Translate this page into:
Photosensitive spongiotic/lichenoid eruption of micropapules and plaques: A morphologically distinct entity
2 Department of Pathology, All India Institute of Medical Sciences, New Delhi, India
Correspondence Address:
Binod K Khaitan
Department of Dermatology and Venereology, All India Institute of Medical Sciences, Ansari Nagar, New Delhi - 110 029
India
| How to cite this article: Shah N, Khaitan BK, Ramam M, Sharma VK, Singh MK. Photosensitive spongiotic/lichenoid eruption of micropapules and plaques: A morphologically distinct entity. Indian J Dermatol Venereol Leprol 2013;79:497-505 |
Abstract
Background: A distinct morphological pattern of photodermatosis has been observed with shiny skin colored to hypopigmented tiny papules, discrete or coalescing to form plaques. Aims: To study the clinico-pathological features of patients presenting with these lesions. Methods: A total of 72 patients were recruited. Clinical examination and skin biopsy was carried out to evaluate the morphological patterns and the histopathological features. Results: In all patients, tiny discrete to coalescent papules were observed on sun-exposed sites but usually sparing the face. The condition occurred more commonly in women. Three specific histopathological patterns were observed : 0 spongiotic (43.7%), lichenoid (22.5%), psoriasiform (18.7%) and also perivascular pattern in 5%. Conclusion: Photosensitive lichenoid eruption is a morphologically distinct photodermatoses that is commonly seen in Indian patients with pathological features showing mostly spongiotic changes and in some cases lichenoid changes.Introduction
A photodermatosis with distinct morphological appearance characterized by shiny, skin colored to hypopigmented tiny papules, discrete or coalescing to form plaques has been reported. This entity has been described variously as summer time actinic lichenoid eruption (SALE), [1],[2] actinic lichen nitidus, [3] and lichen nitidus actinicus. [4],[5] A pinpoint papular variant of polymorphous light eruption in African Americans, in Singaporean patients of Asian origin and a micropapular light eruption in Japanese patients have also been described and appear to represent the same entity. [6],[7],[8],[9],[10] These reports have included small numbers of patients and biopsies, ranging from 1 to 25. We describe the clinicopathological features of the condition in 72 Indian patients seen in our hospital.
Methods
The study was conducted in the Department of Dermatology and Venereology at AIIMS, New Delhi from December 2005 to October 2007 after ethical clearance from the Institutional Ethics Committee.
Patients who had hypopigmented, skin colored or hyperpigmented micropapules or papules, violaceous papules or plaques, or lichenified plaques on photo-exposed skin were included. Patients with wet eczematous changes, classical lesions of lichen planus, or lichen nitidus were excluded. On the first visit, a detailed history was obtained and a complete physical examination performed. Initial lesions and their evolution were noted. Seasonal variation and relation to sunlight was assessed. Any history suggestive of atopy was recorded. History of drugs taken and skin care products used over the affected area in the 2 weeks before the onset of disease was obtained. Clinical photographs were taken at the outset, at 2 weeks and 4 weeks after initiation of treatment and
the response to treatment was observed. Skin biopsy from the representative lesions was taken in 70 patients. Two patients′ biopsy could not be taken.
As a preliminary step, it was decided to do phototesting and photopatch test in only 10 patients. However, though phototesting (photoprovocation) could be done in 10 patients, photopatch testing could be done in only three patients with ultraviolet A (UVA) chamber (UV 7001 K Waldmann, Germany). Minimal erythema dose (MED) for UVA cannot be calculated for Indian skin, [11] so we arbitrarily chose an initial dose of 6 J/cm 2 for photo-provocation. A total of five doses of UVA was given once daily from Monday to Friday starting from 6 J/cm 2 with increments of
1 J/cm 2 per day. On day 5, the final reading was done. Patch testing and photopatch testing was done with
20 antigens in the Indian standard series (ISS) recommended by the contact and occupational contact dermatoses forum of India (CODFI) in only three patients.
All patients were treated with fluocinolone acetonide 0.025% cream applied twice daily on the lesions and the response was recorded at 2 weeks and 4 weeks. Patients were advised to avoid sunlight and use a sunscreen.
