Translate this page into:
Phototherapy for mycosis fungoides
Correspondence Address:
Sunil Dogra
Department of Dermatology, Venereology and Leprology, Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh - 160 012
India
| How to cite this article: Dogra S, Mahajan R. Phototherapy for mycosis fungoides. Indian J Dermatol Venereol Leprol 2015;81:124-135 |
Abstract
Background: Both phototherapy and photochemotherapy have been used in all stages of mycosis fungoides since they improve the symptoms and have a favourable adverse effect profile. Materials and Methods: We performed an extensive search of published literature using keywords like "phototherapy", "photochemotherapy", "NBUVB", "PUVA", "UVA1", "mycosis fungoides", and "Sezary syndrome", and included systematic reviews, meta-analysis, national guidelines, randomized controlled trials (RCTs), prospective open label studies, and retrospective case series. These were then arranged according to their levels of evidence. Results: Five hundred and forty three studies were evaluated, of which 107 fulfilled the criteria for inclusion in the guidelines. Conclusions and Recommendations: Photochemotherapy in the form of psoralens with ultraviolet A (PUVA) is a safe, effective, and well tolerated first line therapy for the management of early stage mycosis fungoides (MF), that is, stage IA, IB, and IIA (Level of evidence 1+, Grade of recommendation B). The evidence for phototherapy in the form of narrow-band UVB (NB-UVB) is less robust (Level of evidence 2++, Grade of recommendation B) but may be considered at least as effective as PUVA in the treatment of early-stage MF as an initial therapy. In patients with patches and thin plaques, NB-UVB should be preferentially used. PUVA may be reserved for patients with thick plaques and those who relapse after initial NB-UVB therapy. For inducing remission, three treatment sessions per week of PUVA phototherapy or three sessions per week of NB-UVB phototherapy may be advised till the patient achieves complete remission. In cases of relapse, patients may be started again on PUVA monotherapy or PUVA may be combined with adjuvants like methotrexate and interferon (Level of evidence 2+, Grade of recommendation B). Patients with early-stage MF show good response to combination treatments like PUVA with methotrexate, bexarotene or interferon-α-2b. However, whether these combinations hold a significant advantage over monotherapy is inconclusive. For late stage MF, the above-mentioned combination therapy may be used as first-line treatment (Level of evidence 3, Grade of recommendation C). Currently, there is no consensus regarding maintenance therapy with phototherapy once remission is achieved. Maintenance therapy should not be employed for PUVA routinely and may be reserved for patients who experience an early relapse after an initial course of phototherapy (Level of evidence 2+, Grade of recommendation B). Bath-water PUVA may be tried as an alternative to oral PUVA in case the latter cannot be administered as the former may show similar efficacy (Level of evidence 2-, Grade of recommendation C). In pediatric MF and in hypopigmented MF, both NB-UVB and PUVA may be tried (Level of evidence 3, Grade of recommendation D).INTRODUCTION
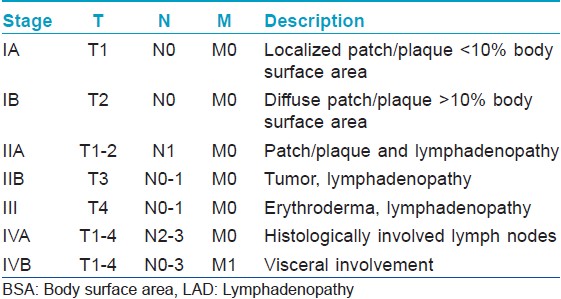
Cutaneous T-cell lymphomas (CTCLs) are a heterogenous group of non-Hodgkin lymphomas (NHL) of which mycosis fungoides (MF) is the most common form comprising about 65%. Mycosis fungoides has an indolent clinical course with a low risk of mortality in early disease [Table - 1]. The histology is characterized by epidermotropism of small- to medium-sized atypical T lymphocytes with cerebriform nuclei, and presence of epidermal Pautrier′s micro abscesses. Immunohistochemistry reveals the cell of origin to be the mature memory Tcells (CD 3+ , CD 4+ , CD45RO + , CD 8− ). Tcell receptor gene analysis shows a clonal re-arrangement in the majority of cases. Therapeutically, the natural course of the disease is not modified by any type of treatment. Progression to extracutaneous involvement is estimated to occur in up to 30% of patients and is associated with a poor prognosis. [1] Based on the current literature, it is recommended that early-stage mycosis fungoides should be initially treated with skin directed therapy (SDT). [2],[3] These include topical therapies like corticosteroids, nitrogen mustard, and bexarotene; radiotherapy like total skin electron beam therapy, and superficial X-irradiation; and phototherapy.
The UV spectrum is arbitrarily divided into three sub-regions: UVA (320-400 nm), UVB (290-320 nm), and UVC (100-290 nm). The various forms in which phototherapy is administered include natural sunlight phototherapy (or heliotherapy), fluorescent tubes: UVA, PUVA (UVA + topical/systemic psoralens) and UVB. UVB phototherapy includes broadband (BB) UVB; of 290-320 nm and narrow band (NB) UVB of 311+/- 2 nm. The newer variants include targeted phototherapy like excimer laser and lamp (308+/- 2 mm). The various dermatologic indications of phototherapy are psoriasis, vilitigo, atopic dermatitis, patch/plaque stage mycosis fungoides, prevention of photodermatosis, pityriasis lichenoides chronica, scleroderma, uremic pruritus, acquired perforating dermatosis and mastocytosis. [4],[5],[6] Contraindications to the use of phototherapy include associated disorders with significant photosensitivity, lupus erythematosus and pregnant or lactating females (only for PUVA). The treatment may be used with caution in patients with history or family history of melanoma or non-melanoma skin cancer, exposure to ionizing radiation or arsenic, uremia and hepatic failure (for PUVA).
Irrespective of the disease indicated, there are two regimens that are most commonly used; the first involves determination of the individual′s minimum erythema dose (MED) or minimal phototoxic dose (MPD). Seventy percent of the MED value is used for the first treatment; thereafter therapy is given three times or more in a week with 20%, or 10% increments depending on local experience and skin type tolerance. Another approach, as commonly practiced in India, involves a standard starting dose (280 mJ/cm 2 for NB-UVB and 0.5 J/cm 2 for PUVA), with stepwise increase (usually 20%) depending upon the patient′s erythema response. [7] The safe administration of photo (chemo) therapy requires the involvement of a dermatologist knowledgeable about the modality, trained staff to administer treatment, and an informed patient.
