Translate this page into:
Pityriasis rubra pilaris mixed type III/IV successfully treated with narrow band-ultraviolet B
2 Hospital de Santa Maria - Centro Hospitalar de Lisboa Norte, Lisboa, Portugal
Correspondence Address:
A F Massa
Department of Dermatology, Centro Hospitalar de V.N.Gaia/Espinho, EPE, R. Conceiç�o Fernandes, 4430 Vila Nova de Gaia
Portugal
| How to cite this article: Massa A F, Vasconcelos P, de Almeida L S, Filipe P. Pityriasis rubra pilaris mixed type III/IV successfully treated with narrow band-ultraviolet B. Indian J Dermatol Venereol Leprol 2015;81:435 |
Sir,
Pityriasis rubra pilaris (PRP) is a rare papulo-squamous disorder of childhood. Its presentation is characterized by a cephalocaudal cutaneous eruption of follicular hyperkeratotic papules with characteristic islands of spared skin along with palmoplantar keratoderma as a frequent feature. Pityriasis rubra pilaris in children, according to Griffiths′ classification, [1] is divided into 3 types type III, classic juvenile type, similar to adult type-I classic pityriasis rubra pilaris with a generalized eruption, type IV, circumscribed juvenile pityriasis rubra pilaris presenting over the knees and elbows as well-demarcated hyperkeratotic erythematous plaques, and type V, atypical juvenile type presenting in childhood but with a more chronic course and a scleroderma-like appearance of palms and soles.
We report an 8-year-old Caucasian girl, phototype II, who developed an erythematous eruption for 1 month. She had no previous personal or family history of cutaneous disease and a previous respiratory tract infection was denied. On physical examination, an erythematous eruption of follicular micro-papules with scaling was observed over the entire skin, more intense on the face and trunk with thick hyperkeratotic plaques on the knees and elbows and palmoplantar keratoderma with a yellowish-orange tint [Figure - 1].
 |
| Figure 1: Disseminated erythematous eruption of follicular micropapules with scaling, hyperkeratotic plaques in the knees and elbows, and palmoplantar keratoderma with a yellowish-orange tint |
Skin biopsy showed regular acanthosis of the epidermis, a preserved granular layer covered by a checkerboard pattern of alternating ortho- and parakeratosis and a lymphocytic perivascular infiltrate in the superficial dermis [Figure - 2], consistent with the clinical diagnosis of pityriasis rubra pilaris. The presence of a widespread eruption in addition to well-defined hyperkeratotic plaques suggested mixed type III/IV disease.
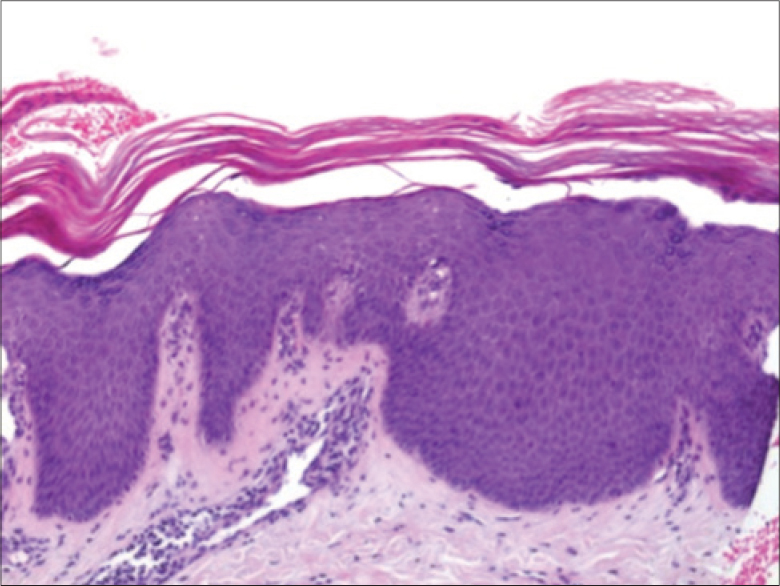 |
| Figure 2: Histologic aspects: Alternating ortho- and parakeratosis, psoriasiform epidermal hyperplasia, and focal superficial dermal perivascular lymphocytes (H and E, ×40) |
Treatment was initiated with emollients, hydrocortisone cream on the face, and topical vitamin D analog, calcipotriene on the body with little improvement observed after a week. Narrow-band ultraviolet-B (NB-UVB) was added while maintaining regular topical treatment for another week. Subsequently, NB-UVB and emollients were administered for 2 months and then stopped. With a total of 19 sessions and a cumulative dose of 10.5 J/cm 2 , more than 90% improvement was observed with just two residual lesions on the knees. After 18 months of follow-up, without any further treatment apart from the use of emollients, the patient remained free of lesions and no recurrence was observed [Figure - 3].
 |
| Figure 3: (a and b) After treatment, two residual lesions are found on the knees. (c– f) After 18 months of follow-up, no lesions are observed |
We report a case of childhood pityriasis rubra pilaris with clinical aspects that do not fit completely into type IV of Griffiths′ [1] classification. It also presented with a more widespread eruption in the upper half of the body, in what could be a mixed type III/IV disease, although the circumscribed form usually does not evolve into the classical type. The histological findings of alternating orthokeratosis and parakeratosis in both vertical and horizontal axes were compatible with that typically described for pityriasis rubra pilaris.
Pityriasis rubra pilaris is a rare disease with some cases being recalcitrant and resistant to treatment. The most effective treatment, especially in children, remains controversial. Systemic retinoids are often considered the first choice of treatment for this hyperkeratotic entity. [2] Although the disease can be phototriggered, phototherapy seems to be an effective option. There are some encouraging case reports of successful treatment with NB-UVB [3] including the combination of acitretin and UVB light treatment (ReUVB). [4] In the case of an UVB phototriggered patient, bath psoralen and ultraviolet A (PUVA) can be used as a rescue option. [5] Modified Goeckerman regimen (tar + UVB) is reported to have moderate efficacy. [2]
ACKNOWLEDGMENT
We would like to acknowledge Prof. João Borges da Costa for his review of the manuscript.
| 1. |
Griffiths W. Pityriasis rubra pilaris. Clin Exp Dermatol 1980;5:105-12.
[Google Scholar]
|
| 2. |
Allison DS, El-Azhary RA, Calobrisi SD, Dicken CH. Pityriasis rubra pilaris in children. J Am Acad Dermatol 2002;47:386-9.
[Google Scholar]
|
| 3. |
Vergilis-Kalner IJ, Mann DJ, Wasserman J, Petronic-Rosic V, Tsoukas MM. Pityriasis rubra pilaris sensitive to narrow band-ultraviolet B light therapy. J Drugs Dermatol 2009;8:270-3.
[Google Scholar]
|
| 4. |
Kirby B, Watson R. Pityriasis rubra pilaris treated with acitretin and narrow-band ultraviolet B (Re-TL-01) Br J Dermatol 2000;142:376-7.
[Google Scholar]
|
| 5. |
Kaskel P, Grundmann-Kollmann M, Schiller PI, Krähn G, Pillekamp H, Peter RU, et al. Bath PUVA as a treatment for pityriasis rubra pilaris provoked by ultraviolet B. Br J Dermatol 1999;140:769-70.
[Google Scholar]
|
Fulltext Views
4,631
PDF downloads
2,345