Results
Clinical features
There were 48 females, and 24 males with mean age of 29.2 ± 10.4 years (range 12-65 years). The mean age at onset was 27.1 ± 10.4 years (range 9-64 years). Duration of disease ranged from 15 days to 17 years (mean: 2.2 years). A total of 53 (73.6%) patients gave history of sun-exposure of approximately 1-4 h in the course of the day during their routine activity and occupational activities, 14 (19.4%) patients had minimal or less than an hour of sun-exposure and 5 (6.9%) had history of sun-exposure of more than 4 h.
A total of nine patients gave history of taking medications before the onset of lesions: antitubercular therapy INH, rifampicin, pyrazinamide, ethambutol (HRZE) and oral contraceptives in two patients each; and vitamin supplements, amlodipine, citalopram and zolpidem, unknown ayurvedic medication and fluconazole, and glibenclamide, in one patient each. Seven of them had been taking drugs for 2 months or longer before the onset of lesions. One of the patients had undergone shortwave diathermy for pain in the neck and after 2-3 sittings (approximately over a week) developed exacerbation of the pre-existing lesions. A total of 53 (73.6%) patients gave history of application of a variety of oils, moisturizers or petroleum jelly. No patient had applied these substances exclusively to the areas of the lesion.
A total of 48 (66.7%) patients presented with their first episode while 24 (33.3%) had recurrent episodes (2-12).
Itching was mild in 31 (43.1%) patients, moderate in 30 (41.7%), severe in 10 (13.9%) and absent in a patient. The most common site of onset was forearms (34 [47.2%]), followed by nape and sides of the neck and upper back (23). There were relatively fewer patients who presented with onset on the face (8), dorsa of hands (3), or arms (3). One patient had onset of lesions both on arms and forearms simultaneously.
A total of 37 patients (51.4%) had onset in summer and early rainy season (May-July) and 21 (29.2%) patients in the spring (February-April). Patients also reported exacerbations in summer and spring. A total of seven patients (9.7%), each one of whom had onset in late rainy season and autumn (August-October) and winter (November-January) months.
A history suggestive of atopy was noted in 12 (16.7%) patients, and a family history of atopy in 8 (11.1%) patients.
General physical examination was normal in almost all the patients. Five patients, however, showed pallor, and one showed pedal edema and mild acanthosis nigricans.
The eruption consisted of papules and plaques [Figure - 1],[Figure - 2],[Figure - 3] and [Figure - 4]; the former were predominant in 25 patients (34.7%), the latter in 25 patients (34.7%); 7 (9.7%) patients had only papules while 1 (1.4%) patient had plaques alone. The number of papules ranged from a few to numerous, while the number of plaques ranged from 1 to 25.
 |
| Figure 1: Hypopigmented, skin colored, grouped papules |
 |
| Figure 2: Tiny, hypopigmented, discrete papules |
 |
| Figure 3: Papules coalescing to form a plaque |
 |
| Figure 4: Plaque on abdomen in a sari wearing woman |
Papules were round, flat topped, and were tiny ranging in size from 1-2 mm (47 [66.2%]) to 2-4 mm in 24 (33.8%) patients. The papules tended to group and also coalesce together to form plaques. The papules were hypopigmented (59 [83.1%]), skin colored (22 [31%]), hyperpigmented (12 [16.9%]), erythematous (12 [16.9%]), and violaceous (1 [1.4%]), with papules of more than one color in some patients. Mild, white, fine and loosely adherent scaling was present in 29 (40.8%) patients. The eruption was present on photo-exposed skin, 3 (4.2%) patients also had lesions on covered sites. Involvement was bilateral in 66 (93%) patients. In four patients the involvement was bilateral on forearms but on the neck, anterior right side was involved sparing the left side due to the way a sari is worn by Indian women. In one sari wearing woman, there was involvement of the left side of the abdomen, which is exposed while wearing a sari [Figure - 4].