Goals of the guidelines
The present guidelines are aimed to systematically review the evidence regarding the use of phototherapy and photochemotherapy in mycosis fungoides, their effectiveness and adverse effects and on this basis, put forth guidelines for the practicing dermatologists regarding their use.
Methodology
An extensive literature search was performed to collect data on the use of phototherapy in mycosis fungoides. Relevant literature published till July 2014 was obtained from PubMed, EMBASE and the Cochrane Library. Keywords like "phototherapy", "photochemotherapy", "NBUVB", "PUVA", "UVA1", "mycosis fungoides", and "Sezary syndrome" were used for literature search. All systematic reviews, meta-analysis, national guidelines, randomized controlled trials (RCTs), prospective open label studies, and retrospective case series in the English literature mentioning these keywords were reviewed. However, individual case reports mentioning the efficacious use of various forms of phototherapy were not included.
Evaluation of the literature
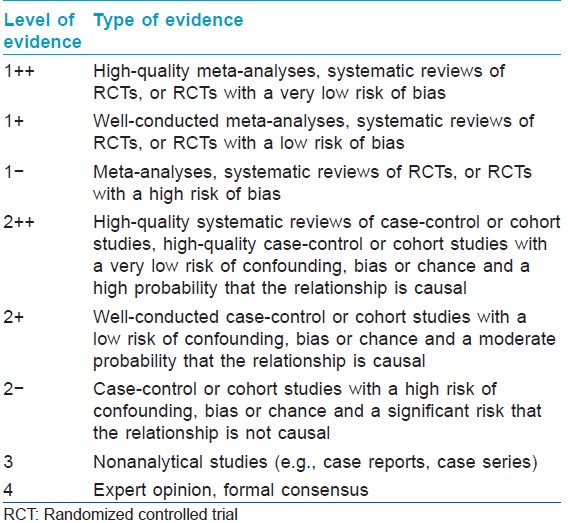
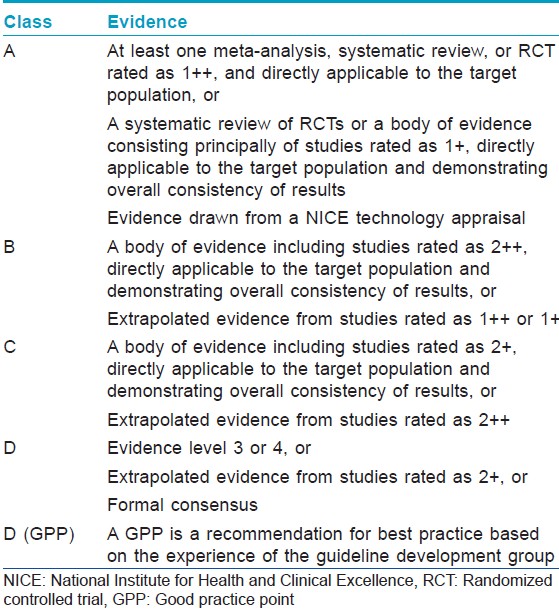
Evidence assessment: To assess the methodological quality of each study included for efficacy analysis, a grade of evidence was assigned using the criteria in [Table - 2] and [Table - 3].
Results
A total of 543 studies were evaluated, 107 of which fulfilled the criteria for inclusion in the guidelines. Other aspects of the interventions (e.g. safety and combination therapy) were evaluated in accordance with the publications available, but without conducting a complete, systematic review of the literature.
PUVA
Initial clearing regimen
There is a paucity of randomized controlled trials to prove the effectiveness of PUVA in mycosis fungoides. Hence, the recommendations are based on data derived from these few randomized controlled trials along with the prospective open labels studies and retrospective studies. PUVA has been tried in all stages of mycosis fungoides but is most successful in early-stage disease, i.e. less than stage IIa. Gilchrest et al. for the first time reported the successful treatment of nine patients with 8-methoxypsoralen plus UVA. [8] Briffa et al. in one of the largest prospective studies found PUVA to achieve remission in majority of the patients. [9] Subsequently, several studies have established the efficacy of PUVA although these are heterogeneous studies with differences in patient selection, treatment protocols, and outcome variables [Table - 4]. [10] Based on the data of five studies and a total of 244 patients, Herrmann et al. calculated the rate of complete remission after an initial course of PUVA to be 90% for stage IA, 76% for stage IB, 78% for stage IIA, 59% for stage IIB, and 61% for stage III disease (Level of evidence 2++) and similar figures have been reported by Hönigsmann et al. (with a mean duration of treatment being 2-5 months in stage IA-III MF). [11],[12] Whittaker et al. in a recent well conducted RCT observed that of the 41 patients receiving PUVA monotherapy, complete and partial remission (PR) was observed in 71% patients in a median of 27.5 PUVA sessions. [13] The median duration of response was 9·7 months and the total UVA doses received were 107 J/cm 2 (Level of evidence 1+). Wackermangel et al. evaluated the efficacy of PUVA using 5-methoxypsoralen (5-MOP) versus 8-MOP and found the two to have comparable results in terms of PUVA therapy duration, number of treatments or cumulative UVA dose and relapse rates. [14]
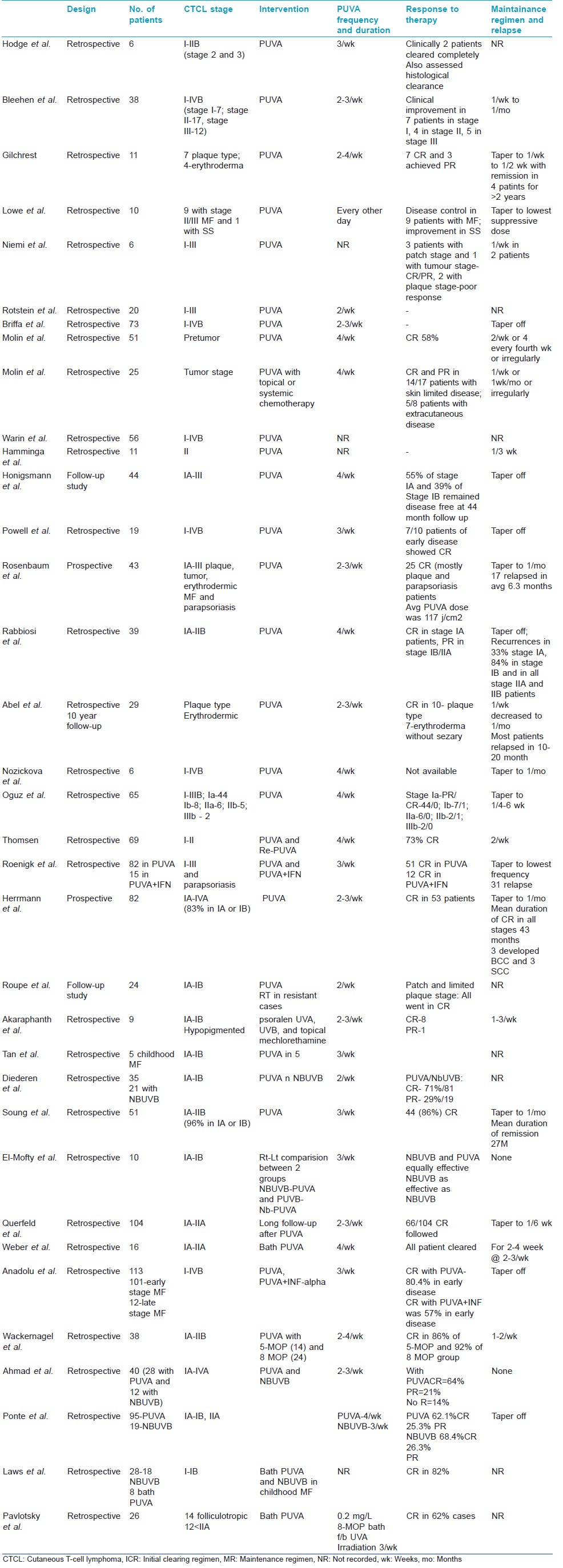
Frequency of PUVA
PUVA in mycosis fungoides is generally undertaken according to the guidelines established for the treatment of psoriasis. [15] The rates of complete remission vary from 58% to 88% when 2-3 treatments per week are administered; 42-86% when the frequency is 3 times per week; and 64-89% when PUVA is administered 2-4 times per week (Level of evidence 2+). [10] Once a patient achieves complete remission, a confirmatory biopsy of a previously exposed site is often recommended, although the implication of complete remission without pathological clearance is unclear.
