Translate this page into:
Pinch-punch technique for scrotal calcinosis cutis
Corresponding author: Dr. Arpita Nibedita Rout, Department of Dermatology and Venereology, All India Institute of Medical Sciences, Bhubaneswar, Odisha, India. arpitanrout1988@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Rout AN, Pradhan S, Sirka CS. Pinch-punch technique for scrotal calcinosis cutis. Indian J Dermatol Venereol Leprol 2021;87:858-60.
Sir,
Scrotal calcinosis cutis is a benign condition which usually occurs at a young age or in early adulthood.1 The condition manifests as solitary or multiple, asymptomatic calcified nodules or papules on the scrotum. It may be associated with pruritus, feeling of heavy sensation, discharge of white chalky material, secondary bacterial infection or a combination of all these features. The term idiopathic scrotal calcinosis is used in the absence of any systemic disorder of the calcium/phosphorus metabolism.1 Treatment of scrotal calcinosis is intended to address the associated symptoms as well as to preserve cosmesis. Surgery is the usual mode of treatment in scrotal calcinosis. Various surgical methods practiced for the condition include enucleation, wide local excision with direct closure and complex scrotal reconstruction.2 Pinch-punch technique has been described as a novel method for removal of calcinosis cutis in patients with fewer and smaller lesions.3 In this case series, we intend to report the outcomes of 12 patients with scrotal calcinosis who were managed by pinch-punch technique.
A total of 12 patients with age ranging from 18 to 33 years, who presented with a total of 92 calcinosis cutis nodules of size less than one centimeter over the scrotum were managed by the pinch-punch technique, during the past one year. Most of the patients (10/12, 83.3%) were unmarried. The duration of the lesions at the time of presentation ranged from one to eight years with most (9/12, 75%) of the lesions being asymptomatic and the rest reporting occasional itching. The reasons for seeking treatment were fear of future complications (10/12, 83.3%) and cosmesis (6/12, 50%). The number of nodules ranged from two to 15 per patient.
Before the procedure, routine investigations like screening for HIV, HBsAg, HCV and serum calcium levels were done in all cases. Serum calcium and phosphate levels were normal in all. Consent for the procedure was obtained from all the patients. The area was cleaned with spirit, lignocaine 2% was injected locally by insulin syringe. The nodule was pinched with the thumb and index finger to stretch the overlying skin and with the help of a disposable skin biopsy punch (3–4 mm), the superficial skin of the nodule was removed. Subsequently, the nodule was squeezed from the base and the sides with an artery forceps which led to the easy removal of intact calcified nodule [Figures 1-4]. After removal, hemostasis was obtained by local pressure for around 5–10 min. In case of lesions larger than 0.5 cm, single suture was done with Prolene 4.0 which was removed after seven days. Oral and topical antibiotics were prescribed to all for seven days with the advice of cleaning the area daily with normal water. Oral analgesics were advised as and when required basis. All cases were followed up weekly for two weeks post-procedure to look for any adverse effects at the site of surgery.

- The base of the nodule has been held between index finger and thumb (pinch) and skin is cut by disposable skin biopsy punch

- The superficial skin separated by disposable skin biopsy punch and the nodule pressed from below with artery forceps

- The intact nodule coming out through the gap in the skin
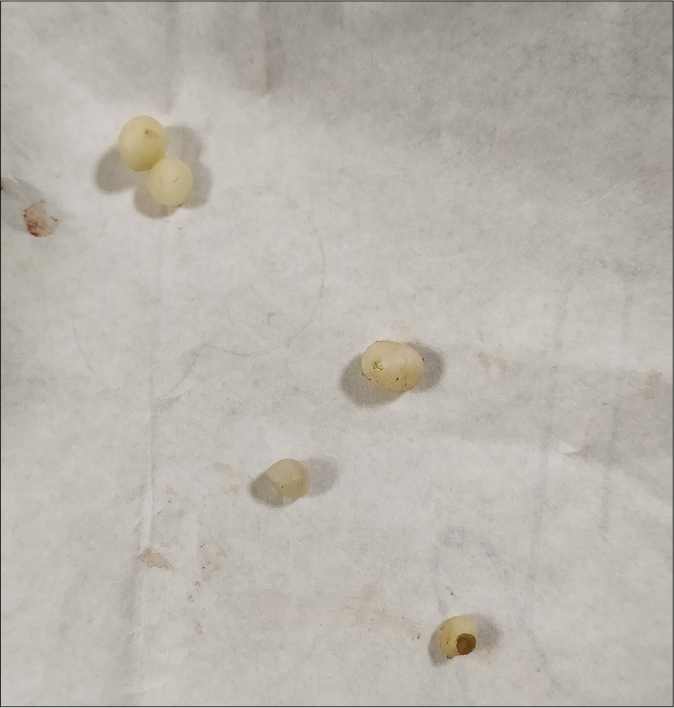
- Intact nodules removed
Out of 92 nodules, 59 came out en masse, 32 ruptured and the sac was pulled out with artery forceps; only one case required excision. There was minimal hemorrhage during the procedure, and in visual analog scale, the pain during the procedure was graded from one to three by all the patients. There was no down time for any of the patients and all of them could join their work on the next day. None of the patients required oral analgesics for more than two days. Resultant scarring was acceptable for all the patients. There was no suture site infection in any of the patients.
Due to the indolent and painless nature, usually, there is a delay in treatment seeking behavior. All of our patients sought medical advice for cosmetic reasons and apprehension.
Surgery is the treatment of choice and provides excellent results in scrotal calcinosis. “In toto excision” procedure is the most convenient option, but needs meticulous precision to limit the excision process to dermis level so as to avoid damage to dartos layer. In case of numerous lesions, the procedure can be tedious, expensive and time consuming requiring multiple sittings.4 There may be extensive loss of scrotal skin in traditional procedures which calls for inclusion of the surgical specialists to manage complications.5 The other traditional procedures such as enucleation, wide local excision and scrotal reconstruction are complex, time consuming, require expertise, have long down time and can result in extensive scarring. A similar minimally invasive technique with incision (either with 11 – no surgical blade or cautery) and expression of content followed by pulling out the sac with forceps through the opening has been described for steatocystoma multiplex.6,7 The present procedure helps in removing the redundant skin over the nodule, thus there is minimal chance of bag-like outpunching.
In conclusion, the pinch-punch technique described by by Chang et al. is an easy, convenient, method suitable as an out-patient procedure for less extensive scrotal calcinosis with minimal scarring and has an easy learning curve. It is less painful and convenient for the patients also.3 We report this case series to bring about awareness regarding this easy technique.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Idiopathic scrotal calcinosis: Report of 2 cases, and review of pathogenesis and factors that determine patients' acceptance of surgical treatment. Clin Cosmet Investig Dermatol. 2018;11:333-7.
- [CrossRef] [Google Scholar]
- Idiopathic scrotal calcinosis: A non-elucidated pathogenesis and its surgical treatment. Rev Urol. 2011;13:95-7.
- [Google Scholar]
- Surgical Pearl: Pinch-punch excisions for scrotal calcinosis. J Am Acad Dermatol. 2004;50:780-1.
- [CrossRef] [Google Scholar]
- Idiopathic scrotal calcinosis: A new case report. Urol Case Rep. 2020;32:101225.
- [CrossRef] [Google Scholar]
- A simple surgical technique for the treatment of steatocystoma multiplex. Int J Dermatol. 2001;40:785-8.
- [CrossRef] [Google Scholar]
- A modified surgical technique for steatocystoma multiplex. J Cutan Aesthet Surg. 2010;3:25-8.
- [CrossRef] [Google Scholar]





