Translate this page into:
Polymorphic presentation of disseminated cutaneous rhinosporidiosis in an immunocompetent individual
2 Department of Pathology, Self Employed, Bhubaneswar, Odisha, India
Correspondence Address:
Chandra Sekhar Sirka
Department of Dermatology, All India Institute of Medical Sciences, Bhubaneswar, Odisha
India
| How to cite this article: Pradhan S, Sirka CS, Baisakh MR. Polymorphic presentation of disseminated cutaneous rhinosporidiosis in an immunocompetent individual. Indian J Dermatol Venereol Leprol 2018;84:614-617 |
Sir,
Rhinosporidiosis is a chronic granulomatous and localized infection of the mucous membranes caused by Rhinosporidium seeberi.[1] It often involves the nasopharynx and presents as painless, friable polyps. Cutaneous involvement is quite rare. Among cutaneous variants, disseminated cutaneous rhinosporidiosis has been rarely reported in the literature.[2] Here, we report a case of disseminated cutaneous rhinosporidiosis presenting with different morphologies at different body sites, such as lipoma, cutaneous horn, molluscum contagiosum, subcutaneous plaques with pigmentary change, wart and pyogenic granuloma.
A 32-year-old male presented to the dermatology out-patient department of All India Institute of Medical Sciences with multiple swellings on the body for 3 years. He had a history of recurrent nose bleeding, nasal stuffiness and difficulty in breathing because of the nasal mass. He was diagnosed with nasal rhinosporidiosis and was operated for the same thrice in 4 years. The most recent surgery was done 4 months back. Skin lesions appeared 1year after nasal lesions. The patient was a farmer by occupation and used to take baths in the pond. There was no history of visit to the American continent anytime in the past. On examination, the patient had six types of skin lesions that included lipoma-like lobulated subcutaneous