Bath PUVA has been utilized as a therapeutic modality in patients in whom oral psoralens cannot be given. Pavlotsky et al. studied the effectiveness of bath PUVA (0.2 mg/L 8-methoxypsoralen bath 3 times weekly followed by UVA irradiation at 0.3 J/cm 2 with fixed increments every second session) in the treatment of folliculotropic mycosis fungoides (14 patients) and NBUVB-refractory early-stage mycosis fungoides (12 patients). [16] A complete clinical response was achieved in 62% of patients after an average of 33 weeks and a cumulative radiation dose of 158 J/cm 2 . In another study, bath-PUVA was shown to decrease CCR4(+) cells and Tregs in lesions of mycosis fungoides but did not induce circulating Tregs. [17] In a retrospective study by Weber et al., complete remission was achieved in all 16 patients after a mean duration of 63 days requiring 29 treatments and a mean cumulative UVA dose of 33 J/cm 2 . The time to relapse after complete clinical clearance was 45.6 (+/-9.2) weeks. The results were comparable to oral PUVA. [18] Bath PUVA has also been tried in childhood mycosis fungoides. In a retrospective review of 28 children, 79% of whom had hypopigmented mycosis fungoides, use of NB-UVB phototherapy and bath PUVA led to complete or partial remission in 19 out of 22 patients after a median of 4 months. In 7 out of 12 patients treated with NB-UVB, relapse occurred after a median of 4 months, whereas 4 out of 8 patients treated with bath PUVA relapsed after a median of 45.5 months. [19]
Relapse rates and disease-free interval
The relapse rates and disease-free interval after phototherapy are less well studied. Hönigsmann et al. followed up 44 patients treated with PUVA and found that 55.5% of patients with stage IA disease and 38.4% with stage IB disease remained in complete remission for more than 6 years, whereas all patients with T3 disease experienced relapses. [12] Roupe et al. reported follow-up of 24 patients with early-stage mycosis fungoides for 3-18 years treated with PUVA and noted long-term remission in nearly 50% of the patients. [20] Querfeld et al. followed up 66 patients who achieved complete remission with PUVA and reported 5- and 10-year disease-free survival rates for patients with T1 disease to be 56% and 30%, respectively, and for T2 disease to be 74% and 50%, respectively. [21] Survival rates at 5, 10, and 15 years did not differ between the non-relapse and relapse groups. The results with PUVA are comparable to those seen with topical chemotherapy and total skin electron beam radiation. [22],[23]
Combination treatment with PUVA
PUVA has been combined with other systemic treatments (interferon-α [IFN-α] and retinoids) [24],[25],[26] to improve efficacy or in patients with insufficient response to PUVA alone. In a recent systematic review, it was concluded that no combination treatment has been demonstrated to be superior to monotherapy. However, in advanced stages of mycosis fungoides, combining PUVA with IFN-α or retinoids did not improve response to treatment, a benefit that was seen with a combination of methotrexate with IFN-α. [27] In an open label trial by Stadler et al., PUVA was combined with IFN-α in patients with stages I and II disease and the combination was found to be effective in inducing complete remission in 10 of 13 patients and partial remission in another 3 patients (Level of evidence 2+). [28] Nikolaou found the combination of IFN-α2b and PUVA to be an effective and safe treatment treatment-refractory early stage MF patients as well as treatment-naïve advanced stage patients (Level of evidence 3). [29] In patients with advanced disease, complete remission rates were 14% versus 37% in stage IIB and III/SS patients, respectively. Patients with early stage disease had a 2-year disease-free survival of 100% versus 27% for the advanced stage group (P < 0.001).
