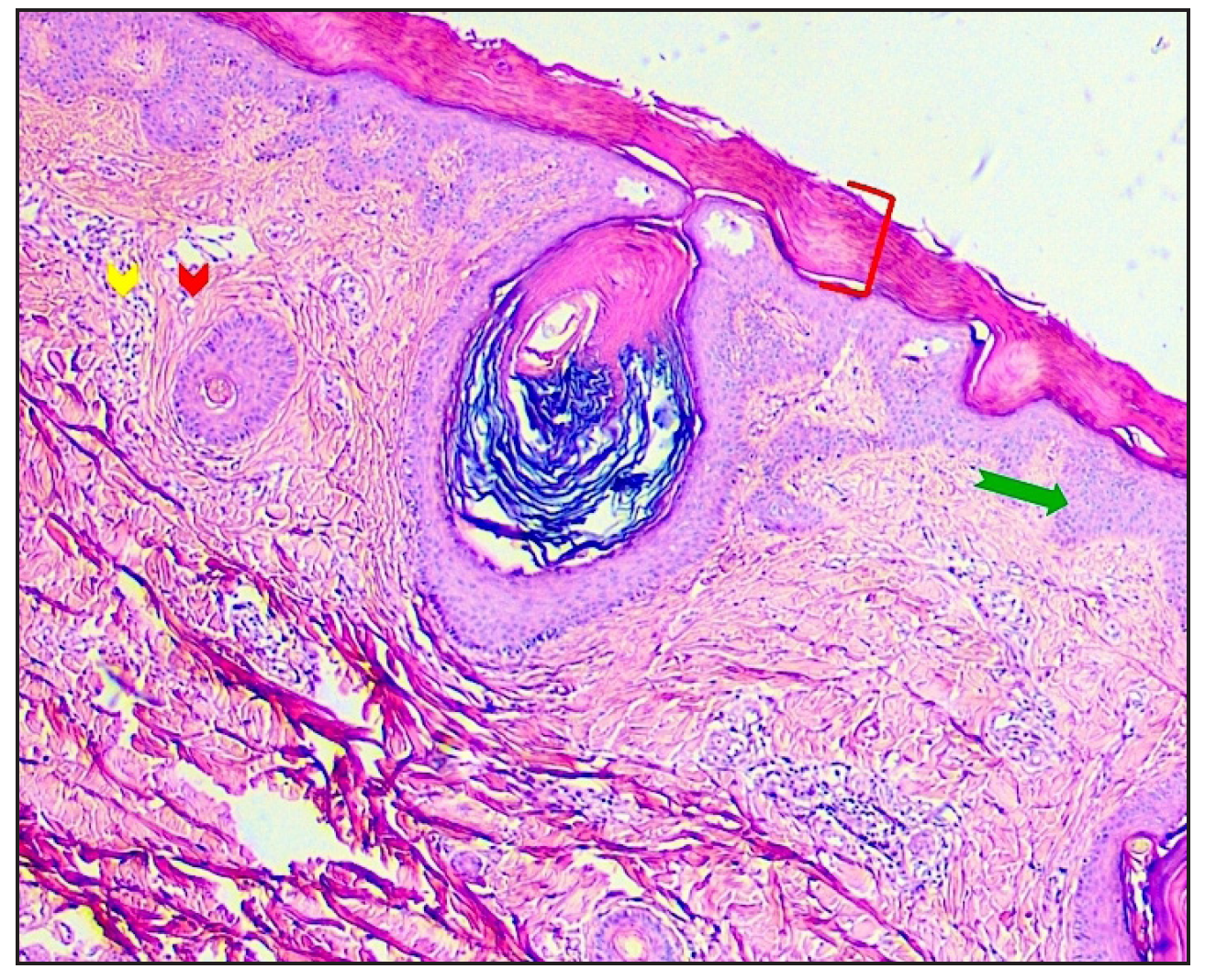
- Histopathological image of scalp biopsy (Haematoxylin and eosin stain, 40x magnification) showing hyperkeratosis (red bracket), acanthosis (green arrow) and spongiosis. Anagen hair follicles in the dermis are accompanied by perifollicular fibrosis (red arrowhead) and inflammation consisting primarily of lymphocytes (yellow arrowhead) with no interface activity.
Genetic sequencing revealed a mutation in the TGM1 gene, specifically identified as c.2087C>T p.(Thr696Met) missense mutation located in exon 13, classified as a pathogenic variant. Patients were treated with isotretinoin at 0.5 mg/kg/day, along with contraceptive counselling and emollients. After three months, scaling significantly reduced.
