Translate this page into:
Pregnancy-associated vesicular prurigo pigmentosa: A rare entity
Corresponding author: Ass. Prof. Dr. Noha Mohammed Dawoud, Department of Dermatology, Venerology and STDs, Faculty of Medicine, Menoufia University, Shebine El-Kom, Egypt. dr_ndawoud@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Sagr RZ, Bin Mahfoz AM, Dawoud MM, Dawoud NM. Pregnancy-associated vesicular prurigo pigmentosa: A rare entity. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_1328_2023
Dear Editor,
Prurigo pigmentosa (PP) is an intensely pruritic skin eruption that leaves behind, reticulate hyperpigmentation.1,2 Interestingly, few reports of PP have been documented in pregnant women.2–4 Here, we report a case of PP in a 35-year-old Gravida 3, Para 2 pregnant woman from Saudi Arabia. She presented with an itchy skin rash, mainly on the chest and back at 12 weeks of gestational age. She suffered from recurrent vomiting and weight loss of about 10 kg. There were intact small vesicles on the erythematous base with areas of crusting over the sides of the neck [Figure 1a] and the anterior hairline [Figure 1b]. Multiple erythematous papules and crusted vesicles were seen on the anterior chest and in a V-shaped distribution on the posterior trunk admixed with reticulate post-inflammatory hyperpigmentation [Figure 2].

- Small vesicles on erythematous bases with areas of crustation over the sides of the neck.

- Small vesicles on erythematous bases with areas of crustation over the anterior hairline.

- Small vesicles on erythematous bases with areas of crustation admixed with reticulated post-inflammatory hyperpigmentation in the middle of the anterior chest.
Laboratory investigations were normal including total IgE levels and antinuclear antibodies. Urinary ketones were high at 15 mmol/L (+4).
Differential diagnoses included PP, pemphigoid gestationis, pemphigus foliaceous, dermatitis herpetiformis, varicella or confluent and reticulated papillomatosis.
Skin biopsy [Figure 3a–d] showed an intraepidermal bulla filled with mixed inflammatory infiltrate admixed with acantholytic epidermal cells. Perifollicular epidermis showed multiple abscesses, while the dermis showed perivascular and periadnex chronic inflammatory infiltrate. Periodic acid-Schiff (PAS) stain was negative and so was the direct immunofluorescence (DIF) of the perilesional skin.
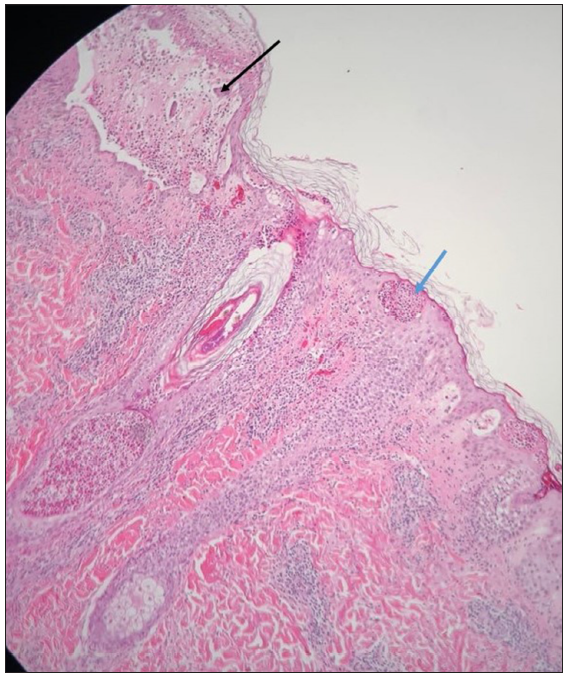
- Intraepidermal bulla (black arrow) filled with mixed inflammatory infiltrate admixed with acantholytic cells. Mild focal spongiosis and multiple abscesses (blue arrow) filled with mixed inflammatory cells (Haematoxylin and Eosin, 100x).
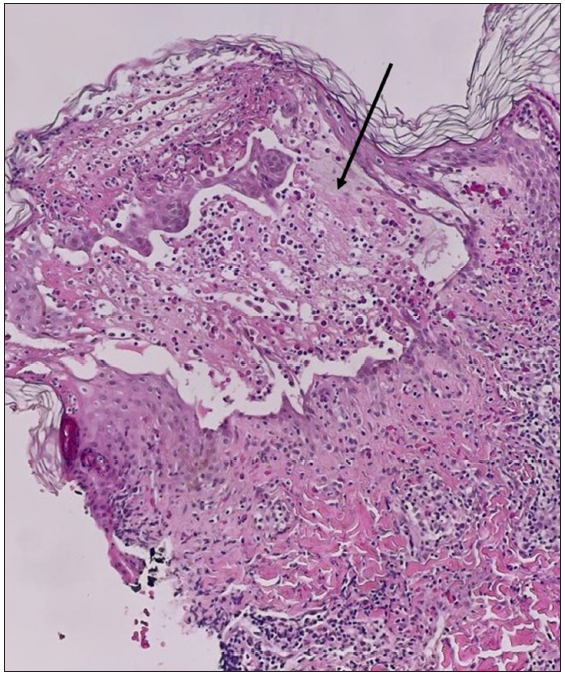
- Bulla (black arrow) closer view (Haematoxylin and eosin, 200x).

