Translate this page into:
Prevalence of metabolic syndrome in patients with psoriasis
Correspondence Address:
Nuzhatun Nisa
Department of Dermatology, STD and Leprosy, S.M. H. S. Hospital, Srinagar, Jammu and Kashmir - 190 010
India
| How to cite this article: Nisa N, Qazi MA. Prevalence of metabolic syndrome in patients with psoriasis. Indian J Dermatol Venereol Leprol 2010;76:662-665 |
Abstract
Background: Psoriasis is a chronic inflammatory disease of the skin and is associated with an increased risk of cardiovascular atherosclerosis. Metabolic syndrome, a conglomerate of various clinical and biochemical parameters is a significant predictor of atherosclerotic disease and the associated risk for cardiovascular events in such patients. Aim: To investigate the prevalence of metabolic syndrome in patients with psoriasis. Methods: The study was a prospective, hospital based case-control study involving 150 adult patients with chronic plaque psoriasis and 150 healthy controls. Venous samples were taken at the enrolment visit after the subjects had fasted overnight (at least 8 h). Serum cholesterol and triglycerides were measured with enzymatic procedures. Plasma glucose was measured using a glucose oxidase method. Metabolic syndrome was diagnosed by the presence of three or more criteria of the National Cholesterol Education Programme's Adult Panel III (ATP III). Statistical analysis of the data was done using statistical processing software (SPSS-17) and epi-info software. Results: Metabolic syndrome was significantly more common in psoriatic patients than in controls 42(28%) vs 9(6%), odds ratio (OR) = 6.09, P<0.05. Psoriatic patients also had a significantly higher prevalence of hypertriglyceridaemia (73/150 among cases vs 24/150 among controls; P<0.05), arterial hypertension (74/150 among cases vs 24/150 among controls; P<0.05) and impaired fasting plasma glucose levels (27/150 among cases vs 04/150 among controls; P<0.05). Psoriatic patients with metabolic syndrome had mean disease duration of 13.67±11.87 years against 6.46±5.80 years in those without metabolic syndrome. Conclusion: There is a significantly higher prevalence of metabolic syndrome in psoriasis patients as compared to general population and so is the risk of having atherosclerotic adversity. While managing the psoriatic plaques of these patients, concerns should extend to the atherosclerotic plaques as well.Introduction
Psoriasis is a chronic inflammatory skin disease that affects 1-3% of the population. [1],[2] Epidemiological research has shown that hypertension, heart failure and diabetes are significantly more common in patients with psoriasis than in controls. [3] Moreover, an increased mortality from cardiovascular disease in patients with severe psoriasis has been documented and psoriasis may confer an independent risk of myocardial infarction especially in young patients. [4] Major factors that may contribute to this unfavorable cardiovascular risk profile include cigarette smoking, obesity, physical inactivity, hyperhomocysteinemia and psychological stress, which have a higher prevalence among patients with psoriasis. Obesity is associated with severe psoriasis and is reported about twice as frequently among psoriasis patients as in the general population. [3],[5] The association between psoriasis and metabolic syndrome is also true for mild severity psoriasis and is independent from the tendency of psoriatic patients to be obese. [5]
Methods
This study was conducted within a duration of eighteen months (January 2008 to June 2009), in the Department of Dermatology, STD and Leprosy, SMHS Hospital (associated teaching hospital of Government Medical College Srinagar, Jammu and Kashmir, India). The study was a hospital-based case-control study involving a series of 150 patients. Inclusion criteria for patients were age more than 18 years, disease duration of at least six months and not receiving any systemic treatment for psoriasis for at least one month before enrolment. The controls were patients with insignificant complaints, attendants of patients and staff members of the hospital. The source population for cases and controls was the same. An informed consent was taken from all patients and patient characteristics were recorded on a standard proforma. Statistical analysis of the data was done using statistical processing software (SPSS-17) and epi-info software.
