Translate this page into:
Pityriasis versicolor in the pediatric age group
Correspondence Address:
Binayak Chandra Dwari
Plot No. 8, Phase-IV, Adarsha Vihar, Bhubaneswar - 31, Orissa
India
| How to cite this article: Jena DK, Sengupta S, Dwari BC, Ram MK. Pityriasis versicolor in the pediatric age group. Indian J Dermatol Venereol Leprol 2005;71:259-261 |
Abstract
BACKGROUND: Pityriasis versicolor (PV) is a mild chronic infection of the skin caused by Malassezia yeasts. Although it is primarily seen in adults, children are often affected in the tropics . METHODS: Over a period of 2 years, children (up to the age of 14 years) who were clinically and mycologically diagnosed as PV were included in the study. The clinical and epidemiological pattern in different age groups was noted. RESULTS: PV in this age group formed about 31% of the total cases of PV; 4.8% cases presented in infancy. The commonest site of involvement was the face in 39.9% of the cases. Most of the cases presented in summer months. CONCLUSIONS: PV is not an uncommon disease among children in the tropics. There is a sudden resurgence of cases in the hot monsoons and even infants are not spared.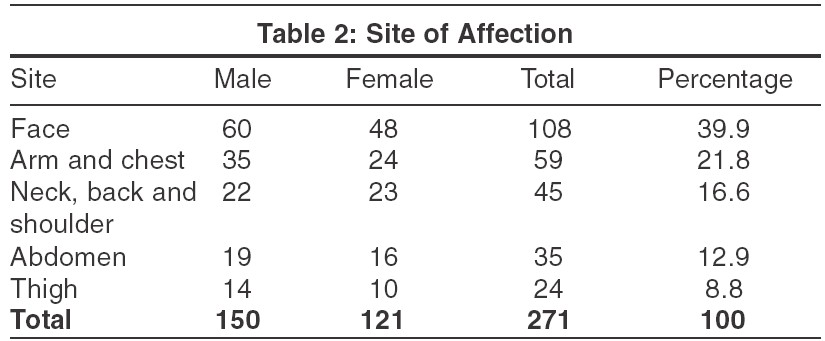
 |
 |
INTRODUCTION
Pityriasis versicolor (PV) is a superficial mycosis, affecting the superficial layer of stratum corneum.[1] The causative organism is Malassezia furfur , a yeast-like lipophilic fungus. Previously the mycelial form was called either P. ovale or P. orbiculare .[2] In 1951, Gordon isolated the organism M. furfur and renamed it P. orbiculare . It was recognized that M. furfur is the correct name and that P. orbiculare , P. ovale , and M. ovalis are synonyms.[3] The disease is most prevalent in early adulthood and small children are rarely affected.[3],[4],[5],[6] PV is common in the post-pubertal age where sebaceous glands are active and in individuals who sweat more.[7] There is often a positive family history of the disease.[10]
An increase in humidity, temperature and carbon dioxide tension are important predisposing factors.[3],[5] The prevalence in colder climates is less than 1%.[8] M. furfur is a component of the normal skin flora in more than 90% of adults living in tropical areas.[14] PV, consequently, is more common in the tropics than in temperate zones.[2]
MATERIALS AND METHODS
Two hundred and seventy one cases of PV up to the age of 14 years attended the Dermatology OPD of the S.C.B. Medical College, Cuttack during the study period of 2 years. They were diagnosed based on clinical criteria and confirmed by Wood′s lamp examination and demonstration of organisms by 10% KOH examination of skin scrapings.
RESULTS
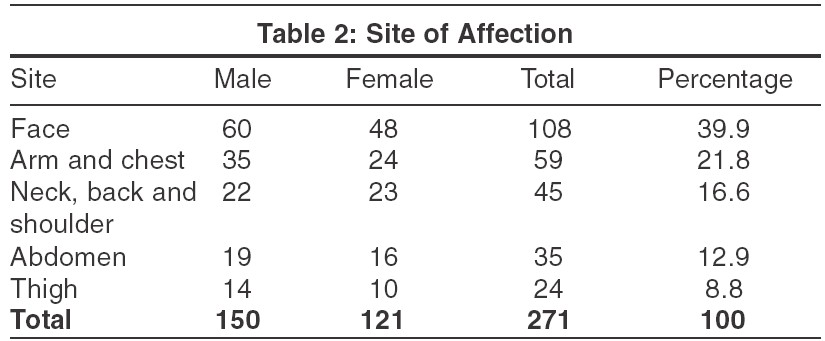
In the study period of 2 years, 271 children were diagnosed with PV, accounting for 31% of the total PV cases attending the outpatient department. There were 150 boys and 121 girls. The majority of patients were aged 8-12 years [Table - 1], but 10 infants (3.7%) were also affected. The duration of infection was less than 6 months in all cases.