swellings on the extremities and trunk of size ranging from 2 cm×2 cm to 15 cm×10 cm and were soft to firm in consistency [Figure - 1]a. Erythematous shiny nodules of approximately 5cm × 6 cm were present on the left forearm; they had hemorrhagic crusts and dilated blood vessels on the surface giving the appearance of pyogenic granuloma [Figure - 1]a. There were plaques of size vaying from 2 cm × 2cm to 6 cm ×8 cm in the inner aspect of the left arm and posterior aspect of the trunk with pigmentary change on the surface [Figure - 1]b. On the left side of the neck, there were pearly white papules resembling molluscum contagiosum [Figure - 2]a. On the chest there were papules and nodules; a few lesions on the cheeks and lumbar area had verrucosity on the surface, which appeared as warts[Figure - 2]b. The lesion on the left anterior chest had a verrucous projection on the surface which mimicked a cutaneous horn.[Figure - 2]c. Other systemic examination was unremarkable.
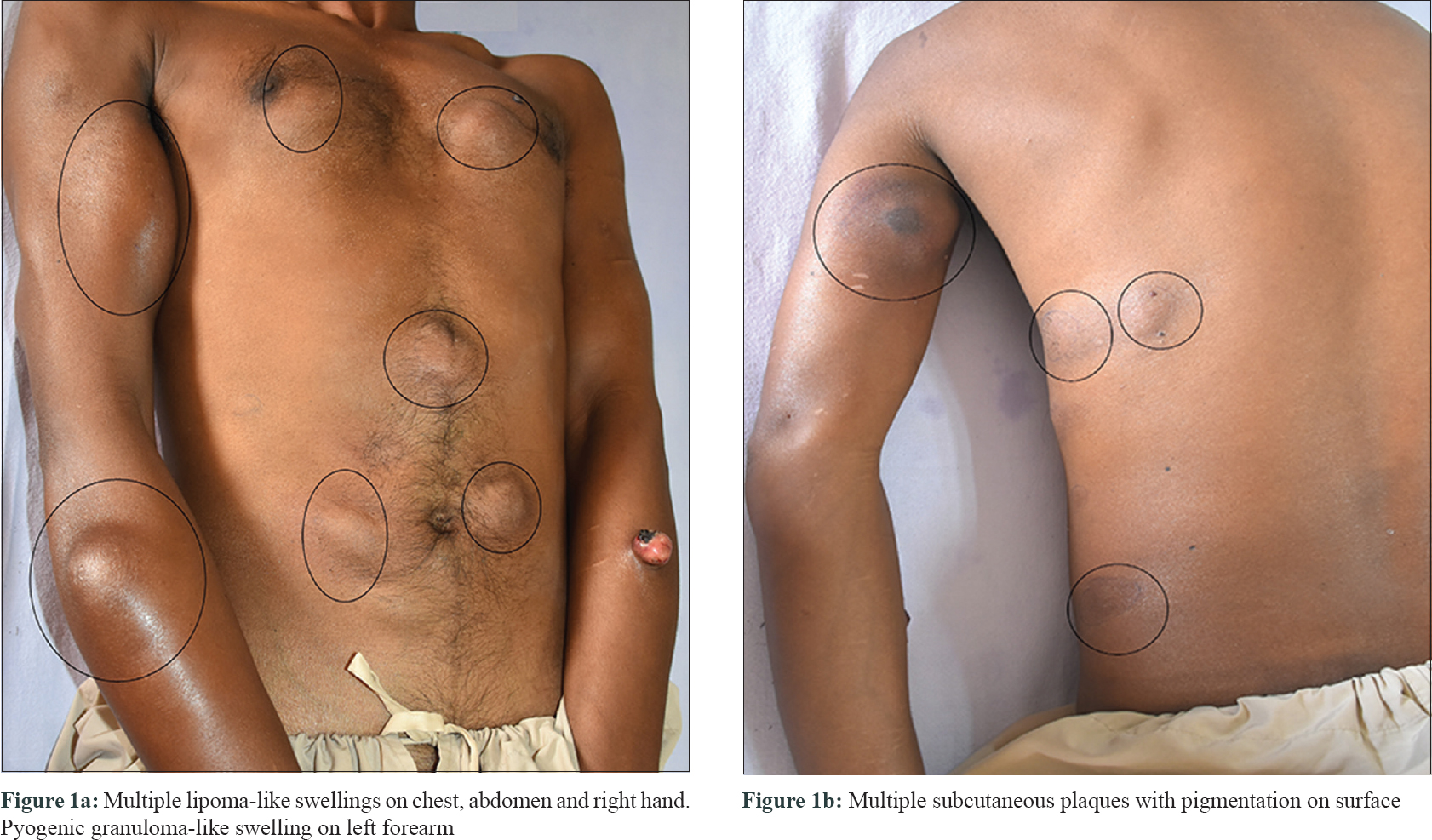 |
| Figure 1: |
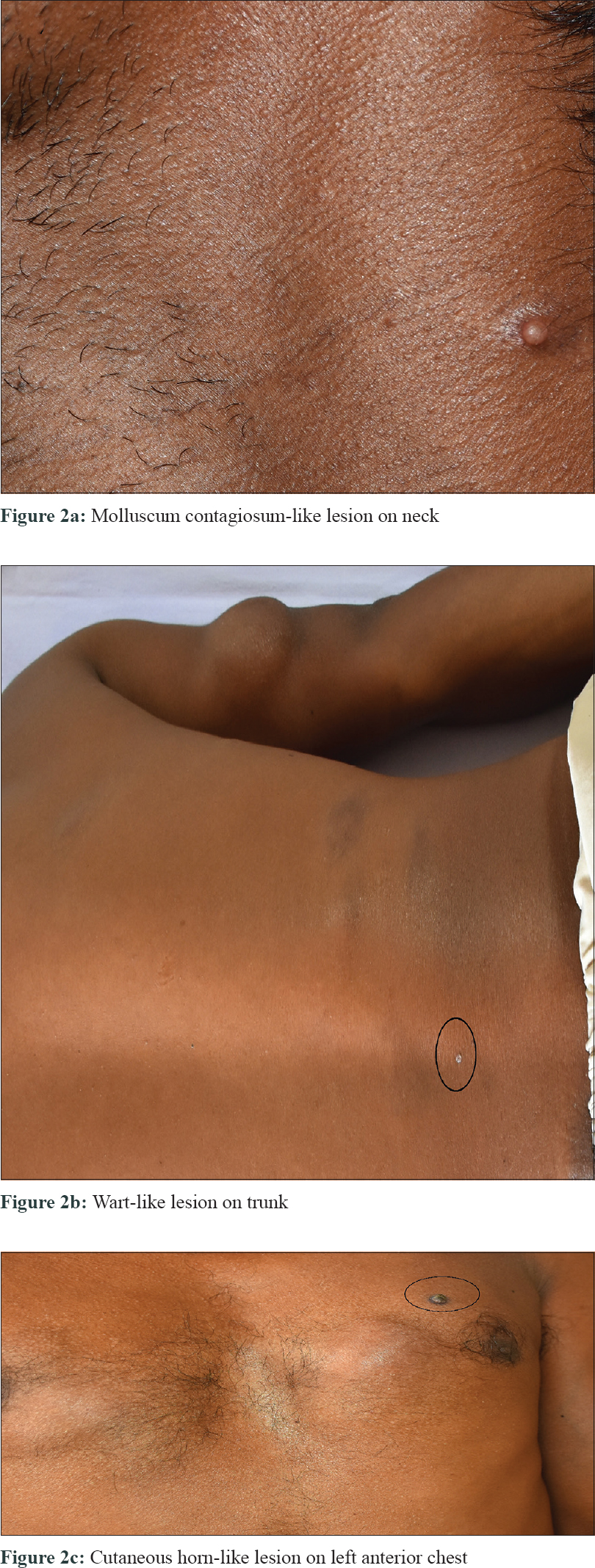 |
| Figure 2: |
Histopathological examination of the skin biopsy specimen taken from the swelling on both forearms, verrucous papule on trunk, papule on neck and subcutaneous plaque on left arm showed multiple sporangia containing endospores with mixed inflammatory cell infiltrate in the dermis.[Figure - 3]. X-ray and computed tomography scan of the chest did not show any involvement of the lung. Ultrasound abdomen revealed that the liver and the spleen were normal. The enzyme-linked immunosorbent assay test for human immunodeficiency virus I and II were non reactive. His routine hematological parameters were within normal limits. A final diagnosis of nasal rhinosporidiosis with cutaneous dissemination was made. The patient was referred to surgery for excision of larger swellings along with starting medical treatment with oral dapsone (100 mg/day). On follow-up, the patient was still developing new skin lesions, despite being on oral dapsone.