Relevant data included age, gender, weight, height, body mass index, waist circumference, blood pressure, smoking habit, age of onset and duration of psoriasis, type and severity of psoriasis. Body mass index (BMI) was calculated as weight in kilograms/height 2 in meters. To determine waist circumference, we located the upper hip bone and placed the measuring tape at the level of the upper most part of the hip bone around the abdomen (ensuing the tape measure was horizontal). The tape measure was snug but did not cause compression on the skin. Blood pressure was recorded as the average of two measurements after subjects have been sitting for five minutes. Severity of psoriasis was assessed according to psoriasis area and severity index (PASI) and percent body surface area (%BSA) involvement. Chronic plaque psoriasis was considered to be localized or disseminated when it covered less or more than 10% of the BSA involvement. Metabolic syndrome was diagnosed by the presence of three or more of the five criteria of the National Cholesterol Education Programme′s Adult Panel III (ATP III): waist circumference > 102 cm in men or > 88 cm in women; hypertriglyceridaemia > 1.7 mmol/l (150mg/dl); high density lipoprotein (HDL) cholesterol < 1.0mmol/l (40mg/dl) in men or < 1.3mmol/dl (50mg/dl) in women; blood pressure > 130/85 mmHg; fasting plasma glucose of > 6.1 mmol/l (100mg/dl). [6] Venous samples were taken at the enrolment visit after the subjects had fasted overnight (at least 8 h). Serum cholesterol and triglycerides were measured with enzymatic procedures. Plasma glucose was measured using a glucose oxidase method. The study was approved by the institutional ethical committee.
Results
The study included 150 cases and 150 controls with descriptive chracteristics of each group given in [Table - 1]. Psoriasis area and severity index (PASI) score ranged from 2.3 to 70 (median PASI=13.05). Body surface area (BSA) involved ranged from 2% to 90%, with a median BSA involvement of 20. Ninety seven patients had involved BSA > 10% while fifty three had involved BSA < 10%. Disease duration in cases ranged from six months to thirty years with a mean disease duration of 6.67 years.

We found a higher prevalence of metabolic syndrome in cases (42/150= 28%) than in controls (09/150 = 6%) with an odds ratio (OR) of 6.09, P < 0.05 after adjusting for confounding by age. Individual components of metabolic syndrome like hypertriglyceredaemia, impaired fasting plasma glucose and hypertension were also more prevalent in cases than in controls. The prevalence of various components of metabolic syndrome in cases and controls along with odds ratio and P value are given in [Table - 2].

Comparing psoriatic patients with and without metabolic syndrome, we observed that patients with metabolic syndrome had longer mean disease duration than psoriatic patients without metabolic syndrome as in [Table - 3]. There was no difference regarding psoriasis severity, gender or prevalence of smoking.
In all age groups we observed higher prevalence of metabolic syndrome among cases than controls. We also observed an early onset of metabolic syndrome in patients of psoriasis [Figure - 1].

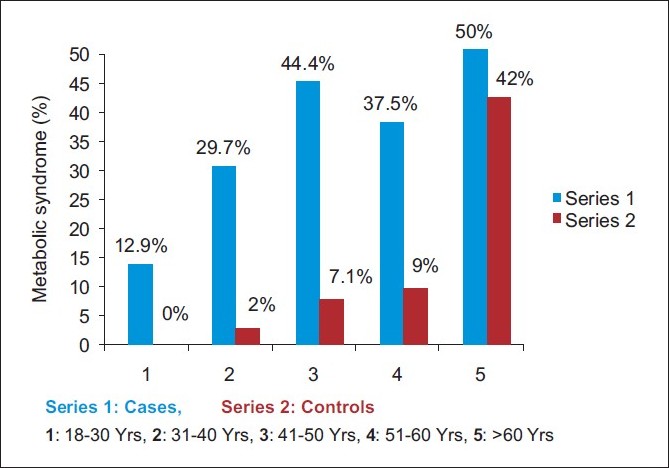 |
| Figure 1 :Comparing prevelance of metabolic syndrome among different age groups of cases and controls |
Discussion
The hypothesis that the atherosclerotic and the psoriatic plaques are the two offshoots of same root is a focus of current research. The following few recent advances in the understanding of atherosclerosis, psoriasis and metabolic syndrome beget the consideration of exploring a common etiopathogenetic pathway for the diseases.