In a phase III randomized controlled trial by EORTC Cutaneous Lymphoma Task Force, Whittaker et al. observed that there was no significant difference in response rate or response duration in early mycosis fungoides in the PUVA/bexarotene group versus PUVA group. [13] However, there was a trend toward fewer PUVA sessions and lower UVA dose required to achieve complete clinical response in the combination arm. Cheeley et al. in a small retrospective chart review studied 32 patients with cutaneous T cell lymphoma (CTCL) of whom 29 had mycosis fungoides, 2 had Sézary syndrome, and 1 had CTCL not otherwise specified. [30] In all, 26 patients received acitretin in addition to another therapy such as NB-UVB or PUVA. The overall response rate was 59%. In a prospective phase II trial by Chiarion-Sileni et al., of IFN-α-2a plus PUVA in patients with CTCL, 51 of 63 patients (Stage IA, n = 6; IB, n = 37; IIA, n = 3; IIB, n = 3; III, n = 12; IVA, n = 2) achieved complete remission (74.6%) or partial remission (6%) (Level of evidence 2+). [31] The median response duration was 32 months with a 5-year overall survival rate of 91% and the 5-year disease-free survival rate of 75%. In a multicentric prospective phase II clinical study by Rupoli et al. on 89 patients with early-stage IA to IIA mycosis fungoides treated for 14 months with low-dose IFN-α-2b (6-18 MU/week) and PUVA, [32] complete remission was achieved in 84% patients with an overall response rate of 98%; 6-month complete remission was associated with a non-confluent skin infiltrate on histology (P = 0.044) and 14-month complete remission with high epidermal CD1a + dendritic-cell density (P = 0.030). The combination protocol was successfully tolerated and the most common reason of failure was related to relapse and not to toxicity. Sustained remissions were achieved in 20% of patients. High CD8 + lymphoid T-cell density was associated with a lower relapse rate (P = 0.002).
NB-UVB
As with PUVA, uncontrolled trials and case series form the bulk of the evidence supporting its use in mycosis fungoides. NB-UVB is administered 2-3 times per week as the initial clearing regimen. [10] Most patients experience an erythema within 24 h, which decreases abruptly allowing follow up treatment at 48 h. [33] Milstein et al., in 1982 for the first time reported the successful use of UVB in 31 patients with mycosis fungoides. [34] In a retrospective analytical study involving 143 patients with early mycosis fungoides treated with PUVA, NB-UVB, psoralen and NB-UVB, BB-UVB or BB-UVA, there was no statistically significant difference between the response to oral PUVA and NB-UVB. [35] The efficacy of NB-UVB has been addressed by a number of studies and case series [Table - 5]. [10],[36],[37],[38],[39] Gokdemir et al. concluded that in stage IA-IIA, complete remission can be achieved with a NB-UVB thrice weekly regimen in 54-91% of patients within 3-4 months (Level of evidence 2+). [40] In this study, all the patients with patch stage mycosis fungoides had a complete remission, whereas in patients with plaque stage disease, 60% patients had a complete remission and 40% had partial remission or no clinical response. The mean cumulative dose and the mean number of treatments was 90.15 J/cm 2 and 35.33, respectively, in patch stage mycosis fungoides compared with 90.67 J/cm 2 and 39.40, respectively, in plaque stage mycosis fungoides (P > 0.05). In a study by Hofer et al., complete remission was achieved in five out of six patients after a mean of 20 treatments and 17.2 J/cm 2 cumulative doses, and. relapses were reported in all patients within a mean of 6 months after discontinuation of treatment. [41]
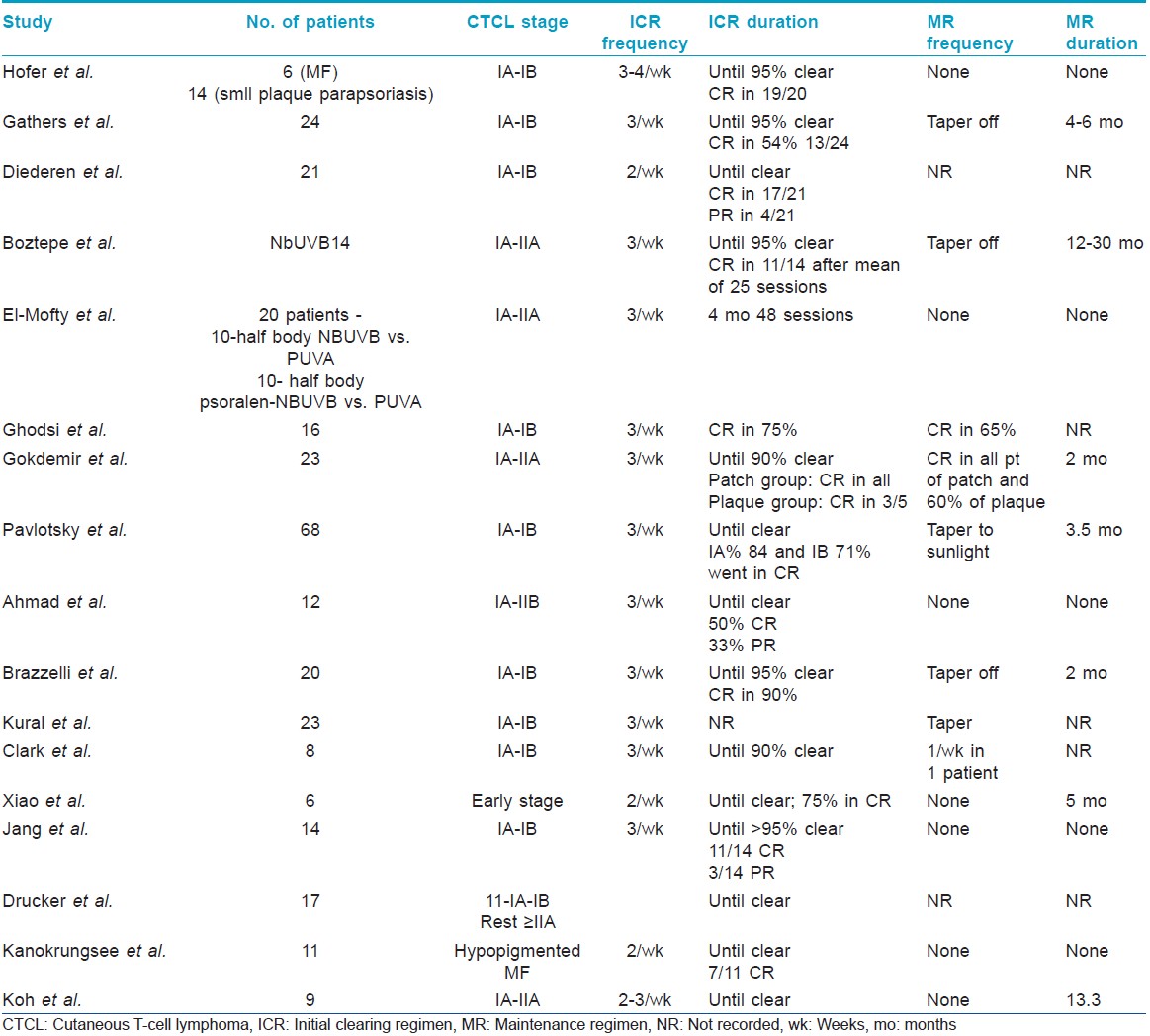
In a recent open label trial by Jang et al., 11 (78.6%) of 14 patients achieved complete remission within a mean of 15.36 ± 5.71 weeks, 31.0 ± 7.4 treatments and a mean cumulative UVB dose of 31.31 ± 12.16 J/cm 2 . [42] The remaining three patients achieved partial remission. Six of eleven patients relapsed after a mean of 8.5 ± 4.1 months. In one of the larger retrospective trials, Ponte et al. analyzed 95 patients treated with PUVA and 19 with narrow band UVB. [43] With PUVA, 59 patients (62.1%) had a complete remission, 24 (25.3%) had a partial remission, and 12 (12.6%) had a failed response. NB-UVB led to complete remission in 12 (68.4%) patients, partial remission in 5 (26.3%) patients, and a failed response in 1 (5.3%) patient. There were no differences in time to relapse between patients treated with PUVA and those treated with narrow-band UVB (11.5 vs. 14.0 months, respectively; P = 0.816). In another retrospective study of 56 patients comparing NB-UVB with PUVA, Diederen et al. found complete remission rates and mean relapse-free intervals to be similar between the two modalities and concluded that due to the practical advantages of NB-UVB, it might be a reasonable approach to a patient with early mycosis fungoides to start with NB-UVB and in case of lack of progression or lack of response switch to PUVA. [44] Similarly, Ahmad et al. in their retrospective analysis of 40 patients found both PUVA and NB-UVB to be effective in the treatment of early mycosis fungoides. [45] In another retrospective chart review, 15 of 17 patients with mycosis fungoides who were switched from PUVA to NB-UVB improved with better response in patients with earlier stage disease. [46]