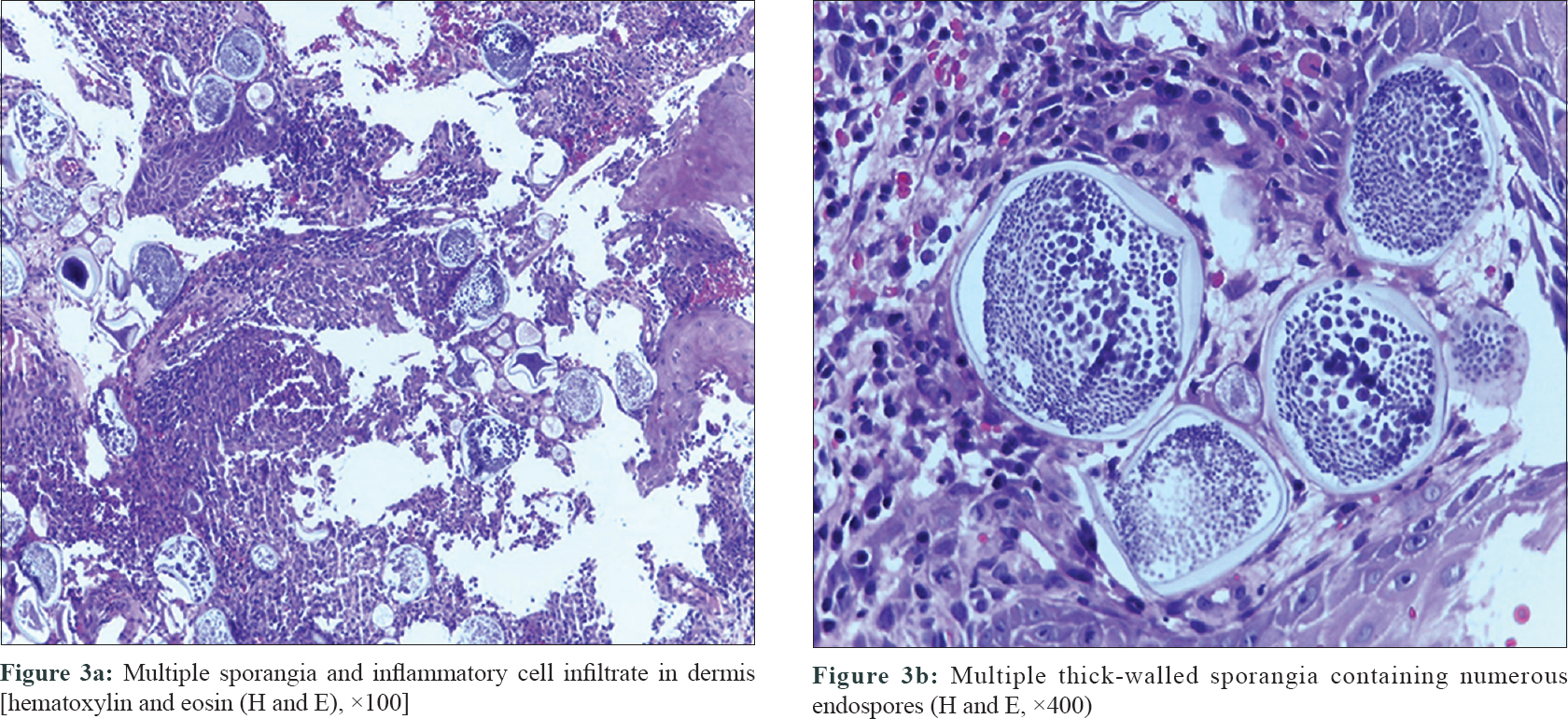 |
| Figure 3: |
Rhinosporidiosis can occur in four forms: nasal, ocular, cutaneous and disseminated (rare). The most common sites of infection are the nose and the nasopharynx, accounting for more than 75% of cases, followed by the 15% cases that develop lesion on the palpebral conjunctiva or associated structures such as the lacrimal apparatus.[3] Occasionally, rhinosporidiosis affects lips, palate, uvula, maxillary antrum, epiglottis, larynx, trachea, bronchus, ear, scalp, vulva, vagina, penis, rectum and skin.[4]
The presumed mode of infection is transepithelial, through traumatized nasal mucosa, from the natural aquatic habitat of R. seeberi. Common predisposing factors include trauma to the nasal mucous membrane, mostly during diving and swimming in the stagnant water or ponds.[5] In addition, impaired ciliary action, irritation and stagnation of secretions due to anatomic obstruction may also help in acquiring infection.[5] Cutaneous rhinosporidiosis has three modes of spread:(a)autoinoculation causing satellite lesions on the adjoining skin in nasal rhinosporidiosis; (b) hematogenous dissemination causing generalized cutaneous involvement with and/or without nasal involvement and (c) direct inoculation on the skin resulting in primary cutaneous rhinosporidiosis.[6]
Mucosal and cutaneous lesions commonly present as friable papillomas or pedunculated papules or plaques.[6] However, varied morphological presentations such as verrucous plaques, polypoidal growths, subcutaneous nodules, furunculoid lesions, ecthymatoid lesions, molluscum contagiosum, pyogenic granuloma, cutaneous horn and lipoma-like lesions have been reported in different individuals.[6],[7] Kumari et al. have reported a case of disseminated rhinosporidiosis presenting with different morphology of lesions at different body sites such as verrucous plaque, ulcerated tumor, granulomatous growth, furunculoid lesions and cutaneous horn along with nasal rhinosporidiosis.[6]