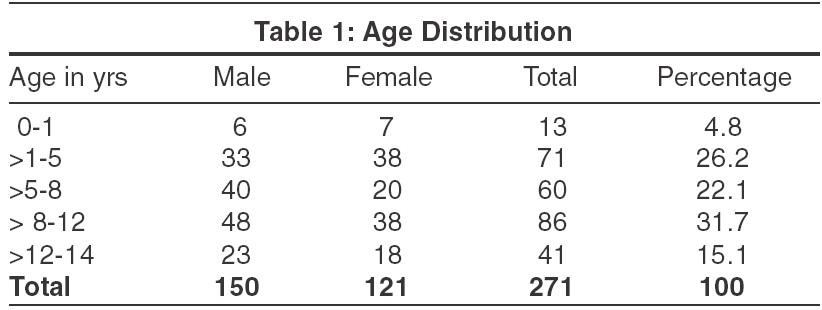
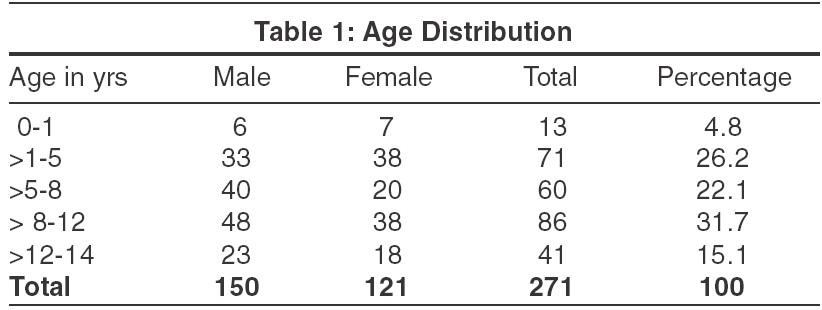
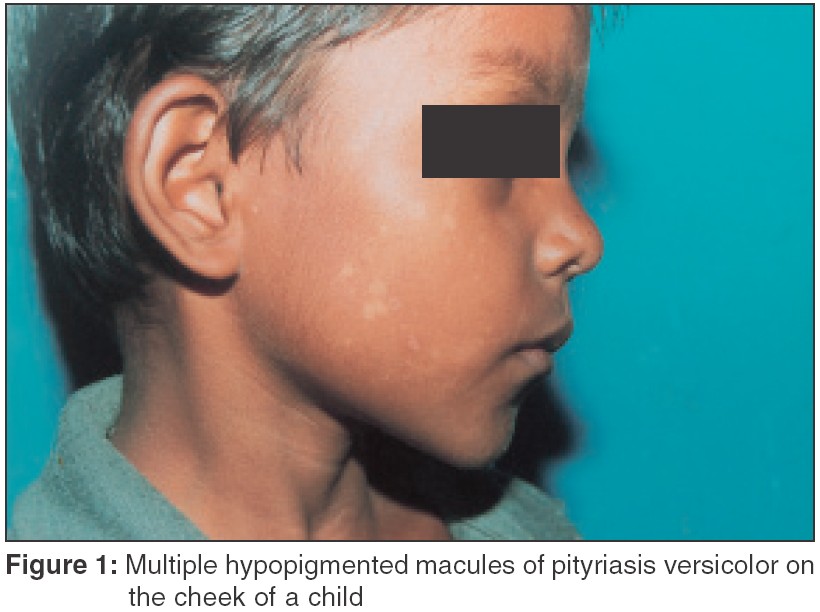
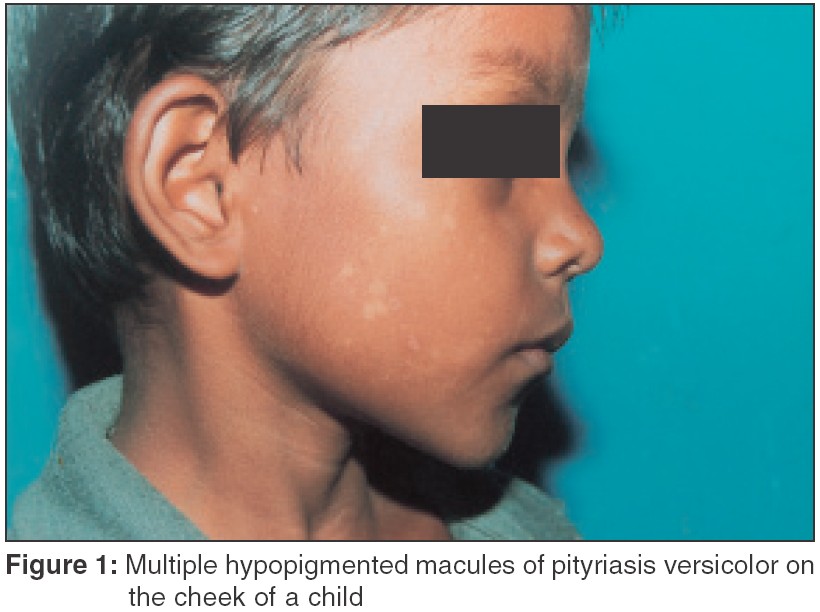
Many patients (102 [37.6%]) gave history of profuse sweating and some of these (26 [9.6%]) had mild pruritus. All patients had characteristic skin lesions, achromic or hypochromic macules with an irregular margin. Hyperpigmented macules with mild scaling were present in 28 [9.3%]. The most common site involved was the face (39%) [Table - 2]. Extensive involvement was seen in 45 [16.6%] children with lesions on the neck, shoulder and back.
