Translate this page into:
Perianal warts and the development of squamous cell carcinoma in epidermodysplasia verruciformis
2 Family Medicine Clinic, Sisli State Hospital, Istanbul, Turkey
Correspondence Address:
Hilal Kaya Erdogan
Department of Dermatology, Sisli Etfal Training and Research Hospital Istanbul, 34377
Turkey
| How to cite this article: Kivanc-Altunay I, Erdogan HK, Kayaoglu S. Perianal warts and the development of squamous cell carcinoma in epidermodysplasia verruciformis. Indian J Dermatol Venereol Leprol 2011;77:112 |
Sir,
Epidermodysplasia verruciformis (EV) is a rare, inherited disorder that predisposes patients to chronic widespread human papillomavirus (HPV) infection. [1] Typical lesions are notably variable with pityriasis versicolor-like macules, wart-like flat papules, psoriasiform red papules, pigmented keratotic lesions resembling seborrheic keratosis. Wart-like lesions or atypical warts caused by HPV are especially important, because skin cancers may develop on sun-exposed areas such as the back of hands, neck and the legs. The genital areas are rarely involved and HPV lesions on this area have been previously reported only twice. [2],[3] As far as we know, concurrent perianal HPV infection has not been reported to date.
A 37-year-old man presented with a verrucous mass on the perianal region that has enlarged for over 4 years. He had been operated twice for this mass during these 4 years, but the recurrence of painful lesions had occurred after each operation. On admission, it was also apparent that the patient had numerous red and brown maculopapular lesions on his face and dorsum of hands. These lesions existed for about 25 years and he did not complain about them. Examination of all systems was normal. His medical history was unremarkable except for smoking for 20 years. Homosexual history was not obtained. The patient did not have any medications and denied a family history of any skin diseases. Dermatological examination revealed multiple tan brown-colored maculopapular lesions on the face [Figure - 1]a and neck, verrucous-hyperkeratotic papules and plaques on the hands and forearms, verrucous lesions on the perianal region [Figure - 1]b. Some of the finger and toe nails were also hyperkeratotic. Routine laboratory tests including hematological and biochemical analyses of blood and urine were within normal limits. VDRL, TPHA and HIV serology results were all negative. HPV phenotyping was performed by polymerase chain reaction from perianal region and HPV type 53 with high oncogenic potential was detected. Genetic study was not done in our case. Two punch biopsies were performed from forearm and perianal regions. Histology of the forearm lesions revealed hyperkeratosis, papillomatosis, hypergranulosis, koilocytic changes in upper spinous layer and perivascular mononuclear cell infiltration in papillary dermis [Figure - 2]a. Perianal biopsy showed dyskeratosis in epidermis, papillomatosis, loss of polarity, hyperchromatic nuclei, pleomorphism, koilocytic atypical cells which were consistent with condyloma accuminatum with high-grade squamous cell carcinoma (SCC) [Figure - 2]b. Surgical excision was planned for perianal mass. Post-operative pathological examination confirmed previous diagnosis of SCC. Although total excision provided a cure for cancer, post-operative radiotherapy was additionally planned for regional control of the cancer. The patient is now on follow-up.
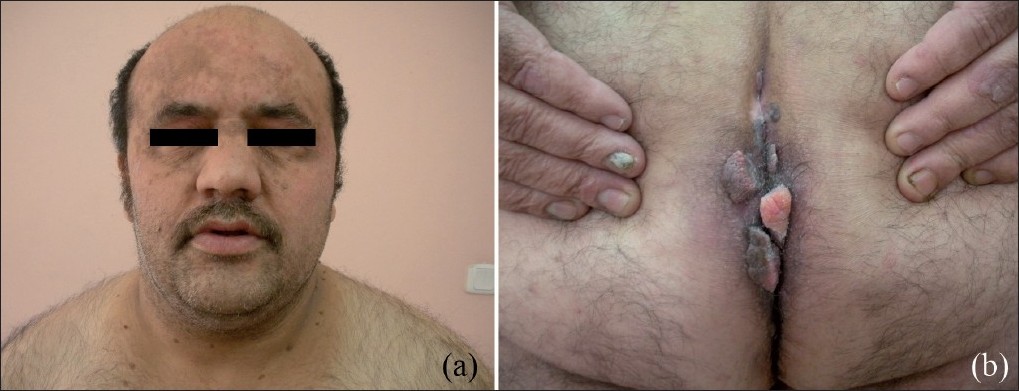 |
| Figure 1: (a) Red and brown maculopapular lesions on the face. (b) Verrücous lesions on anogenital region |