The plaques were mostly formed by coalescence of papules. Indeed, in 60 of these patients there were some discrete papules at the periphery of the plaques. The color of the plaques ranged from hypopigmented, skin colored, erythematous to hyperpigmented and violaceous. Size of the plaques was 1-3 cm in 47 patients (72.3%). The plaques were larger in 18 patients (27.7%) with a maximum size of 8 cm. Plaques were round to oval in 53 patients (81.5%) and irregularly shaped in 28 patients (43.1%). Margins of the plaques were ill-defined in most of the cases, with a well-defined margin seen only in a few cases. Scaling overlying the plaques was seen in 37 (56.9%) patients. Excoriation and lichenification were observed in 9 (13.9%) and 4 (6.2%) patients respectively.
Histopathology
Histopathological analysis was carried out in 80 skin biopsies from 70 patients. In two patients, biopsy could not be taken. Four major reaction patterns were observed: spongiotic in 35, lichenoid in 18, psoriasiform in 15, perivascular lymphohistiocytic infiltrate in four while eight biopsies showed other patterns.
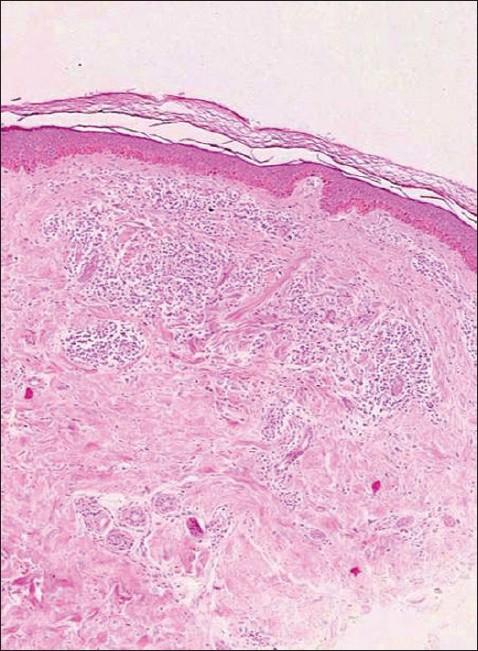
On analyzing these 80 specimens, 35 specimens (43.7%) showed the spongiotic pattern [Figure - 5] and [Figure - 6].
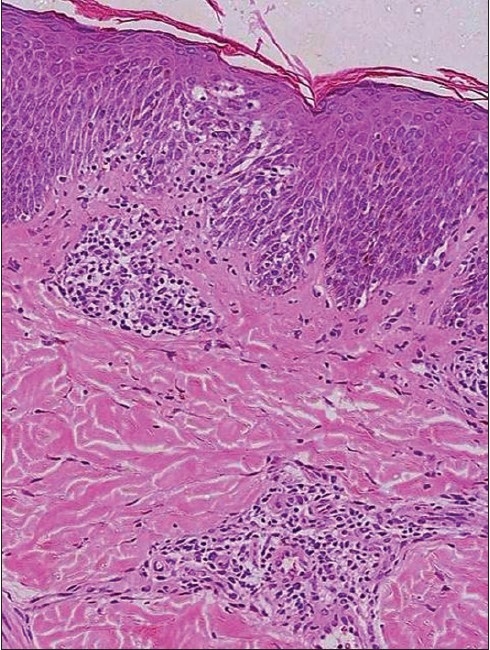 |
| Figure 5: Spongiotic pattern: Epidermal spongiosis, papillary edema and a superficial perivascular infiltrate (H and E, × 100) |
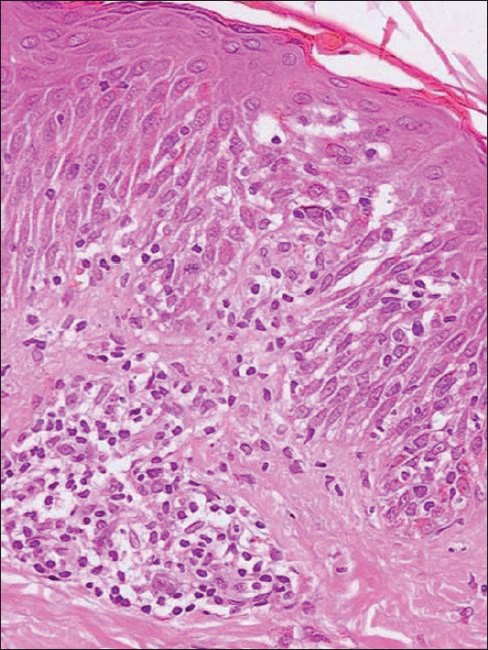 |
| Figure 6: Spongiotic pattern: Epidermal spongiosis with exocytosis of lymphocytes (H and E, × 200) |
The changes in the epidermis and underlying dermis were focal. Biopsies revealed parakeratosis, acanthosis, spongiosis, exocytosis of lymphocytes and histiocytes and edema of individual dermal papillae with an infiltrate of lymphocytes and histiocytes. The infiltrate also extended around vessels in the superficial dermal plexus. The severity