The differential diagnosis of cutaneous rhinosporidiosis depends on the morphology of lesion. The frequently considered differentials include lipoma, pyogenic granuloma, wart, tuberculous verrucosa cutis, liposarcoma and coccidioidomycosis. The diagnosis can be easily confirmed by performing a Giemsa-stain, imprint smear from the tissue sample from lesion or while doing fine-needle aspiration cytology.[6] However, histopathology is the gold standard for diagnosing rhinosporidiosis.[1] Characteristic findings in histology include sporangia of various sizes lined by well-defined wall, which can be seen in various stages of maturation(size varying from 10 to 200 μm). Endospores are seen inside the sporangia. Histopathologically, rhinosporidiosis should be differentiated from coccidioidomycosis. Coccidioidomycosis is an endemic disease in America with different clinical presentation and has smaller sporangia size (<60 μm in diameter) compared to rhinosporidiosis.[6] Our case had six different types of morphologies of cutaneous rhinosporidiosis, i.e., wart, pyogenic granuloma, lipoma, cutaneous horn, molluscum contagiosum and subcutaneous plaques with pigmentary change on surface; fitting into the diagnosis of disseminated cutaneous rhinosporidiosis. In addition, the present case had a new morphological variant, i.e. subcutaneous plaques with pigmentary change which has not been described in literature. Suspicion of cutaneous rhinosporidiosis was made based on the history of recurrent nasal rhinosporidiosis, habit of pond bathing and was confirmed by histopathology revealing multiple well-defined sporangia containing endospores.