In a small retrospective series of 11 patients with hypopigmented mycosis fungoides treated with NB-UVB twice weekly, 7 achieved complete remission with a mean of 40 treatments and the other 4 patients had a partial remission. Relapse was seen in three patients after a mean of 10 months. [47] In another series of nine patients with hypopigmented mycosis fungoides, six patients received NB-UVB and three patients received PUVA. [48] In six patients who had complete remission, disease recurred in four (66.7%), and the disease-free interval ranged from 2 months to 6 years. In another study involving patients with hypopigmented mycosis fungoides from Egypt, phototherapy was effective in 86.7% of patients with success rate of 66.7% with NBUVB and 80% with PUVA. [49] Similar observations were earlier made by Akaraphanth et al. [50] In childhood mycosis fungoides, a retrospective analysis of nine children of East Asian descent with early-stage disease showed that treatment with NB-UVB led to complete remission in eight children with no significant adverse effects but all showed disease relapse after a mean of 13.8 months (range 4-36). [51]
UVA1
In a preliminary short case series, four patients with early-stage mycosis fungoides were treated with 1630-2710 J/cm 2 UVA1 given in 29-40 fractions. Complete remission was achieved in all cases. [52] In a study by Zane et al., of the 13 patients (stage IB-III) who received high dose (100 J/cm 2 ) UVA1 phototherapy daily, 11 patients showed complete clinical and histological remission and another 2 had partial remission in contrast to the untreated control lesions. [53] In another study of 19 patients with mycosis fungoides treated with low-dose UVA-1 (20 or 30 J/cm 2 ), complete clinical and histological complete remission was achieved in 11 patients and partial remission in 3 patients after a mean cumulative dose of 1665 J/cm 2 and mean number of 73 exposure sessions. [54] In a study evaluating the efficacy of BB-UVA in the treatment of early-stage mycosis fungoides, 30 patients received either BB-UVA at 20 J/cm 2 /session or PUVA three times/week for 40 sessions. Comparable clinical and histopathological improvement was noted in both groups. [55] The authors concluded that the use of BB-UVA in the treatment of early-stage mycosis fungoides is comparable or even superior to PUVA regarding efficacy and remission periods. Similar observations have been made by other authors. [56],[57]
New developments in skin-targeted phototherapy include the excimer laser and the use of excimer light. There are seven studies, four of excimer laser and three of excimer light, all with good results. [58],[59],[60],[61],[62],[63],[64],[65]
Need for maintenance therapy in mycosis fungoides
In a recent multinational survey among dermatologists, 88% of the respondents indicated that they used some form of PUVA maintenance after clearance had been achieved. [10] There was, however, no agreement on duration, frequency, and UVA-dose and a wide range of schedules were in use. At present, there is insufficient evidence for the benefit of PUVA maintenance [Table - 6]. The recently published consensus of the EORTC suggested avoidance of maintenance therapy. [66] In their follow-up of nearly 28 months, Sanchez et al. observed that maintenance therapy with PUVA does not prevent relapse. A practical approach might be to reserve maintenance for patients who experience an early relapse after an initial course of PUVA and to adapt the schedule so as to minimize interference with the patients′ quality of life (e.g. once weekly without further dose increments for 3-6 months). [67] Pavlotsky et al. used BB-UVB and NB-UVB for treatment of cutaneous T cell lymphoma and demonstrated no difference in relapse rate for those with and without maintenance therapy. Sixty one percent of patients with disease relapse could be re-cleared with a second initial clearing regimen of UVB. [36] Boztepe et al. treated patients with NB-UVB using maintenance therapy and thought the use of maintenance phototherapy was a logical next step and may prolong the duration of remission. [37]

In another retrospective study involving 31 patients followed up for a median of 55 months (20-120 months), relapse was observed in 11 (35.5%) patients, within a mean of 28.8 ± 18.2 months (median 33 months, range 4-59 months), whereas 20 (64.5%) patients stayed relapse-free for a mean of 54.2 ± 28.8 months (median 55.5 months, range 20-119 months). Patients received maintenance phototherapy with a median duration of 12 months (range 1-30 months) after achieving complete response. [68]
Conclusions
In treating mycosis fungoides, it may be inferred that in patients with patches and thin plaques, NB-UVB should be preferentially used and that PUVA should be reserved for patients with thick plaques and those who relapse after initial response to UVB. In late stage disease, PUVA may be combined with methotrexate, bexarotene or interferon as first-line therapy. However, in early stage mycosis fungoides, the evidence is insufficient whether any combination is superior to monotherapy. Bath PUVA is another option especially when oral PUVA cannot be administered. However, more evidence needs to be generated on the efficacy of bath PUVA. Hence, it is reasonable to start with phototherapy alone and combine it with one of the alternative therapies in case of inadequate response or early relapse. Moreover, there are insufficient data to conclude which type of phototherapy and which schedule (e.g. in terms of dose increments, frequency, etc.) might be optimal. The same is true for maintenance treatments, for which efficacy has not yet been proven although they are widely used in clinical practice. Mycosis fungoides is rare in childhood. Hence, the usefulness of phototherapy is not clearly defined in children. Both NB-UVB and PUVA have shown efficacy in the treatment of childhood disease and variants such as hypopigmented mycosis fungoides. Since most of these studies are small case series, it is difficult to extrapolate the results to a larger population.
