Translate this page into:
Pilomatricoma with a bullous appearance
Correspondence Address:
Jian-You Wang
Department of Dermatology, Second Affiliated Hospital, Zhejiang University School of Medicine, 88 Jiefang Rd, Hangzhou, Zhejiang, 310009
China
| How to cite this article: Cao HL, Chen JS, Yan JL, Wang JY. Pilomatricoma with a bullous appearance. Indian J Dermatol Venereol Leprol 2015;81:77-78 |
Sir,
Pilomatricoma is a benign skin tumor generally characterized by a firm, deep-seated nodule. Pilomatricoma with a bullous appearance is rarely reported. Diagnosis in such cases is difficult prior to histopathologic examination due to its atypical presentation. We report the case of a 24-year-old man who presented with a bullous lesion on his right shoulder which showed features of pilomatricoma on histology.
A previously healthy 24-year-old man presented with a nodule with an overlying blister on his right shoulder. He had a 4-month history of a small cutaneous nodule which enlarged and developed bullous change one month previously. The lesion was not preceded by local trauma or insect bite. Dermatological examination revealed a semi-translucent, thick-walled, and pink-colored bulla on the right shoulder, 35 × 30 mm in size underlying which a hard nodule was palpable [Figure - 1]. There was no regional lymphadenopathy and the remainder of the physical examination was unremarkable. Hematologic, biochemical, and urinalysis results were normal. The lesion was excised completely.
 |
| Figure 1: A bullous mass on the right shoulder of the patient |
Histopathologic examination revealed tumor nests in the dermis composed of basophilic cells and shadow cells surrounded by a fibrous capsule [[Figure - 2]a, b]. Foci of calcification and giant cell reaction were observed [[Figure - 2]c]. Lymphedema and dilated lymphatic vessels were observed in the superficial dermis [[Figure - 2]d]. A diagnosis of bullous pilomatricoma was made. The patient was clinically free of disease at a recent follow-up, 3 years after treatment.
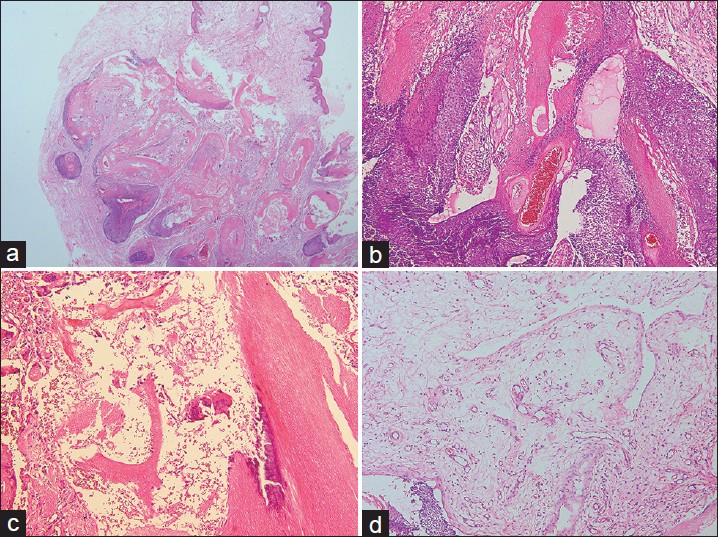 |
| Figure 2: Histology of the lesion. (a), Histopathology showed edema in the superficial dermis and tumor nests in the deep dermis. (b), The tumor nests were composed of basophilic cells and shadow cells. (c), Foci of calcification and giant cell reaction were observed in the tumor mass. (d), Lymphedema and dilated lymphatic vessels were observed in the superficial dermis. (hematoxylin-eosin, original magnification: (a), ×20; (b), (c), (d), ×100) |
Pilomatricoma is a cutaneous neoplasm of hair matrix origin with differentiation toward the cells of the outer root sheath, [1] and is usually characterized by a solitary cutaneous nodule located on the head or neck. [2] It is typically a tumor of childhood, and females are more commonly affected than males. [3] Multiple pilomatricomas and familial cases can be associated with Curschmann-Steinert myotonic dystrophy, Gardner′s syndrome, Rubinstein-Taybi syndrome, and other genetic disorders. [4] Some pilomatricomas are caused by mutations in the beta-catenin gene. [5] However, in the literature review of the patients with bullous pilomatricoma by Chen et al., none of them had any of these related genetic disorders. [3] Instead, mechanical irritation and trauma could be the most likely contributing factors.
On histological examination, pilomatricomas often present with transformation of basophilic basaloid tumor cells to eosinophilic shadow or "ghost" cells at the center of the tumor. [2] In bullous pilomatricoma, dilated lymphatic vessels and severe lymphedema in the dermis overlying a typical pilomatricoma are observed in most cases. [3] The etiopathogenesis of bullous pilomatricoma is not fully understood. The widely accepted theory is that the pilomatricoma induces obstruction of lymphatic vessels and congestion of lymphatic fluid. This subsequently results in the dilation of lymphatic vessels, leakage of lymph, and edema in the dermis. External pressure is postulated to be the cause of the lymphedema. Thus, bullous pilomatricoma is also named as lymphangiectatic pilomatricoma. [2] In addition, the bullous form of pilomatricoma is usually characterized by anetodermic cutaneous changes and marked reduction of elastic fibers in the dermis above the pilomatricoma. [6] It is postulated that elastinolytic enzymes produced by tumor cells may be responsible for the reduction of elastic fibers.
The most common differential diagnosis for this type of lesion is lymphangioma, along with a wide range of other possible diagnoses, such as malignancy, secondary anetoderma, or bullous morphea. For pilomatricomas, surgical incision or curettage is the treatment of choice. Malignant transformation is exceedingly rare.
| 1. |
Simi CM, Rajalakshmi T, Correa M. Pilomatricoma: A tumor with hidden depths. Indian J Dermatol Venereol Leprol 2010;76:543-6.
[Google Scholar]
|
| 2. |
Julian CG, Bowers PW. A clinical review of 209 pilomatricomas. J Am Acad Dermatol 1998;39:191-5.
[Google Scholar]
|
| 3. |
Chen SY, Wu F, Qian Y, Zhu L, Tu YT, Huang CZ. Pilomatricoma with bullous appearance: A case report and review of literature. Int J Dermatol 2011;50:615-8.
[Google Scholar]
|
| 4. |
Wachter-Giner T, Bieber I, Warmuth-Metz M, Brocker EB, Hamm H. Multiple pilomatricomas and gliomatosis cerebri-a new association? Pediatr Dermatol 2009;26:75-8.
[Google Scholar]
|
| 5. |
Chan EF, Gat U, McNiff JM, Fuchs E. A common human skin tumour is caused by activating mutations in beta-catenin. Nat Genet 1999;21:410-3.
[Google Scholar]
|
| 6. |
Jones CC, Tschen JA. Anetodermic cutaneous changes overlying pilomatricomas. J Am Acad Dermatol 1991;25:1072-6.
[Google Scholar]
|
Fulltext Views
4,218
PDF downloads
3,220