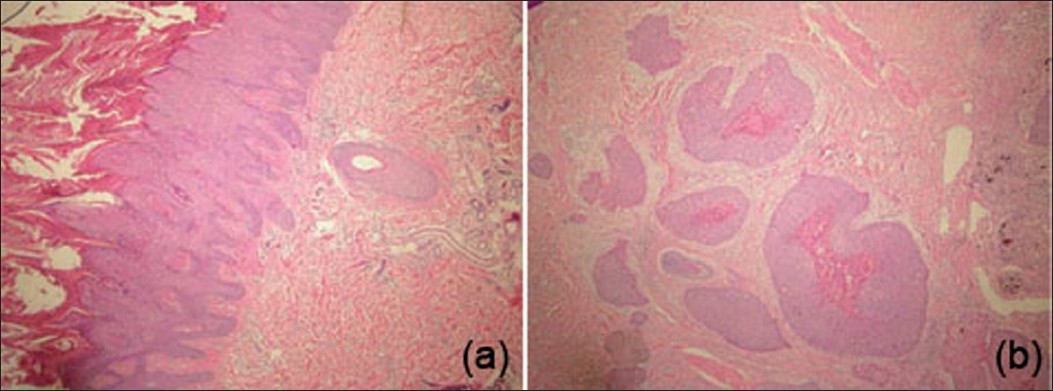 |
| Figure 2: (a) Hyperkeratosis, papillomatosis, hypergranulosis, koilocytic changes in upper spinous layer and perivascular mononuclear cell infiltration in papillary dermis (H and E, ×40). (b) Invasive, well-differentiated squamous cell carcinoma (H and E, ×40) |
EV was first described by Lewandowsky and Lutz in 1922 as an epidermal nevus. [3] It is a rare, autosomal recessive genodermatosis that predisposes patients to widespread HPV infection that do not regress due to unique susceptibility to spesific HPV types. Lesions typically have either the appearance of flat warts or flat, scaly, red-brown macules that resemble lesions of pityriasis versicolor. [1] The localizations of the lesions are predominantly sun-exposed areas such as the face, neck and dorsa of the hands. However, genital warts involving scrotum, penis may also rarely occur. There are only two reports of genital localizations of wart-like lesions. [2]
Malignant transformation as non-melanoma skin cancers occurs in approximately 30-50% of patients, predominantly on sun-exposed areas and rarely on non-sun-exposed skin. The high transformation rate in sun-exposed areas could be explained by the chronic ultraviolet B exposure and the probable presence of oncogenic EV-HPV in hair follicles. [4] The exact molecular pathway between EV-HPV and development of non-melanoma skin cancer, however, remains unclear . Development of SCC in non-sun-exposed area in our case can be explained by oncogenic potential of HPV type 53. [1]
Malignancies are commonly associated with HPV types 5 and 8 in around 90% of cases, and much less frequently with types 9, 12, 14, 17, 20 and 47, as non-melanoma skin cancers which are usually multiple, locally invasive and rarely metastatic. [5] There is a recent case report in which HPV 22 b was found to be accountable for the development of an aggressive SCC. [6] Our case is interesting in two ways. First is the development of perianal warts which is unusual localization for warts in EV and second is the role of HPV type 53 in the occurrence of SCC. As far as we know, HPV type 53 has never been previously reported in EV. Therefore, one should also pay attention to the warts on non-sun-exposed areas for possible malignant transformation in EV.
| 1. |
Gül U, Kiliç A, Gönül M, Cakmak SK, Bayis SS. Clinical aspects of epidermodysplasia verruciformis and review of the literature. Int J Dermatol 2007;46:1069-72.
[Google Scholar]
|
| 2. |
Sanclemente G, García JJ, Gómez LF, Tyring SK, Wolff JC, Correa LA, et al. An unusual presentation of human papillomavirus (HPV) infection in a black epidermodysplasia verruciformis (EV) patient. Int J Dermatol 2007;46:199-201.
[Google Scholar]
|
| 3. |
Bogdan I, Schärer L, Rüdlinger R, Hafner J. Epidermodysplasia verruciformis in two brothers developing aggressive squamous cell carcinoma.Dermatol Surg 2007;33:1525-8.
[Google Scholar]
|
| 4. |
De Oliveira WR, Festa Neto C, Rady PL, Tyring SK. Clinical aspects of epidermodysplasia verruciformis. J Eur Acad Dermatol Venereol 2003;17:394-8
[Google Scholar]
|
| 5. |
Al Rubaie S, Breuer J, Inshasi J, Al Saady S, Fathi I. Epidermodysplasia verruciformis with neurological manifestations. Int J Dermatol 1998;37:766-71.
[Google Scholar]
|
| 6. |
Kim T, Park JC, Roh MR, Park JM, Kim SH, Cho NH, et al. Development of Aggressive Squamous Cell Carcinoma in Epidermodysplasia Verruciformis Associated with Human Papillomavirus Type 22b. Dermatology 2010;220:326-8.
[Google Scholar]
|
Fulltext Views
1,991
PDF downloads
2,606