- Suppurative folliculitis with dermal perivascular and peri-adnexal chronic inflammatory infiltrate (Haematoxylin and Eosin, 100x).
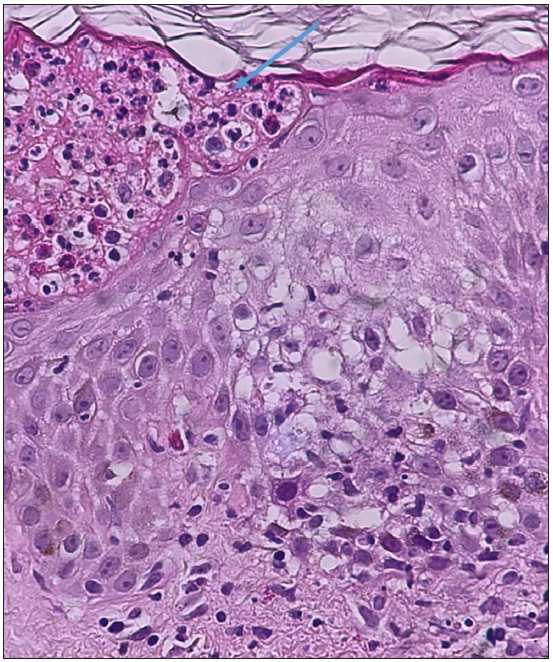
- Mild epidermal spongiosis and intraepidermal abscess (blue arrow) filled with neutrophils, eosinophils and lymphocytes (Haematoxylin and Eosin, 400x).
As a result of the presence of subcorneal pustule, pustular psoriasis, acute generalized exanthematous pustulosis (AGEP), subcorneal pustular dermatoses, dermatitis herpetiformis, pemphigus foliaceus, IgA pemphigus and infections were suspected. However, the evident reticulate hyperpigmentation and the presence of ketosis together with the absence of the other specific histopathological features of such diseases favoured the diagnosis of early-stage vesicular PP.
The patient was admitted to the hospital as a case of hyperemesis gravidarum to control vomiting and received intravenous fluids and antiemetic medications which reduced ketones in urine (+1) upon discharge. A topical soothing lotion was prescribed for the skin rash.
The skin rash subsided within 2 weeks following improvement of vomiting and ketosis and the patient was back to regular diet, leaving reticulate hyperpigmentation mainly on the trunk with no recurrence of the eruption during the 12-week follow-up period.
PP is underreported. However, it is now more common with trending habits for weight loss such as prolonged fasting, anorexia and ‘keto diet’. Ketosis as ketonuria or ketonaemia was reported in many studies to be a risk factor for the development of PP secondary to different metabolic aetiologies including diabetes mellitus, primary biliary cirrhosis, anorexia nervosa and post-bariatric surgeries due to decreased oral intake.1
Researchers have suggested that ketones might activate perivascular neutrophilic inflammation and induce the development of PP. Resolution of PP can be achieved with diet modification alone and the treatment of dehydration. Although the first-line therapy is oral minocycline or doxycycline which inhibits neutrophil chemotaxis and function, they are pregnancy category D drugs and may aggravate gastrointestinal upset. Other reported treatment options include dapsone, colchicine, macrolide antibiotics and systemic isotretinoin.5
There are a few reported cases of PP during pregnancy. In a systematic review done by Mufti et al., only five cases of PP have been reported during pregnancy.1 Two of them suffered from hyperemesis gravidarum and one followed a strict diet to avoid nausea and vomiting.2,4 Similar to our case, three patients presented in early pregnancy at about 12 weeks of gestation and had ketonuria. One patient’s skin rash and ketonuria improved only by rehydration and diet modification.1 So, our case seems to be the sixth reported case of pregnancy-associated PP worldwide and probably the first one from the Middle East.
Not only ketosis but also a possible hormonal role has been hypothesised as a worsening factor during pregnancy and menstruation. Thus, future research is needed to determine the exact pathogenesis of PP during pregnancy and the possible risk factors.6
Formation of vesicles or bullae in PP is very rare. Typical sites affected are the trunk and the neck. However, occurrences in atypical locations (e.g., face, scalp and the suprapubic region) have been described in only a few cases.7 In the present case, the presence of numerous itchy vesicular lesions on an erythematous base on the face and scalp, particularly along the anterior hairline and behind the ears, was a misleading presentation. It was confused with viral exanthema, especially varicella which is a serious diagnosis during early pregnancy.
The vesiculobullous lesions may result from marked spongiosis, liquefactive degeneration of the basal cell layer, papillary dermal oedema and extensive inflammation with intercellular and intracellular oedema.
Although rare, dermatologists should pay attention to the incidence of PP in association with hyperemesis gravidarum during early pregnancy. Fast and prompt control of ketosis is mandatory to improve and cure pregnancy-associated PP. Atypical presentation (vesicular) or atypical localization (face, neck and scalp) does not exclude PP.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Clinical manifestations and treatment outcomes in prurigo pigmentosa (Nagashima disease): A systematic review of the literature. JAAD Int. 2021;3:79-87.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Bullous prurigo pigmentosa in a pregnant woman with hyperemesis gravidarum. J Dermatol. 2015;42:436-7.
- [CrossRef] [PubMed] [Google Scholar]
- Prurigo pigmentosa in a pregnant woman. Int J Gynaecol Obstet. 2007;98:261-2.
- [CrossRef] [PubMed] [Google Scholar]
- Prurigo pigmentosa during pregnancy. Ann Dermatol Venereol. 2019;146:215-8.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical features and follow-up of prurigo pigmentosa: A case series. Cureus. 2022;29;14:e24600.
- [PubMed] [Google Scholar]
- Prurigo pigmentosa: A clinicopathologic study of 4 cases from the Middle East. Am J Dermatopathol. 2014;36:800.
- [CrossRef] [PubMed] [Google Scholar]
- Ketogenic diet-induced prurigo pigmentosa (the “keto rash”): A case report and literature review. J Clin Aesthet Dermatol. 2021;14:S29-S32.
- [PubMed] [PubMed Central] [Google Scholar]





