Translate this page into:
Post-lower segment cesarean section wound infection with Mycobacterium abscessus
Corresponding Author:
Jyotsna M Joshi
Department of Pulmonary Medicine, 2nd Floor, OPD Building, Topiwala National Medical College and BYL Nair Hospital, AL Nair Road, Mumbai Central, Mumbai - 400 008, Maharashtra
India
drjoshijm@gmail.com
| How to cite this article: Sasikumar C, Desai U, Joshi JM. Post-lower segment cesarean section wound infection with Mycobacterium abscessus. Indian J Dermatol Venereol Leprol 2017;83:349-350 |
Sir,
Nontuberculous mycobacteria exist widely in the environment. These organisms can cause pulmonary disease, skin and soft tissue infections and disseminated disease in humans.[1],[2],[3],[4],[5] Nontuberculous mycobacteria consist of photochromogens, scotochromogens, nonchromogens and rapid growers. Skin and soft-tissue infections contribute to the spectrum of hospital-acquired infections and rapidly growing nontuberculous mycobacteria are emerging as important causes of the surgical site infection outbreaks.[2]Mycobacterium abscessus is an acid-fast bacillus classified as pathogenic, rapidly-growing nontuberculous mycobacteria.[3]
A 30-year-old married woman visited our pulmonary medicine outpatient department, Topiwala National Medical College and BYL Nair Hospital, Mumbai with complaints of a non-healing lower segment cesarean section wound and repeated abscess formation at and above the incision line of the lower segment cesarean section scar for 3 months. The patient had initially an abscess within the non-healing lower segment cesarean section wound which developed into a sinus within 1 week of the surgery. Methicillin-sensitive Staphylococcus was grown in the bacterial culture of pus from the wound. She had received multiple courses of antibiotics; however, the abscess did not heal. She was treated empirically with antitubercular therapy by her treating physician for 2 weeks with no relief of symptoms. There was no history of any major medical or surgical illness in the past. The general examination was normal. On local examination, a gaping lower segment cesarean section scar of size 1 cm × 2 cm with sinus formation was seen along and above the lower segment cesarean section incision [Figure - 1]. There was no local rise of temperature, tenderness or regional lymphadenopathy. Systemic examination was normal. Blood tests revealed hemoglobin - 11 g/dl, leukocyte count - 6800 cells/cc mm, platelet count - 260,000 cells/cc mm and fasting blood sugar - 90 mg%. The liver and renal function tests were normal. The enzyme-linked immunosorbent assay for human immunodeficiency virus was nonreactive. Chest X-ray was normal. A local part ultrasound showed periwound edema and abscess formation extending to the skin and subcutaneous tissue. Mantoux test was negative. By the time she visited us, acid-fast bacilli culture of pus had grown nontuberculous mycobacteria and empirical antitubercular therapy was stopped. We reconfirmed nontuberculous mycobacterial culture isolation on two occasions. The smear was positive for acid-fast bacilli and the acid-fast bacilli culture showed growth of rapidly growing nontuberculous mycobacteria. Molecular line probe assay for species identification performed on the acid-fast bacilli culture isolate revealed Mycobacterium abscessus [Figure - 2]. The organism was susceptible to amikacin, clarithromycin and linezolid, whereas resistant to ciprofloxacin, cotrimoxazole, doxycycline, imipenem, minocycline and tobramycin on drug susceptibility tests. Subsequently, she was treated with oral clarithromycin 500 mg twice daily for 3 months and local care of the wound as per the American Thoracic Society guidelines for the management of nontuberculous mycobacteria infections. The wound started healing with minimal gaping and serous discharge. At the end of therapy, the wound had completely healed and the patient was asymptomatic on follow-up for 6 months [Figure - 3]. Outbreak could not be traced and investigated as the patient was referred at a later date. Hence, we could only postulate the possible source of infection.
