Translate this page into:
Periocular lupus vulgaris secondary to lacrimal sac tuberculosis: A rare presentation with emphasis on magnetic resonance imaging in localizing the primary focus of infection
2 Department of Radiodiagnosis, Maulana Azad Medical College and Lok Nayak Hospital, New Delhi, India
Correspondence Address:
Bijaylaxmi Sahoo
Department of Dermatology, Maulana Azad Medical College and Lok Nayak Hospital, New Delhi
India
| How to cite this article: Bansal S, Sahoo B, Garg VK, Singh S. Periocular lupus vulgaris secondary to lacrimal sac tuberculosis: A rare presentation with emphasis on magnetic resonance imaging in localizing the primary focus of infection. Indian J Dermatol Venereol Leprol 2013;79:425-427 |
Sir,
Atypical presentations of lupus vulgaris have infrequently been reported in the literature, and so are the complications resulting from delayed diagnosis and inappropriate therapy. [1],[2],[3] Periocular lupus vulgaris is an uncommon form where delayed and inappropriate treatment can lead to significant disfigurement and morbidity. [3] The mode of acquisition in most of the cases is either through hematogenous spread from an infected pulmonary focus or less commonly due to direct inoculation of bacilli. However, lupus vulgaris occurring secondary to infection of the ocular adnexa has not been reported before. We report two cases of periocular lupus vulgaris secondary to tubercular dacryocystitis, which is exceedingly rare. Problems in diagnosis and management have also been discussed.
Patient 1 was a 46-year-old female who presented to our tertiary hospital with epiphora in right eye for 1 year and purulent discharge from the medial canthus for 8 months. The symptoms persisted in spite of repeated drainage of sac and multiple courses of antibiotics. After a month of failed treatment, she noticed a reddish-brown raised asymptomatic lesion on the site of discharge for which she was referred to our dermatology outpatient department. She did not show any history of nasal obstruction or altered vision.
On examination, there was a single 2 × 1.5 cm reddish-brown plaque located in the region of right lacrimal sac with appreciable epiphora in the same eye [Figure - 1]. There was no pre-auricular or cervical lymphadenopathy. Direct and endoscopic examinations of the nasal cavity did not reveal any abnormality.
 |
| Figure 1: (a) Pre - treatment photograph of patient 1 showing the lupus vulgaris lesion near right medial canthus and (b) 2 months post-treatment photograph of the same patient showing a small hyperpigmented scar at the site of lesion |
The tuberculin skin test (carried out with 1 TU of purified protein derivative and read after 72 h) was strongly positive with an induration of 35 mm. Histopathological examination of the skin lesion revealed multiple non-caseating epithelioid cell granulomas with Langhans giant cells located in the superficial and mid-dermis [Figure - 2]. Magnetic resonance imaging (MRI) of the orbit showed a 0.9 cm × 1 cm lobulated area of altered signal intensity within the medial extraconal compartment of the right orbital globe in the region of right lacrimal sac suggestive of an inflammatory pathology. There was no focus of tuberculosis elsewhere in the body.
 |
| Figure 2: (a) Histological section from the skin lesion of patient 1 showing multiple non - caseating epithelioid cell granulomas (arrow) in superficial and mid - dermis (H and E, ×100), (b) higher magnification showing multinucleated Langhans giant cell (arrow) along with epithelioid cells and lymphocytes (H and E, ×400) |
Patient 2 was a 30-year-old male presented with history of epiphora in right eye for 8 months. A month later, he noticed a reddish-brown raised asymptomatic lesion near the right medial canthus, which progressively increased in size over a period of 2 months.
Cutaneous examination revealed a 5.5 × 2.5 cm reddish-brown plaque occupying the right medial canthus, right infraorbital region, and part of the upper eyelid [Figure - 3]. There was no significant lymphadenopathy. Direct and endoscopic examinations of the nasal cavity were normal.
The tuberculin skin test was strongly positive (28 mm induration). Histopathological examination revealed ill-defined epithelioid cell granulomas in the superficial dermis. MRI of the orbit showed thickening of skin and subcutaneous tissue along with a heterogeneously hyperintense signal in the region of right lacrimal sac and nasolacrimal duct [Figure - 4].