Acknowledgements
We acknowledge the contribution made by Dr. Venkatram Mysore, Consultant Dermatologist, Venkat Charamalaya in providing his expert views during the preparation of this manuscript. We also acknowledge the contribution made by Dr Ajay Rai, Junior Resident at the Department of Dermatology and Venereology, AIIMS, New Delhi in preparing [Table - 4] and [Table - 5].
| 1. |
Agar NS, Wedgeworth E, Crichton S, Mitchell TJ, Cox M, Ferreira S, et al. Survival outcomes and prognostic factors in mycosis fungoides/Sezary syndrome: Validation of the revised international society for cutaneous lymphomas/European organisation for research and treatment of cancer staging proposal. J Clin Oncol 2010;28:4730-9.
[Google Scholar]
|
| 2. |
Wollina U. Cutaneous T cell lymphoma: Update on treatment. Int J Dermatol 2012;51:1019-36.
[Google Scholar]
|
| 3. |
Trautinger F, Knobler R, Willemze R, Peris K, Stadler R, Laroche L, et al. EORTC consensus recommendations for the treatment of mycosis fungoides/Sezary syndrome. Eur J Cancer 2006;42:1014-30.
[Google Scholar]
|
| 4. |
Roelandts R. The history of phototherapy: Something new under the sun? J Am Acad Dermatol 2002;46:926-30.
[Google Scholar]
|
| 5. |
Van Weelden H, De La Faille HB, Young E, van der Leun JC. A new development in UVB phototherapy of psoriasis. Br J Dermatol 1988;119:11-9.
[Google Scholar]
|
| 6. |
Green C, Ferguson J, Lakshmipathi T, Johnson BE. 311 nm UVB phototherapy-an effective treatment for psoriasis. Br J Dermatol 1988;119:691-6.
[Google Scholar]
|
| 7. |
Dogra S, Kanwar AJ. Narrow band UVB phototherapy in dermatology. Indian J Dermatol Venereol Leprol 2004;70:205-9.
[Google Scholar]
|
| 8. |
Gilchrest BA, Parrish JA, Tanenbaum L, Haynes HA, Fitzpatrick TB. Oralmethoxsalenphotochemotherapy of mycosis fungoides. Cancer 1976;38:683-9.
[Google Scholar]
|
| 9. |
Briffa DV, Warin AP, Harrington CI, Bleehen SS. Photochemotherapy in mycosisfungoides. A study of 73 patients. Lancet 1980;2:49-53.
[Google Scholar]
|
| 10. |
Carter J, Zug KA. Phototherapy for cutaneous T-cell lymphoma: Online survey and literature review. J Am Acad Dermatol 2009;60:39-50.
[Google Scholar]
|
| 11. |
Herrmann JJ, Roenigk HH Jr, HönigsmannH. Ultraviolet radiation for treatment of cutaneous T-cell lymphoma. Hematol Oncol Clin North Am 1995;9:1077-88.
[Google Scholar]
|
| 12. |
Hönigsmann H, Brenner W, Rauschmeier W, Konrad K, Wolff K. Photochemotherapy for cutaneous T-cell lymphoma. J Am Acad Dermatol 1984;10:238-45.
[Google Scholar]
|
| 13. |
Whittaker S, Ortiz P, Dummer R, Ranki A, Hasan B, Meulemans B, et al. Efficacy and safety of bexarotene combined with psoralen-ultraviolet A (PUVA) compared with PUVA treatment alone in stage IB-IIA mycosisfungoides: Final results from the EORTC Cutaneous Lymphoma Task Force phase III randomized clinical trial (NCT00056056). Br J Dermatol 2012;167:678-87.
[Google Scholar]
|
| 14. |
Wackernagel A, Hofer A, Legat F, Kerl H, Wolf P. Efficacy of 8-methoxypsoralen vs. 5-methoxypsoralen plus ultraviolet A therapy in patients with mycosis fungoides. Br J Dermatol 2006;154:519-23.
[Google Scholar]
|
| 15. |
Holzle E, Honigsmann H, Rocken M, Ghoreschi K, Lehmann P. Recommendations for phototherapy and photochemotherapy. J Dtsch Dermatol Ges 2003;1:985-97.
[Google Scholar]
|
| 16. |
Pavlotsky F, Hodak E, Ben Amitay D, Barzilai A. Role of bath psoralen plus ultraviolet A in early-stage mycosis fungoides. See comment in PubMed Commons belowJ Am Acad Dermatol 2014;71:536-41.
[Google Scholar]
|
| 17. |
Kato H, Saito C, Ito E, Furuhashi T, Nishida E, Ishida T, et al. Bath-PUVA therapy decreases infiltrating CCR4-expressing tumor cells and regulatory T cells in patients with mycosis Fungoides.See comment in PubMed Commons below Clin Lymphoma Myeloma Leuk 2013;13:273-80.
[Google Scholar]
|
| 18. |
Weber F, Schmuth M, Sepp N, Fritsch P. Bath-water PUVA therapy with 8-methoxypsoralen in mycosis fungoides. Acta Derm Venereol 2005;85:329-32.
[Google Scholar]
|
| 19. |
Laws PM, Shear NH, Pope E. Childhood mycosis fungoides: Experience of 28 patients and response to phototherapy. Pediatr Dermatol 2014;31:459-64.
[Google Scholar]
|
| 20. |
Roupe G, Sandström MH, Kjellström C. PUVA in early mycosis fungoides may give long-term remission and delay extracutaneous spread. Acta Derm Venereol 1996;76:475-8.
[Google Scholar]
|
| 21. |
Querfeld C, Rosen ST, Kuzel TM, Kirby KA, Roenigk HH Jr, Prinz BM, et al. Long-term follow-up of patients with early-stage cutaneous T-cell lymphoma who achieved complete remission with psoralen plus UV-A monotherapy. Arch Dermatol 2005;141:305-11.