of the changes varied in the biopsies. Parakeratosis varied from spotty to mounds and zones of parakeratosis that contained globules of fibrin. Spongiosis was mild and focal in some while it was marked and associated with the formation of a spongiotic vesicle in others. Spongiosis also affected the upper follicular epithelium in two cases. Three cases showed flask-shaped collections of Langerhans cells in the epidermis. Acanthosis was of mild to moderate degree in most of the specimens but was absent in four cases. In the dermis, there was papillary edema with a lymphohistiocytic infiltrate. Papillae appear to be expanded more by edema than the infiltrate. One biopsy showed focal extravasation of red blood corpuscles (RBCs) in the papilla (unaccompanied by other changes of vasculitis). In addition, there was a superficial perivascular infiltrate of lymphocytes and histiocytes that was accompanied, in three cases, by eosinophils. The infiltrate extended around hair follicles and into the mid- and deep-dermis in three cases.
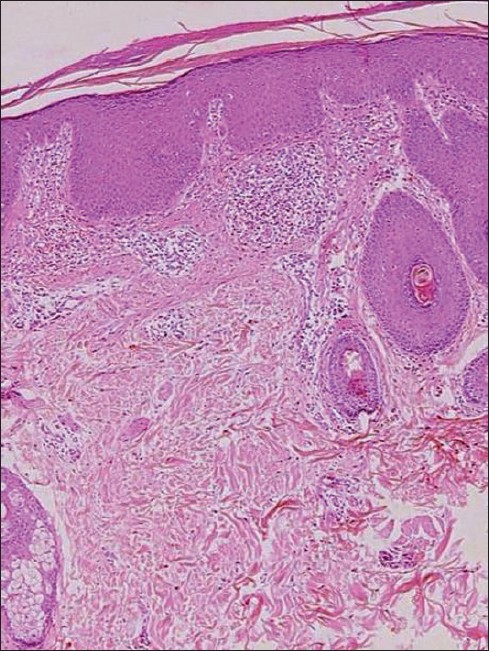
Eighteen specimens (22.5%) showed the lichenoid pattern [Figure - 7] and [Figure - 8]. Characteristically, an infiltrate of lymphocytes and histiocytes filled and expanded a single dermal papilla that was mildly edematous. Melanophages were prominent in the superficial dermis. The epidermis was thinned overlying the infiltrate and basal cells showed vacuolization and/or necrosis of keratinocytes. Colloid bodies were seen in the papillary dermis. Two biopsies showed mild parakeratosis overlying the papillary dermal infiltrate and three showed mild spongiosis but exocytosis was not prominent. In a patient who had biopsies taken from both a papule and a plaque, the latter showed a lichenoid infiltrate in adjacent papillae coalescing in almost a band like pattern, while the papule showed similar changes confined to one papilla.
