Translate this page into:
Periorbital melanosis is an extension of pigmentary demarcation line-F on face
Correspondence Address:
Subrata Malakar
Rita Skin Foundation, GD 381 Salt Lake, Kolkata - 700 106
India
| How to cite this article: Malakar S, Lahiri K, Banerjee U, Mondal S, Sarangi S. Periorbital melanosis is an extension of pigmentary demarcation line-F on face. Indian J Dermatol Venereol Leprol 2007;73:323-325 |
Abstract
Background: To date, periorbital melanosis is an ill-defined entity. The condition has been stated to be darkening of the skin around the eyes, dark circles, infraorbital darkening and so on. Aims: This study was aimed at exploring the nature of pigmentation in periorbital melanosis. Methods: One hundred consecutive patients of periorbital melanosis were examined and investigated to define periorbital melanosis. Extent of periorbital melanosis was determined by clinical examination. Wood's lamp examination was performed in all the patients to determine the depth of pigmentation. A 2-mm punch biopsy was carried out in 17 of 100 patients. Results: In 92 (92%) patients periorbital melanosis was an extension of pigmentary demarcation line over the face (PDL-F). Conclusion: Periorbital melanosis and pigmentary demarcation line of the face are not two different conditions; rather they are two different manifestations of the same disease.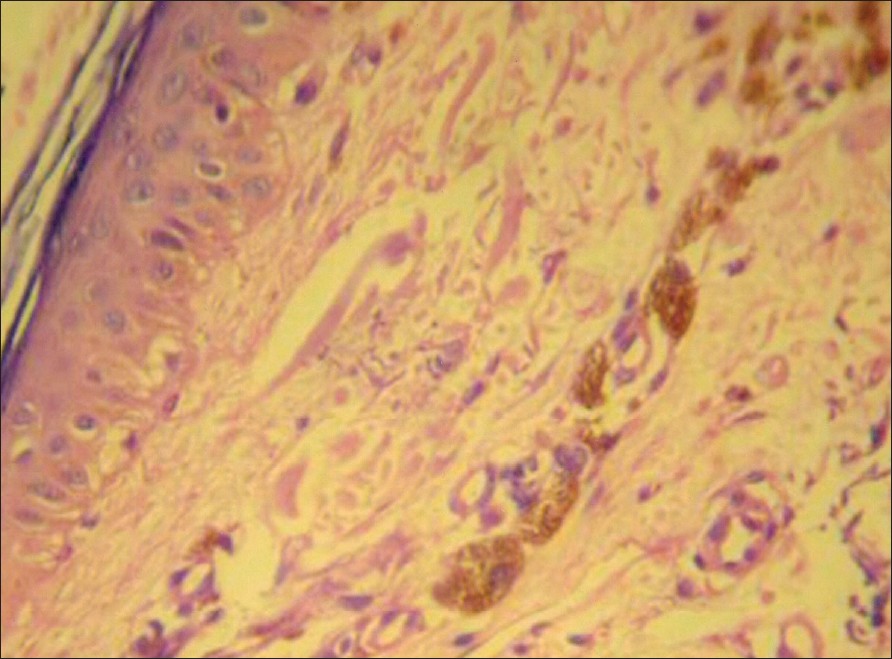 |
| Figure 4: Histopathology from POM showing melanophages in the upper dermis (H and E stain, X400) |
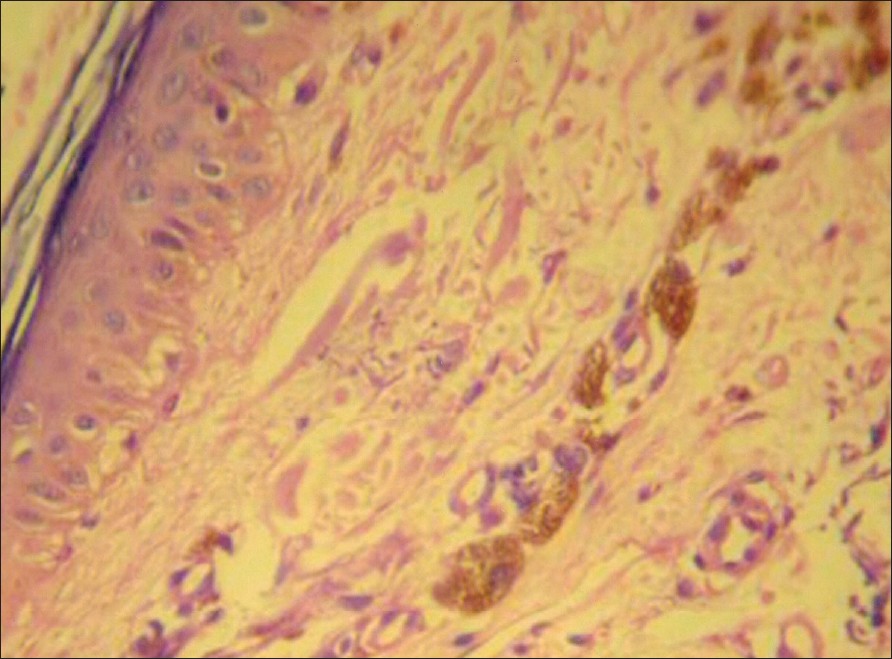 |
| Figure 4: Histopathology from POM showing melanophages in the upper dermis (H and E stain, X400) |
 |
| Figure 3: Periorbital melanosis and pigmentary demarcation line over the face in mother and daughter |
 |
| Figure 3: Periorbital melanosis and pigmentary demarcation line over the face in mother and daughter |
 |
| Figure 2: Same patient as in Figure 1. Turning of the face reveals a hyperpigmented patch on the side of the face with a sharp border (PDL-F). Pigmentary demarcation line-F continued as POM around the eye |
 |
| Figure 2: Same patient as in Figure 1. Turning of the face reveals a hyperpigmented patch on the side of the face with a sharp border (PDL-F). Pigmentary demarcation line-F continued as POM around the eye |
 |
| Figure 1: Periorbital melanosis, uniform hyperpigmented patch around the eyes |
 |
| Figure 1: Periorbital melanosis, uniform hyperpigmented patch around the eyes |
Introduction
Periorbital melanosis (POM) is an ill-defined entity and is a common cosmetic concern. It is popularly known as "dark circles" [1] and has also been referred to as "infraorbital skin discoloration," [2] "infraorbital darkening" [1] and "some darkening of the skin around the eyes." [3] There has been little investigation as to the cause of this common disorder; consequently, varied methods of treatment have been carried out with variable outcomes.