[Google Scholar]
|
| 22. |
Jones GW, Kacinski BM, Wilson LD, Willemze R, Spittle M, Hohenberg G, et al. Total skin electron radiation in the management of mycosis fungoides: Consensus of the EORTC-cutaneous lymphoma project group. J Am Acad Dermatol 2002;47:364-70.
[Google Scholar]
|
| 23. |
Kim YH, Martinez G, Varghese A, Hoppe RT. Topical nitrogen mustard in the management of mycosis fungoides. Arch Dermatol 2003;139:165-73.
[Google Scholar]
|
| 24. |
Tura S, Mazza P, Zinzani PL, Ghetti PL, Poletti G, Gherlinzoni F, et al. Alpha recombinant interferon in the treatment of mycosis fungoides (MF). Haematologica 1987;72:337-40.
[Google Scholar]
|
| 25. |
Olsen EA, Rosen ST, Vollmer RT, Variakojis D, Roenigk HH Jr, Diab N, et al. Interferon alfa-2a in the treatment of cutaneous T cell lymphoma. J Am Acad Dermatol 1989;20:395-407.
[Google Scholar]
|
| 26. |
Zhang C, DuvicM. Treatment of cutaneous T-cell lymphoma with retinoids. Dermatol Ther 2006;19:264-71.
[Google Scholar]
|
| 27. |
Humme D, Nast A, Erdmann R, Vandersee S, Beyer M. Systematic review of combination therapies for mycosis fungoides. Cancer Treat Rev 2014;40:927-33.
[Google Scholar]
|
| 28. |
Stadler R, Otte HG, Luger T. Prospective randomized multicenter clinical trial on the use of interferon α-2a plus acitretin versus interferon α-2a plus PUVA in patients with cutaneous T-cell lymphoma stages I and II. Blood 1998;92:3578-81.
[Google Scholar]
|
| 29. |
Nikolaou V, Siakantaris MP, Vassilakopoulos TP, Papadavid E, Stratigos A, Economidi A. PUVA plus interferon α2b in the treatment of advanced or refractory to PUVA early stage mycosis fungoides: A case series. J Eur Acad Dermatol Venereol 2011;25:354-7.
[Google Scholar]
|
| 30. |
Cheeley J, Sahn RE, DeLong LK, Parker SR. Acitretin for the treatment of cutaneous T-cell lymphoma. J Am Acad Dermatol 2013;68:247-54.
[Google Scholar]
|
| 31. |
Chiarion-Sileni V, Bononi A, Fornasa CV, Soraru M, Alaibac M, Ferrazzi E, et al. Phase II trial of interferon-alpha-2a plus psolaren with ultraviolet light A in patients with cutaneous T-cell lymphoma. Cancer 2002;95:569-75.
[Google Scholar]
|
| 32. |
Rupoli S, Barulli S, Guiducci B, Offidani M, Mozzicafreddo G, Simonacci M, et al. Low dose interferon-alpha2b combined with PUVA is an effective treatment of early stage mycosis fungoides: Results of a multicenter study. Cutaneous-T Cell Lymphoma Multicenter Study Group. Haematologica 1999;84:809-13.
[Google Scholar]
|
| 33. |
Suh KS, Roh HJ, Choi SY, Jeon YS, Doh KS, Baeet JH, et al. Long-term evaluation of erythema and pigmentation induced by ultraviolet radiations of different wavelengths. Skin Res Technol 2007;13:154-61.
[Google Scholar]
|
| 34. |
Milstein HI, Vonderheid E, Van Scott EJ, Johnson WC. Home ultraviolet phototherapy of early mycosis fungoides: Preliminary observations. J Am AcadDermatol 1982;6:355-62.
[Google Scholar]
|
| 35. |
El-Mofty M, Mostafa WZ, Bosseila M, Youssef R, Esmat S, El Ramly A, et al. A large scale analytical study on efficacy of different photo (chemo) therapeutic modalities in the treatment of psoriasis, vitiligo and mycosis fungoides. Dermatol Ther 2010;23:428-34.
[Google Scholar]
|
| 36. |
Pavlotsky F, Barzilai A, Kasem R, Shapiro D, Trau H. UVB in the management of early stage mycosis fungoides. J Eur Acad Dermatol Venereol 2006;20:565-72.
[Google Scholar]
|
| 37. |
Boztepe G, Sahin S, Ayhan M, Erkin G, Kilemen F. Narrowband ultraviolet B phototherapy to clear and maintain clearance in patients with mycosis fungoides. J Am Acad Dermatol 2005;53:242-6.
[Google Scholar]
|
| 38. |
Resnik KS, Vonderheid EC. Home UV phototherapy of early mycosis fungoides: Long-term follow-up observations in thirty-one patients. J Am Acad Dermatol 1993;29:73-7.
[Google Scholar]
|
| 39. |
Trautinger F. Phototherapy of mycosis fungoides. Photodermatol Photoimmunol Photomed 2011;27:68-74.
[Google Scholar]
|
| 40. |
Gokdemir G, Barutcuoglu B, Sakiz D, Koslu A. Narrowband UVB phototherapy for early-stage mycosis fungoides: Evaluation of clinical and histopathological changes. J Eur Acad Dermatol Venereol 2006;20:804-09.
[Google Scholar]
|
| 41. |
Hofer A, Cerroni L, Kerl H, Wolf P. Narrowband (311-nm) UV-B therapy for small plaque parapsoriasis and early-stage mycosis fungoides. Arch Dermatol 1999;135:1377-80.
[Google Scholar]
|
| 42. |
Jang MS, Baek JW, Park JB, Kang DY, Kang JS, Suh KS, et al. Narrowband ultraviolet B phototherapy of early stage mycosis fungoides in korean patients. Ann Dermatol 2011;23:474-80.
[Google Scholar]
|
| 43. |
Ponte P, Serrão V, Apetato M. Efficacy of narrowband UVB vs. PUVA in patients with early-stage mycosis fungoides. J Eur Acad Dermatol Venereol 2010;24:716-21.
[Google Scholar]
|
| 44. |
Diederen PV, van Weelden H, Sanders CJ, Toonstra J, van Vloten WA. Narrowband UVB and psoralen-UVA in the treatment of early-stage mycosis fungoides: A retrospective study. J Am Acad Dermatol 2003;48:215-9.