Cutaneous rhinosporidiosis is best treated by surgical and diathermy excision. However, recurrence is common after excision.[8],[9] Several drugs such as dapsone, ketoconazole, ciprofloxacin and amphotericin B have been tried. Dapsone is quite effective and may arrest the maturation of sporangia and accelerate degenerative changes in them, but is not curative.[8],[9],[10] I n our case, the larger lipoma-like lesions were excised at various intervals and simultaneously dapsone 100 mg/day was started. However, despite medication, new lesions were appearing after 2 months.
We are reporting this case because of the polymorphic presentation with six morphologic variants of cutaneous rhinosporidiosis at different body sites, in an immunocompetent individual. In addition, the patient also had subcutaneous plaques with pigmentary change as a morphological variant of cutaneous rhinosporidiosis, which has not been described in literature to the best of our knowledge.
Declaration of patient consent
The authors certify that they have obtained all appropriate consent from patient, i.e. written consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Kaushal S, Mathur SR, Mallick SR, Ramam M. Disseminated cutaneous, laryngeal, nasopharyngeal, and recurrent obstructive nasal rhinosporidiosis in an immunocompetent adult: A case report and review of literature. Int J Dermatol 2011;50:340-2.
[Google Scholar]
|
| 2. |
Thappa DM, Venkatesan S, Sirka CS, Jaisankar TJ, Gopalkrishnan RC, Ratnakar C, et al. Disseminated cutaneous rhinosporidiosis. J Dermatol 1998;25:527-32.
[Google Scholar]
|
| 3. |
Prasad K, Veena S, Permi HS, Teerthanath S, Shetty KP, Shetty JP, et al. Disseminated cutaneous rhinosporidiosis. J Lab Physicians 2010;2:44-6.
[Google Scholar]
|
| 4. |
Lupi O, Tyring SK, McGinnis MR. Tropical dermatology: Fungal tropical diseases. J Am Acad Dermatol 2005;53:931-51, quiz 952-4.
[Google Scholar]
|
| 5. |
Snidvongs ML, Supanakorn S, Supiyaphun P. Severe epistaxis from rhinosporidiosis: A case report. J Med Assoc Thai 1998;81:555-8.
[Google Scholar]
|
| 6. |
Kumari R, Nath AK, Rajalakshmi R, Adityan B, Thappa DM. Disseminated cutaneous rhinosporidiosis: Varied morphological appearances on the skin. Indian J Dermatol Venereol Leprol 2009;75:68-71.
[Google Scholar]
|
| 7. |
Tolat SN, Gokhale NR, Belgaumkar VA, Pradhan SN, Birud NR. Disseminated cutaneous rhinosporidiomas in an immunocompetent male. Indian J Dermatol Venereol Leprol 2007;73:343-5.
[Google Scholar]
|
| 8. |
Shenoy MM, Girisha BS, Bhandari SK, Peter R. Cutaneous rhinosporidiosis. Indian J Dermatol Venereol Leprol 2007;73:179-81.
[Google Scholar]
|
| 9. |
Verma R, Vasudevan B, Pragasam V, Deb P, Langer V, Rajagopalan S, et al. Acase of disseminated cutaneous rhinosporidiosis presenting with multiple subcutaneous nodules and a warty growth. Indian J Dermatol Venereol Leprol 2012;78:520.
[Google Scholar]
|
| 10. |
Agirdir BV, Derin AT, Ozbilim G, Akman A. Cutaneous rhinosporidiosis presents with recurrent nasal philtrum mass in Southern Turkey. Int J Dermatol 2008;47:700-3.
[Google Scholar]
|
Fulltext Views
3,142
PDF downloads
1,337