 |
| Figure 3: (a) Pre - treatment photograph of patient 2 showing the lupus vulgaris lesion near right medial canthus, (b) 2 months post-treatment photograph of the same patient showing an atrophic scar at the site of lesion |
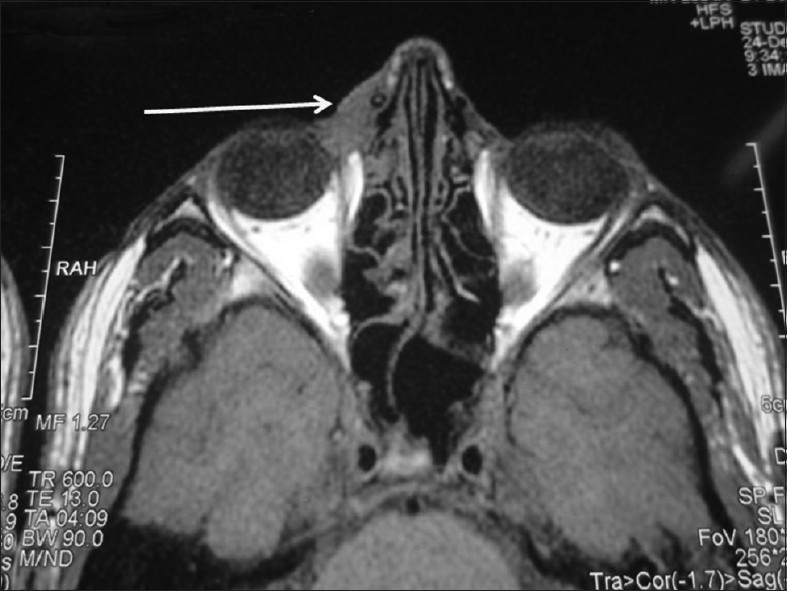 |
| Figure 4: Magnetic resonance imaging (orbit) of patient 2 showing thickening of skin and subcutaneous tissue in the region of medial canthus and a heterogeneously hyperintense signal in region of right lacrimal sac and nasolacrimal duct |
Both the patients were commenced on category I anti-tubercular treatment (2 HRZE + 4 HR). Two months following therapy, we observed complete resolution of the skin lesion and significant improvement in the epiphora [Figure - 1] and [Figure - 3]. An endoscopic dacryocystorhinostomy had to be done in the 1 st patient to cure the persisting epiphora, whereas the 2 nd patient is yet to complete his 6 months of treatment.
Tuberculosis of the orbit is an uncommon form of extrapulmonary tuberculosis. Tubercular infection of the ocular adnexa (lacrimal sac and nasolacrimal duct) and the overlying skin is very rare. A thorough search of the existing literature revealed eight case reports of nasolacrimal tuberculosis. [4],[5],[6] However, to the best of our knowledge, lupus vulgaris developing secondary to lacrimal sac tuberculosis has not been described in the literature.
The disease can occur either as a primary infection of the lacrimal sac or secondary to infection of the nasolacrimal duct which is more common. Since there was no demonstrable focus on endoscopic examination of the nasal cavity, nor elsewhere in the body, we assume that it was a primary infection of the lacrimal sac in our case.
The initial presentation in most cases of nasolacrimal tuberculosis is a non-specific symptom like epiphora which was also the presenting symptom in both our patients. This explains the time delay of up to 3 years between the onset of symptoms and diagnosis in most of the previous reports on nasolacrimal tuberculosis. [4],[6] Delay in diagnosis and treatment can lead to extension of the infectious process to intraocular tissues, causing severe visual impairment. The appearance of cutaneous lesion in our patients helped us to clinch the correct diagnosis relatively early, thus minimizing morbidity to the patients. Moreover, the use of MRI technique helped us to localize the site of infection in the lacrimal sac without any invasive exploratory surgery. Whereas, in almost all the previous studies, some form of invasive surgery had to be done to confirm the primary site of pathology. [5],[6]
Although other causes of epiphora such as trauma, tumors in the nasal cavity, conjunctivitis, and other infectious processes should also be kept in mind, the presence of cutaneous lesion in both our cases, along with high endemicity suggested tuberculosis as the most likely possibility.
The cases demonstrate an unusual presentation of orbital and secondary cutaneous tuberculosis. It also highlights the importance of keeping a high index of suspicion in such cases especially in endemic areas so that the appropriate therapy can be administered at the earliest. We recommend the use of non-invasive techniques like MRI to localize the primary site of infection so that unnecessary surgical intervention can be avoided.
| 1. |
Chowdhury MM, Varma S, Howell S, Holt PJ, Statham BN. Facial cutaneous tuberculosis: An unusual presentation. Clin Exp Dermatol 2000;25:48-50.
[Google Scholar]
|
| 2. |
Khandpur S, Reddy BS. Lupus vulgaris: Unusual presentations over the face. J Eur Acad Dermatol Venereol 2003;17:706-10.
[Google Scholar]
|
| 3. |
El-Ghatit AM, El-Deriny SM, Mahmoud AA, Ashi AS. Presumed periorbital lupus vulgaris with ocular extension. Ophthalmology 1999;106:1990-3.
[Google Scholar]
|
| 4. |
Cotton JB, Ligeon-Ligeonnet P, Durra A, Sartre J, Bureau E, Chetail N, et al. Tuberculous dacryocystitis. Arch Pediatr 1995;2:147-9.
[Google Scholar]
|
| 5. |
Wong SC, Healy V, Olver JM. An unusual case of tuberculous dacryocystitis. Eye (Lond) 2004;18:940-2.
[Google Scholar]
|
| 6. |
Jablenska L, Lo S, Uddin J, Toma A. Nasolacrimal tuberculosis: Case report highlighting the need for imaging in identifying and managing it effectively. Orbit 2010;29:126-8.
[Google Scholar]
|
Fulltext Views
3,054
PDF downloads
2,424