[Google Scholar]
|
| 45. |
Ahmad K, Rogers S, McNicholas PD, Collins P. Narrowband UVB and PUVA in the treatment of mycosis fungoides: A retrospective study. Acta Derm Venereol 2007;87:413-7.
[Google Scholar]
|
| 46. |
Drucker AM, Baibergenova A, Rosen CF, Shear NH. Narrowband UVB as an effective substitute for psoralen plus UVA: Lessons from a psoralen shortage. Photodermatol Photoimmunol Photomed 2012;28:267-8.
[Google Scholar]
|
| 47. |
Kanokrungsee S, Rajatanavin N, Rutnin S, Vachiramon V. Efficacy of narrowband ultraviolet B twice weekly for hypopigmented mycosis fungoides in Asians. Clin Exp Dermatol 2012;37:149-52.
[Google Scholar]
|
| 48. |
Wongpraparut C, Setabutra P. Phototherapy for hypopigmented mycosis fungoides in Asians. Photodermatol Photoimmunol Photomed 2012;28:181-6.
[Google Scholar]
|
| 49. |
Hassab-El-Naby HM, El-Khalawany MA. Hypopigmentedmycosisfungoides in Egyptian patients. J Cutan Pathol 2013;40:397-404.
[Google Scholar]
|
| 50. |
Akaraphanth R, Douglass MC, Lim HW. Hypopigmentedmycosis fungoides: Treatment and a 6 (1/2)-year follow-up of 9 patients. J Am Acad Dermatol 2000;42:33-9.
[Google Scholar]
|
| 51. |
Koh MJ, Chong WS. Narrow-band ultraviolet B phototherapy for mycosis fungoides in children. Clin Exp Dermatol 2014;39:474-8.
[Google Scholar]
|
| 52. |
Olek-Hrab K, Silny W, Da-czak-Pazdrowska A, Osmola-Ma-kowska A, Sadowska PA, Polanska A, et al. Ultraviolet A1 phototherapy for mycosis fungoides. Clin Exp Dermatol 2013;38:126-30.
[Google Scholar]
|
| 53. |
Zane C, Leali C, Airò P, De Panfilis G, Pinton PC. "High-dose" UVA1 therapy of widespread plaque-type, nodular, and erythrodermicmycosis fungoides. J Am Acad Dermatol 2001;44:629-33.
[Google Scholar]
|
| 54. |
Aydogan K, Yazici S, BalabanAdim S, TilkiGunay I, Budak F, Saricaoglu H, et al. Efficacy of low-dose ultraviolet a-1 phototherapy for parapsoriasis/early-stage mycosis fungoides. Photochem Photobiol 2014;90:873-7.
[Google Scholar]
|
| 55. |
El Mofty M, Ramadan S, Fawzy MM, Hegazy RA, Sayed S. Broad band UVA: A possible reliable alternative to PUVA in the treatment of early-stage mycosis fungoides. Photodermatol Photoimmunol Photomed 2012;28:274-7.
[Google Scholar]
|
| 56. |
Jang MS, Kang DY, Jeon YS, Kim ST, Suh KS. Ultraviolet A1 phototherapy of mycosis fungoides. Ann Dermatol 2013;25:104-7.
[Google Scholar]
|
| 57. |
Plettenberg H, Stege H, Megahed M, Ruzicka T, Hosokawa Y, Tsuji T, et al. Ultraviolet A1 (340~400 nm) phototherapy for cutaneous T-cell lymphoma. J Am Acad Dermatol 1999;41:47-50.
[Google Scholar]
|
| 58. |
Passeron T, Zakaria W, Ostovari N. Efficacy of the 308-nm excimer laser in the treatment of mycosis fungoides. Arch Dermatol 2004;140:1291-3.
[Google Scholar]
|
| 59. |
Kontos AP, Kerr HA, Malick F, Fivenson DP, Lim HW, Wong HK. 308-nm excimer laser for the treatment of lymphomatoidpapulosis and stage IA mycosis fungoides. Photodermatol Photoinmmunol Photomed 2006;22:168-71.
[Google Scholar]
|
| 60. |
Upjohn E, Foley P, Lane P. Long-term clearance of patch-stage mycosis fungoides with the 308-nm excimer laser. Clin Exp Dermatol 2007;32:168-71.
[Google Scholar]
|
| 61. |
Passeron T, Angeli K, Cardot-Leccia N, Perrin C, Lacour JP, Ortonne JP. Treatment of mycosis fungoides by 308-nm excimer laser: A clinical and histological study in 10 patients. Ann Dermatol Venereol 2007;134:225-31.
[Google Scholar]
|
| 62. |
Nistico S, Costanzo A, Saraceno R, Chimenti S. Efficacy of monochromatic excimer laser radiation (308 nm) in the treatment of early stage mycosis fungoides. Br J Dermatol 2004;151:877-9.
[Google Scholar]
|
| 63. |
Mori M, Campolmi P, Mavilia L, Rossi R, Cappugi P, Pimpinelli N. Monochromatic excimer light (308 nm) in patch-stage IA mycosis fungoides. J Am Acad Dermatol 2004;50:943-5.
[Google Scholar]
|
| 64. |
Nistico SP, Saraceno R, Schipani C, Costanzo A, Chimenti S. Different applications of monochromatic excimer light in skin diseases. Photomed Laser Surg 2009;27:647-54.
[Google Scholar]
|
| 65. |
Deaver D, Cauthen A, Cohen G, Sokol L, Glass F. Excimer laser in the treatment of mycosis fungoides. See comment in PubMed Commons belowJ Am Acad Dermatol 2014;70:1058-60.
[Google Scholar]
|
| 66. |
Morison WL, Baughman RD, Day RM. Consensus workshop on the toxic effects of long-term PUVA therapy. Arch Dermatol 1998;134:595-8.
[Google Scholar]
|
| 67. |
Sánchez MA, González T, Gaitán MF, Zuluaga A, Jiménez SB, de Galvis YT. Is PUVA maintenance therapy necessary in patients with early-stage mycosis fungoides? Evaluation of a treatment guideline over a 28-month follow-up. Int J Dermatol 2011;50:1086-93.
[Google Scholar]
|
| 68. |
Elcin G, Duman N, Karahan S, Ersoy-Evans S, Erkin G, Karaduman A, et al. Long-term follow-up of early mycosis fungoides patients treated with narrowband ultraviolet B phototherapy. J Dermatolog Treat 2014;25:268-73.
[Google Scholar]
|
Fulltext Views
12,219
PDF downloads
3,383