POM has been stated to result from a variety of reasons; [2] they include dermal melanin deposition, post inflammatory hyperpigmentation from atopic or contact allergic dermatitis as well as shadowing from lax skin and infraorbital swelling. Pigmentary demarcation lines (PDL) are sharp demarcation lines present over the different parts of the body. [4] Thus far, six demarcation lines have been described and given names according to the alphabets A to F. [5] Recently two more PDLs have been described in the Indian population. [6] This study explores the relationship between POM and PDL-F by clinical and histopathological parameters.
Methods
Patients
One hundred consecutive patients of periorbital melanosis attending the outdoor clinic of Rita Skin Foundation constituted the sample population. History of onset, affected family members and triggering factors of POM were noted. All the patients were examined under Wood′s lamp to determine the depth of pigmentation. Histopathological examination was possible in 17 patients. Biopsies were formalin fixed, paraffin embedded and stained with hematoxylin and eosin. In each of all the 17 patients, biopsies were taken from POM (hyperpigmented patch around the eyelids) and PDL-F (pigmentary demarcation line of the face) of the same side.
Photographs
Different views of the face of the patient were taken such as the front view [Figure - 1] and an oblique view [Figure - 2].
Close inspection
All patients of the sample population complaining of periorbital melanosis were inspected closely. They were inspected from front [Figure - 1], first, by keeping their eyes open and then closed. Their faces were then turned to the same side [Figure - 2] to find out PDL-F; if present, it was observed for its extension, intensity of color and pattern. The area was inspected further to reveal the boundary of the periorbital melanosis and that of the pigmentary demarcation line of the face and their relation, if any.
Results
Among 100 patients, 88 were female and 12 male. In 61 patients the POM started during adulthood; in 32 cases, it started at puberty (between 11 and 13 years of age); while it started during childhood in 7 patients. POM was the complaint in all the patients but while turning to the side of the face another condition known as PDL-F [Figure - 2],[Figure - 3] was noticed in 92% cases.
Periorbital melanosis and PDL-F appeared at the same time in 67 patients while 25 cases were not aware of the presence of PDL-F. The triggering factor was pregnancy in 12 patients; acute illness such as viral hepatitis in 3, typhoid in 2 and chicken pox in one patient. Thirty-six patients had history of POM in one or more of their family members. Periorbital melanosis was associated in 92% of cases with PDL-F. The pattern and extension of POM and PDL-F was similar among the affected family members [Figure - 3].