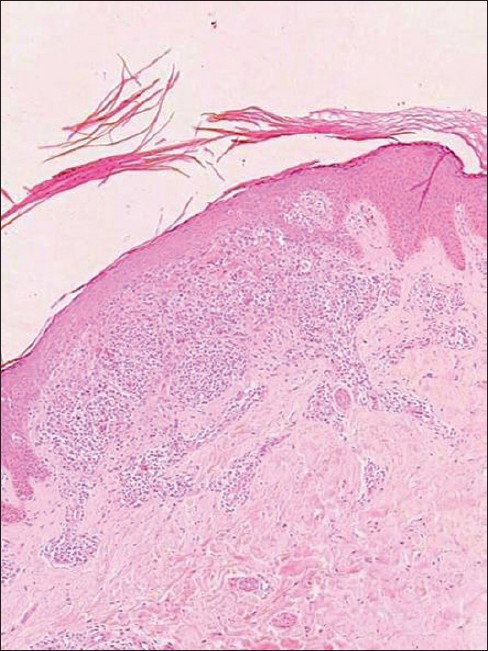 |
| Figure 7: Lichenoid pattern: Lichen nitidus-like morphology (H and E, × 40) |
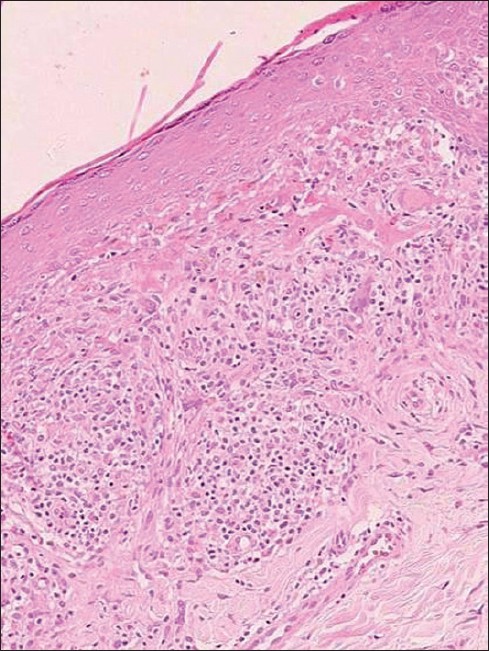 |
| Figure 8: Lichenoid pattern: Basal cell damage with a compact papillary dermal infiltrate (H and E, × 100) |
A psoriasiform pattern was seen in 15 (18.7%) specimens [Figure - 9]. There was compact hyperkeratosis with bulbous rete pegs and varying amounts of papillary fibrosis. There was mild spongiosis in six cases. There was a lymphohistiocytic infiltrate in the papillary dermis associated with papillary edema and perivascular lymphohistiocytic infiltrate.
 |
| Figure 9: Psoriasiform pattern: Epidermal hyperplasia with a superficial perivascular infiltrate. (H and E, × 40) |
Four biopsies were identified with a perivascular lymphohistiocytic pattern [Figure - 10]. There was perivascular infiltrate composed of lymphocytes and histiocytes in the superficial dermis. The infiltrate was associated with edema in one of the cases and extended into the deep dermis and around the follicles. The infiltrate was composed of mainly lymphocytes and histiocytes, with giant cells seen in one and melanophages in another specimen. There were no epidermal changes except in one which showed focal epidermal atrophy.
 |
| Figure 10: Perivascular pattern: A superficial infiltrate with no epidermal changes. (H and E, × 40) |
Five biopsies were essentially normal and did not show any abnormalities. One showed changes suggestive of prurigo, and one showed only mild acanthosis. One biopsy was not available for evaluation.
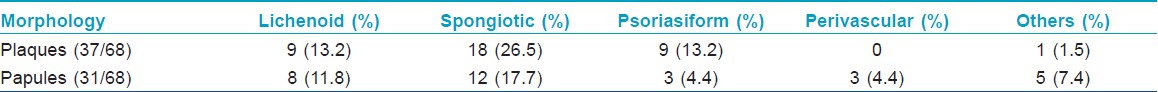
Clinicopathological correlation
Out of 80 biopsy specimens, in 68 (taken from 59 cases), clinicopathological correlation could be done. It was noted whether the biopsy was taken from a plaque or a papule. In the biopsies from the plaques, nine showed lichenoid pattern, eighteen showed spongiotic pattern, nine showed psoriasiform pattern and one biopsy showed essentially normal histology. In the biopsies from the papules, eight showed lichenoid pattern, twelve showed spongiotic pattern, three showed psoriasiform pattern and three showed the perivascular pattern. Four showed essentially normal histology, while one showed prurigo like changes [Table - 1].