A patterned form of alopecia affecting the fronto-temporal scalp is increasingly recognised in LI patients. Many studies have investigated genotype-phenotype correlations in ARCI. TGM1 mutations are linked to alopecia in ARCI patients, with affected individuals over four times more likely to have these mutations.1,2 Putterman et al. found genotype-influenced hair loss severity, with ABCA12 or TGM1 mutations showing similar alopecia levels, whereas ALOX12B and NIPAL4 mutations were not associated with alopecia.3 However, these reports did not include a detailed morphological description of LI-associated alopecia. Challamel et al. described distinct alopecia patterns in LI patients, noting frontotemporal and retro-auricular hairline recession with TGM1 mutations.4 Dias et al. observed frontotemporal cicatricial alopecia in four ichthyosis patients, including three with LI.5 Our report on LI-associated alopecia explores extra-scalp patterns and histopathological findings. Accurate differentiation from conditions like FFA and Graham-Little Piccardi Lassueur syndrome is vital to avoid unnecessary immunosuppressant treatment [Table 1].6
| Characteristics | Scarring alopecia secondary to lamellar ichthyosis | Graham‐Little Piccardi Lassueur syndrome | Frontal fibrosing alopecia |
|---|---|---|---|
| Type | Secondary scarring alopecia | Primary (variant of LPP) | Primary (variant of LPP) |
| Age at presentation | 1st or 2nd decade of life | 30 to 70 years | >Postmenopausal |
| Gender | Men and women are equally affected | Women are 4 times more affected compared to men (4:1) | Women are affected more than men |
| Clinical presentation of alopecia | Progressive receding of frontotemporal hairline with large, polygonal brown scales | Patchy scarring alopecia of the scalp | Progressive symmetrical cicatricial alopecia in the frontotemporal area revealing a uniform shiny pale band of skin. Immediate hairline shows perifollicular erythema and scaling |
| Additional features | Ichthyosis, nail dystrophy | Non-scarring alopecia of axillary and pubic hair and widespread KP-like follicular papules | Thinning of eyebrows or loss may be seen |
| Dermoscopy | Reduced follicular ostia, perifollicular and interfollicular scaling, pili torti | Trichoscopy is similar to frontal fibrosing alopecia. Dermoscopy of follicular papules- round-to-oval yellowish areas with keratotic follicular plugs with mild erythema | Absence of follicular ostia. Presence of inflammatory signs such as perifollicular erythema, scaling and hyperkeratosis and lonely hairs. In skin of colour perifollicular pigment dots can also be seen |
| Histopathology | Hyperkeratosis, acanthosis and perifollicular lymphocytic infiltrate with no interface activity | Similar to LPP. Peri-infundibular and peri-isthmic lymphocytic inflammation and fibrosis, interface changes at infundibular-isthmic epithelium, increased hair in catagen and telogen phases, polytrichia | Similar to lichen planopilaris |
| DIF | Negative | Saggy or patchy deposition of fibrinogen and IgM along follicular BMZ | Non-specific, similar to lichen planopilaris |
| Pathogenesis | Mutation in TGM1 responsible for encoding TGase-1 enzyme, crucial for forming CCE within keratinocytes, catalysing cross-linking of Nε-(γ-glutamyl)lysine and ω-hydroxyceramides |
T cell-mediated autoimmune condition There is a decrease expression of PPAR |
A complex interaction between immune-mediated neurogenic inflammation, genetics, hormones, and possible external stimuli (Sunscreens, face soap), lack of PPAR-γ plays a vital role in all stages of disease |
| Management | Emollients / keratolytic, topical/oral retinoids, Vit D3 derivatives, genetic counselling | Same as frontal fibrosing alopecia | TCS, HCQ, Doxycycline, Finasteride, Pioglitazone, oral steroids, MTX, MMF, retinoids |
BMZ: basement membrane zone; CCE: cornified cell envelope; HCQ: hydroxychloroquine; KP: keratosis pilaris; LPP: lichen planopilaris; MTX: methotrexate; MMF: mycophenolate mofetil; PPAR: peroxisome proliferator‐activated receptor; TGM1: transglutaminase 1; TCS: topical corticosteroids.
The specific patterned alopecia seen in patients with TGM1 mutations strongly indicates a direct association between the TGM1 gene and hair follicle engagement. TGM1 produces the TGase-1 enzyme, vital for creating the cornified cell envelope in keratinocytes by facilitating the cross-linking of Nε-(γ-glutamyl)lysine and ω-hydroxyceramides. TGase-1 is found in different parts of normal hair follicles including cortex, medulla, outer and inner root sheath cells, aiding hair formation and potentially explaining alopecia in LI cases with TGM1 mutation.
In conclusion, we highlight the significance of recognising LI-associated patterned scarring alopecia, emphasising the importance of genotype-phenotype correlations, particularly concerning TGM1 mutations, in elucidating the pathogenesis of LI-related alopecia and guiding tailored therapeutic strategies.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Novel transglutaminase-1 mutations and genotype-phenotype investigations of 104 patients with autosomal recessive congenital ichthyosis in the USA. J Med Genet. 2009;46:103-11.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Autosomal recessive congenital ichthyosis in Sweden and Estonia: Clinical, genetic and ultrastructural findings in eighty-three patients. Acta Derm Venereol. 2003;83:24-30.
- [CrossRef] [PubMed] [Google Scholar]
- Association of the severity of alopecia with the severity of ichthyosis. JAMA Dermatol. 2019;155:1077-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Patients with autosomal recessive congenital ichthyosis present a distinctive pattern of alopecia. J Eur Acad Dermatol Venereol. 2023;37:e1274-6.
- [CrossRef] [PubMed] [Google Scholar]
- Lichenoid folliculitis of the scalp in four patients with ichthyosiform skin disorders and cicatricial alopecia. J Cutan Pathol. 2019;46:431-5.
- [CrossRef] [PubMed] [Google Scholar]
- What’s new in cicatricial alopecia? Indian J Dermatol Venereol Leprol. 2013;79:576-90.
- [CrossRef] [PubMed] [Google Scholar]