When inspected from the front, after closing the eye, the pigmentation of the POM was seen to be around the eyes in all the patients. The intensity of the pigment was same all throughout the radius of the circle around the eyelids. When viewed from the side, the PDL-F was first noticed, in which a patch of hyperpigmentation with sharp demarcation line was present at the side of the face. However, the sharpness of the PDL-F extended up to a point about half an inch to two inches below the lateral canthus [Figure - 2],[Figure - 3]. From this point onwards, the PDL-F was observed to be in continuation with periorbital melanosis. In other words, periorbital melanosis was observed as an extension of pigmentary demarcation line of the face. Thus, POM and PDL-F is one hyperpigmented patch, rather than two, which extends from around the eyes to the lateral side of the face in a definite pattern.
In 69 cases, Wood′s lamp examination showed diminished intensity of the hyperpigmentation of POM; the diminution of same intensity was also noticed in PDL-F on the ipsilateral side of the same patients. In twenty-three patients, both POM and PDL-F jointly became imperceptible after Wood′s lamp examination.
The histological examination of POM and PDL-F of the same patients showed variable degree of melanin pigment within upper dermal macrophages [Figure - 4].
Discussion
A common cosmetic concern, periorbital melanosis, is an ill-defined entity to date. Although it is well distributed among both the sexes, the preponderance of females is possibly due to the fact that they are more conscious about their appearance. As PDL-F is a physiological line, it remains unnoticed from childhood in most of the persons only to be revealed after any triggering factor(s) such as puberty, pregnancy and some unknown causes. In our series, the triggering factors were some acute illnesses such as viral hepatitis, typhoid and chicken pox apart from the abovementioned factors. Both POM and PDL-F appeared at the same time in 67% of patients; the remaining 25% of the patients were not aware of the presence of PDL-F, and it was noticed only after close inspection.
Pigmentary demarcation line-F (PDL-F) were absent in 8% cases, whose age varied between 11 and 22 years. These patients should be followed up for the appearance of PDL-F as the triggering factors may not have stimulated the physiological line to appear as yet. On close inspection, POM was observed as a circular hyperpigmented patch around the eyes. Its medial boundary was clear and extends up to the lateral aspect of bridge of nose on the same side
[Figure - 1],[Figure - 2],[Figure - 3]. The lateral boundary of POM was seen merging with this PDL-F [Figure - 2],[Figure - 3]. The sharp border of PDL-F halts at a point approximately 0.5-2 inches away from the lateral canthus of eye inferiolaterally, where it is in continuation with the POM. Thus, the hyperpigmented patches of both POM and PDL-F stands out as a single patch [Figure - 1],[Figure - 2],[Figure - 3], rather than two different patches of two different conditions.
Histological examination of our four cases showed melanophages in upper dermis in both POM and PDL-F. This fact could be correlated with the relative inffectiveness of the various therapies in POM.
Therefore, we conclude that POM and PDL-F are not two entities, but one. Thereby, we define periorbital melanosis as an extension of pigmentary demarcation line-F of the face and propose the dermal nature of its pigment.
| 1. |
West TB, Alister TS. Improvement of infraorbital hyperpigmentation following carbon dioxide laser resurfacing. Dermatol Surg 1998;24:615-6.
[Google Scholar]
|
| 2. |
Lowe NJ, Wieder JM, Shorr NS, Boxrud C, Saucer D, Chalet M. Infraorbital pigmented skin. Dermatol Surg 1995;21:767-70.
[Google Scholar]
|
| 3. |
Goodman RM, Belcher RW. Periorbital hyperpigmentation. Arch Dermatol 1969;100:169-74.
[Google Scholar]
|
| 4. |
Miura O. On the demarcation lines of pigmentation observed among the Japanese, on inner sites of their extremities and on anterior and posterior sites of their medial regions. Tohoku J Exp Med 1951;54:135-40.
[Google Scholar]
|
| 5. |
Malakar S, Dhar S. Pigmentary demarcation lines over the face. Dermatology 2000;200:85-6.
[Google Scholar]
|
| 6. |
Somani VK, Razvi F, Sita VN. Pigmentary demarcation lines over the face. Indian J Dermatol Venereol Leprol 2004;70:336-41.
[Google Scholar]
|
Fulltext Views
24,027
PDF downloads
4,981