Phototesting
Well-defined mild blanchable erythema and tanning was seen in 6 out of 10 patients. No lesions developed at the phototest sites. Two patients had mild itching on 2 nd and 4 th day respectively of phototesting. No changes were observed in the remaining two.
Patch testing and photopatch testing
One patient each showed positive reaction to solvent yellow and nickel sulfate, while the photopatch was negative. A third patient showed a positive photopatch test to benzocaine and potassium dichromate. There were no findings suggestive of contact dermatitis due to these agents in any of the three patients; their lesions were similar to those of other patients. Photopatch testing could not be done in 7 out of 10 patients as ISS series was not available for some time.
Treatment and follow-up
Forty one patients were followed-up at 2 weeks and 35 patients were followed-up at 4 weeks after treatment. At
2 weeks, 14.6% showed complete or almost complete clearance, while at 4 weeks, 74.2% showed complete or almost complete clearance.
Discussion
A photosensitive eruption composed of tiny papules has been described from the Indian subcontinent, Japan, Singapore and in African American patients [Table - 2]. [1],[3],[4],[5],[6],[7],[8],[9] There is general agreement across studies on the distinctive clinical features of the disease: light to skin colored tiny papules, discrete and coalescing, on photo-exposed skin of the neck and upper limbs, usually sparing the face and occurring more commonly in women except in the Singaporean study where the eruption was common on the face and neck, and more common in men. [8] In contrast, the classic form of polymorphous light eruption, commonly affects the face and dorsa of the hands along with the other sun-exposed areas. [12],[13] Furthermore, the clinical morphology is so distinct in our patients that we may lose its value if an umbrella term of polymorphous light eruption (PMLE) is used for this subsets of patients. In our department, informally the term photosensitive lichenoid eruption was loosely used for several years, but we were not getting lichenoid histopathology in a good proportion of these patients, which led us to study this entity. The eruption is mildly to moderately itchy and responds to treatment with topical corticosteroids and photoprotection. [1],[7]
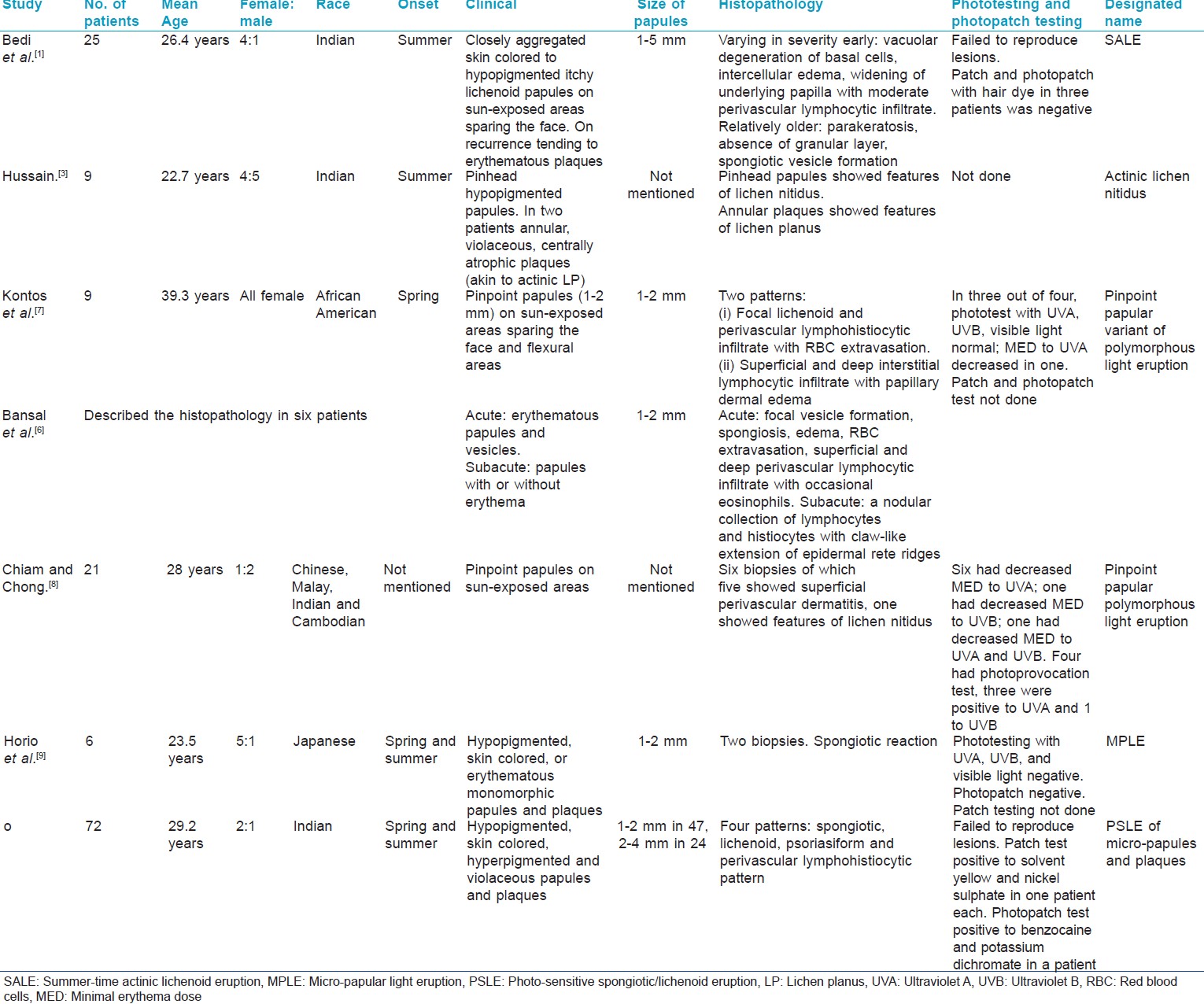