 |
| Figure 1: Lower segment cesarean section wound pre-therapy |
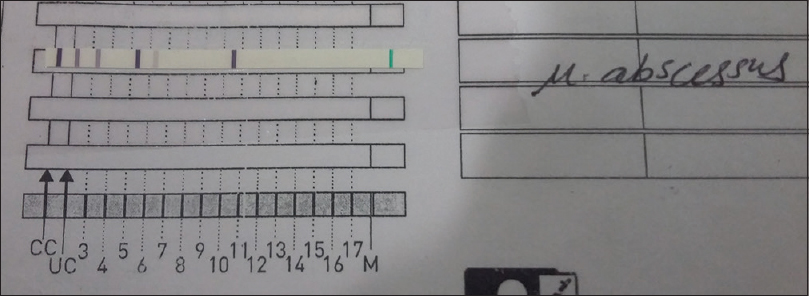 |
| Figure 2: Image of molecular line probe assay of Mycobacterium abscessus |
 |
| Figure 3: Lower segment cesarean section wound post-clarithromycin therapy |
Nontuberculous mycobacteria infections have emerged as an important cause of hospital-acquired surgical site infection causing great morbidity and mortality. It has been reported that skin and soft tissue infections are the second most common infectious complications following urinary tract infections after lower segment cesarean section with an infection rate of 6.3%–11.2%.[4] The nomenclature of rapidly growing nontuberculous mycobacteria has recently changed with the advent of biochemical techniques which allows species to be more accurately identified which in the past were simply identified as belonging to the “Mycobacterium fortuitum complex.” Now, utilizing deoxyribonucleic acid studies, four separate species have been identified as Mycobacterium fortuitum, Mycobacterium peregrinum, Mycobacterium chelonae and Mycobacterium abscessus. Among the rapidly growing nontuberculous mycobacteria species, Mycobacterium abscessus is known to be the major cause of skin infections. Mycobacterium abscessus is ubiquitous in the environment and was first described in 1953.[5]Mycobacterium abscessus causes nosocomial infection, postinjection abscess and wound infections following surgeries. Cutaneous infections with Mycobacterium abscessus manifest in the variety of ways including ulcerations, abscesses, draining sinuses or nodules and cause delayed healing. Laboratory cross-contamination, contaminated instruments or contaminated solutions cause inoculation of these organisms in the surgical wounds. Our patient might have acquired infection through the use of contaminated tap water for sterilization of surgical instruments. Several studies of surgical site infection with nontuberculous mycobacteria have been noted in literature. In their study, Kalita et al. report Mycobacterium fortuitum–Mycobacterium chelonae complex treated with clarithromycin as leading cause of delayed postoperative wound infections.[6] A Mycobacterium abscessus surgical site infection outbreak study by Tsao et al. documented a broad spectrum of clinical manifestations including dull abdominal pain, fever, swelling, indurated lesions, discharge and erythematous lesions in the poorly healed or nonhealed wounds which were treated with clarithromycin.[7] Nontuberculous mycobacteria have 40% positivity on Ziehl–Neelsen stain and 80% of the specimens yield acid-fast bacilli on culture. This indicates a possibility of missing a nontuberculous mycobacteria infection if only acid-fast bacilli smears are taken for diagnosis. Nontuberculous mycobacteria do not respond to antibiotics used for acute pyogenic infections. Species identification and subsequent drug susceptibility test form the cornerstones for prescribing appropriate therapy. Rapidly growing nontuberculous mycobacteria respond to antibiotics such as amikacin, quinolones, doxycycline and sulfamethoxazole. Clarithromycin, cefoxitin and imipenem are the commonly used drugs. Clarithromycin shows good efficacy against a broad range of atypical mycobacteria, but some organisms are resistant and proper sensitivities must be obtained. Extensive reviews suggest clarithromycin as the most common antibiotic of choice in Mycobacterium abscessus.[5],[6],[7] Clarithromycin, a semi-synthetic derivative of erythromycin, exerts its antibacterial action by binding to the 50s ribosomal subunit of susceptible bacteria and suppresses protein synthesis. Dosage is 7.5 mg/kg in children and 500 mg twice daily in adults. Common side effects of this drug are diarrhea, nausea, abnormal taste, dyspepsia, abdominal pain and headache. Rare side effects are liver function abnormalities, interstitial nephritis, transient hearing loss and QT prolongation.
The present case focuses on two important points. First, clinicians should be aware of the risk of nontuberculous mycobacterial infections in delayed or nonhealing wounds following any kind of surgery. Second, prompt diagnosis and initiation of drug susceptibility test guided antimicrobial therapy would reduce the relapse rate in such wound infections.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. | Johnson A, Young D, Reilly J. Caesarean section surgical site infection surveillance. J Hosp Infect 2006;64:30-5. [Google Scholar] |
| 2. | Ding LW, Lai CC, Lee LN, Hsueh PR. Disease caused by non-tuberculous mycobacteria in a university hospital in Taiwan, 1997-2003. Epidemiol Infect 2006;134:1060-7. [Google Scholar] |
| 3. | De Groote MA, Huitt G. Infections due to rapidly growing mycobacteria. Clin Infect Dis 2006;42:1756-63. [Google Scholar] |
| 4. | Lai CC, Tan CK, Chou CH, Hsu HL, Liao CH, Huang YT, et al. Increasing incidence of non-tuberculous mycobacteria, Taiwan, 2000-2008. Emerg Infect Dis 2010;16:294-6. [Google Scholar] |
| 5. | Liao CH, Lai CC, Ding LW, Hou SM, Chiu HC, Chang SC, et al. Skin and soft tissue infection caused by non-tuberculous mycobacteria. Int J Tuberc Lung Dis 2007;11:96-102. [Google Scholar] |
| 6. | Kalita JB, Rahman H, Baruah KC. Delayed post-operative wound infections due to non-tuberculous Mycobacterium. Indian J Med Res 2005;122:535-9. [Google Scholar] |
| 7. | Tsao SM, Liu KS, Liao HH, Huang TL, Shen GH, Tsao TC, et al. The clinical management of cesarean section-acquired Mycobacterium abscessus surgical site infections. J Infect Dev Ctries 2014;8:184-92. [Google Scholar] |
Fulltext Views
7,275
PDF downloads
2,551