Majority of cases (186 [68.6%]) presented between June and November [Figure - 1], when the environmental temperature and relative humidity are quite high in Cuttack. None of the children had any associated systemic disease. A large majority of the children (194 [71.6%]) hailed from the lower and middle socioeconomic groups. Six per cent cases (16 patients) had a family history of PV.
On microscopic examination hyphal forms were found in 196 cases [72.3%] and the "spaghetti and meat ball" (hyphae and spores) pattern in the rest [27.7%].
DISCUSSION
We observed a marked increase in the incidence of PV during the summer and monsoon and a sudden fall in December to February. Michalowski et al and Terragni et al also found a similar increased incidence during the warmer months.[9],[10] In an Indian study by Miskeen, 71.2% of cases were seen in the hot months of May to October.[15]
The most common age group involved was 8-12 years. Most of the patients in a study by Silva et al were in the 11-15 years age group.[11] In addition, 10 infants were found to be affected in our study. Di silverio et al also reported PV in infants.[6] None of the cases were associated with systemic diseases.
The most commonly involved site was the face (39.9%), which was observed by Akpata et al[12] and Terragni et al too.[13] In fact, Terragni et al opine that the face is usually the only site affected by PV in children, in contrast to adults.[12] The thigh and legs were also affected, which is unusual in adults. PV lesions over the face were smaller than those present on the trunk.
On microscopic examination we found the hyphal forms to be commoner [72.3% cases] than the "spaghetti and meat ball" (hyphae and spores) pattern [27.7%]. This finding is in contrast to the observation that in adult patients with PV, the ′hyphae and spore′ pattern is the commonest finding. We have not been able to explain the cause of this variation but this particular observation was also found in another Indian study by Miskeen et al.[15]
In conclusion, we believe that PV is not an uncommon disease in children. We have also noticed a sudden spurt of the disease in children during the monsoons, and even infants are not spared.
| 1. |
Marcon MJ, Powell DA. Human infection due to malassezia Spp. Clin Microbiol Rev 1992;5:101-19.
[Google Scholar]
|
| 2. |
Hay RJ, Moore M. Mycology. In: Champion RH, Burton JL, Burns DA, et al , editors. Book of Dermatology. 6th edn. England: Blackwell Science Oxford; 1998. p. 1277-90
[Google Scholar]
|
| 3. |
Silva - Lizama E. Tinea versicolor. Int J Dermatol 1995;34:611-7
[Google Scholar]
|
| 4. |
Sohnle PG. Dermatophytosis. In: Cox RA, editor. Immunology of Fungal Diseases. CRC Press: Florida; 1989. p. 1-27.
[Google Scholar]
|
| 5. |
Boussida S, Boudaya S, Ghorbel R, Meziou TJ, Markkekehi S, Turki H, et al. Pityriasis versicolor in children: a retrospective study of 164 cases. Ann Dermatol Venereol 1998;125:581-4.
[Google Scholar]
|
| 6. |
Di Silverio D, Zeccara C, Serra F, Ubezio S, Mosca M. Pityriasis versicolor in a new born. Mycoses 1995;38:227-8.
[Google Scholar]
|
| 7. |
Schmidt A. Malassezia furfur : A fungus belonging to the physiological skin flora and its relevance in skin disorders. Cutis 1997;59:21-4.
[Google Scholar]
|
| 8. |
Rippon JW. Dermatophytosis and dermatophytomycosis. In: Medical Mycology. 2nd ed. Philadelphia: WB Saunders; 19820. p. 154-9.
[Google Scholar]
|
| 9. |
Michalowski R, Rodziewicz H. Pityriasis versicolor in children. Br J Dermatol 1963;75:397-400.
[Google Scholar]
|
| 10. |
Terragni L, Lasagni A, Oriani A, Gelmetti C. Pityriasis versicolor in the pediatric age. Pediatr Dermatol 1991;8:9-12.
[Google Scholar]
|
| 11. |
Silva V, Di Tilia C, Fischman O. Skin colonization by Malassezia furfur in healthy children upto 15 years old. 1995;132:142-5.
[Google Scholar]
|
| 12. |
Akpata LE, Gugnani HC, Utsalo SJ. Pityriasis versicolor in school children in cross River state of Nigeria. Mycoses 1990;33:549-51.
[Google Scholar]
|
| 13. |
Terragni L, Lasagni A, Oriani A. Pityriasis versicolor of the face. Mycoses 1991;34:345-7.
[Google Scholar]
|
| 14. |
Faergemann J, Freidriksson T. Experimental infections in rabbits and human with pityriasporum orbiculare or pityrosporum ovale. J Invest Dermatol 1981;77:314-8.
[Google Scholar]
|
| 15. |
Miskeen AK, Kelkar SS, Shroff HJ. Pityriasis versicolor in children. Indian J Dermatol Venereol Leprol 1984;50:144-6.
[Google Scholar]
|
Fulltext Views
6,708
PDF downloads
2,702