There has been less agreement about the histopathological findings. Some workers found changes resembling lichen nitidus and this has led to their designating the condition actinic lichen nitidus or lichen nitidus actinicus. [3],[4],[5] In other studies, biopsies were reported to show spongiotic and lichenoid change. [1],[3],[4],[5],[6],[7],[8],[9],[10] We found predominantly three patterns: spongiotic (43.7%), lichenoid (22.5%), psoriasiform (18.7%) and we also noted perivascular pattern in 4 (5%) specimens. The common denominator appeared to be the filling and expansion of the papillae in the dermis with inflammatory infiltrate and edema. Typically, a few individual papillae in each section were affected with adjacent papillae spared. However, in some biopsies, 2-3 adjacent papillae were involved and less frequently, multiple adjacent papillae were affected. This similarity in the pattern of papillary dermal involvement gave some cases with a spongiotic pattern a superficial resemblance to lichen nitidus at scanning magnification; but scrutiny revealed features of spongiotic dermatitis. In the biopsies showing a lichenoid pattern, the papillary contents consisted predominantly of lymphocytes and histiocytes while edema was the more prominent element in the spongiotic pattern. Epidermal changes were largely confined to the epidermis overlying affected papillae in the spongiotic pattern. In the psoriasiform pattern, compact hyperkeratosis and variable acanthosis was seen along with the papillary dermal infiltrate. However, the expansion of the papillae was not present; instead papillary fibrosis was more prominent.
One could speculate that sunlight induces changes in the papillary dermis that are accompanied by a lichenoid or spongiotic change in some individuals. This is modified by scratching to produce a psoriasiform pattern in others. Perivascular infiltrates without epidermal changes may represent an infrequent response in patients who show dermal changes alone. We also experienced that examination of multiple sections is recommended before categorizing the pattern, particularly in biopsies that appear to show few changes. The similarity of the clinical picture in spite of the different histopathological patterns can be explained thus: the small, discrete papules clinically characteristic of the disease are probably a manifestation of pathology in individual dermal papillae seen on biopsy. The same clinical appearance is manifested independent of the nature of changes in the papilla.
Though, the drug history was positive in 9 (12%) patients, the vast variety of drugs and no definite temporal correlation suggest that perhaps drugs do not play a role in the eruption. Since the photo-patch test was done only in three patients, we cannot interpret its results. Photo-provocation did not show the appearance of lesions in any patient, though transient erythema and tanning was seen in some. It seems that real-life situation in these patients may not be simulated by limited exposure to UVA in currently available UVA chambers.
The condition has received different names. The designations SALE, actinic lichen nitidus and lichen nitidus actinicus suggest that the condition is characterized by a lichenoid tissue reaction on biopsy, which is true of a subset of patients, not of all. Pinpoint papular variant of polymorphous light eruption and micropapular light eruption are more inclusive designations because they stress the clinical feature common to all patients, irrespective of histopathological appearance. We coined the term "Photosensitive spongiotic/lichenoid eruption (PSLE) of micropapules and plaques" for it is self-explanatory and also has similarity to the acronym PMLE. In this nomenclature, we are not including psoariasiform consciously, because we think such change is secondary and may be seen with itchy chronic, coalescent lesions and the primary process is either spongiform or lichenoid.
Similar larger studies from other centers in India and other countries may clarify the doubt whether "PSLE of micropapules and plaques" is an exclusive and distinct entity seen in Indian population alone or it is relevant for other parts of the world also.
Acknowledgments
Jenny Murase MD kindly translated the Japanese references.
| 1. |
Bedi TR. Summertime actinic lichenoid eruption. Dermatologica 1978;157:115-25.
[Google Scholar]
|
| 2. |
Isaacson D, Turner ML, Elgart ML. Summertime actinic lichenoid eruption (lichen planus actinicus). J Am Acad Dermatol 1981;4:404-11.
[Google Scholar]
|
| 3. |
Hussain K. Summertime actinic lichenoid eruption, a distinct entity, should be termed actinic lichen nitidus. Arch Dermatol 1998;134:1302-3.
[Google Scholar]
|
| 4. |
Kanwar AJ, Kaur S. Lichen nitidus actinicus. Pediatr Dermatol 1991;8:94-5.
[Google Scholar]
|
| 5. |
Kanwar AJ, Kaur S. Lichen nitidus actinicus. Arch Dermatol 1999;135:714.
[Google Scholar]
|
| 6. |
Bansal I, Kerr H, Janiga JJ, Qureshi HS, Chaffins M, Lim HW, et al. Pinpoint papular variant of polymorphous light eruption: Clinical and pathological correlation. J Eur Acad Dermatol Venereol 2006;20:406-10.
[Google Scholar]
|
| 7. |
Kontos AP, Cusack CA, Chaffins M, Lim HW. Polymorphous light eruption in African Americans: Pinpoint papular variant. Photodermatol Photoimmunol Photomed 2002;18:303-6.
[Google Scholar]
|
| 8. |
Chiam LY, Chong WS. Pinpoint papular polymorphous light eruption in Asian skin: A variant in darker-skinned individuals. Photodermatol Photoimmunol Photomed 2009;25:71-4.
[Google Scholar]
|
| 9. |
Horio T, Danno K, Furukawa F, Okamoto H. Micropapular light eruption. Nihon Hifuka Gakkai Zasshi 1986;96:519-22.
[Google Scholar]
|
| 10. |
Ideyama S, Moriwaki S, Horio T. Experimental production of micropapular light eruption. Nihon Hifuka Gakkai Zasshi 1988;98:341-4.
[Google Scholar]
|
| 11. |
Mehta RV, Shenoi SD, Balachandran C, Pai S. Minimal erythema response (MED) to solar simulated irradiation in normal Indian skin. Indian J Dermatol Venereol Leprol 2004;70:277-9.
[Google Scholar]
|
| 12. |
Ledo E. Photodermatosis. Part I: Photobiology, photoimmunology, and idiopathic photodermatoses. Int J Dermatol 1993;32:387-96.
[Google Scholar]
|
| 13. |
Honigsmann H, Tomoka MT. Polymorphous light eruption, hydroa vacciniforme, and actinic prurigo. In: Lim HW, Honigsmann H, Hawk JL, editors. Photodermatology. 1 st ed. New York: Informa Healthcare; 2007. p. 149-83.
[Google Scholar]
|
Fulltext Views
11,515
PDF downloads
2,471