- Atherosclerosis represents an ongoing low-grade systemic inflammatory state. [7]
- Psoriasis represents a systemic inflammatory disease. [8]
- Psoriatic patients have higher prevalence of metabolic syndrome. [5],[9]
- Psoriasis confers an independent risk for adverse cardiovascular events. [10]
Although the exact etiopathogenetic link is yet to be elucidated, certain proinflammatory cytokines and immunological mediators which are shared by the pathognetic mechanisms of the two diseases have been identified. Proinflammatory cytokines like TNF-a and IL-6, which are over expressed in psoriasis plaques, are known to contribute to features of the metabolic syndrome, such as hypertension, dyslipidaemia and insulin resistance. [11] Similar to psoriasis, the metabolic syndrome is characterized by an increase in the immunological activity of type 1 helper T cells (T H 1). [12]
Many studies have been published on psoriasis vis-ΰ-vis metabolic syndrome or individual components of metabolic syndrome. Our study observed a higher prevalence of metabolic syndrome among psoriatic patients than the controls [28% vs 6%, odds ratio (OR) 6.09, P = <0.05] which is similar to the results of a well designed, good volume, cross-sectional study by Gisondi et al.[5] [30.1% vs 20.6%, OR 1.65, P=0.005]. Further more, Sommer et al.[13] also found higher prevalence of metabolic syndrome among hospitalized psoriatic patients as compared to hospitalized melanoma patients but the study instead of ATP III criteria adopts a modified version of the WHO definition of metabolic syndrome. In comparison to studies of Gisondi et al.[5] and Sommer et al.[13] our study has the drawback of being controlled for confounding via adjustment for age only, instead of age and gender. But the effect of such confounding should be little keeping in view of the fact that in a data which is adjusted for confounding by age, the low prevalence of metabolic syndrome in premenopausal women as compared to males is balanced by its relatively higher prevalence in post menopausal women.
In contrast to Gisondi et al.[5] study which documented the higher prevalence of metabolic syndrome in psoriatic patients than controls after the age of 40 years, [5] we observed the higher prevalence in psoriatic patients right from the late second decade (12.9% vs 0% in the age group 18 - 30 years), [Figure - 1]. We also observed longer mean disease duration in psoriatic patients with metabolic syndrome than those without metabolic syndrome. It is possible that depression, eating habits, psychosocial inactivity, stress and inflammatory mediators associated with psoriasis favor metabolic syndrome. Such an association also suggests that psoriatic patients without metabolic syndrome need to be counseled properly so that behavioral modification in association with appropriate management of their psoriasis may make the emergence of cardiovascular risk factors less likely.
Association of psoriasis with individual components of metabolic syndrome had been a focus of many cross-sectional studies in the recent past. Results from such studies are varied and inconsistent with regard to dyslipidemia. Several studies with varying population and analytical approaches have found an association between psoriasis and increased prevalence of diagnosis of dyslipidemia. [14],[15],[16] In addition, multiple studies have documented increased prevalence of diabetes and hypertension in patients with psoriasis. [13],[17],[18]
Niemann et al.[9] used the General Practice Research Database and found higher rates of diabetes mellitus, hypertension, hyperlipidaemia, obesity and smoking in patients with psoriasis than in controls. [9] The same authors also found that patients with severe psoriasis had higher rates of obesity and diabetes mellitus than those with mild psoriasis. Our study also showed a higher prevalence of metabolic syndrome in psoriatic patients. We also observed the higher prevalence of individual components of metabolic syndrome like triglyceride levels >150 mg/dl (73/150 vs 24/150 OR= 4.98, P=0.0005), fasting plasma glucose > 100 mg/dl (27/150 vs 08/150 OR=3.90, p =0.0006) and blood pressure >130/85 (74/150 vs 24/150 OR=5.11, P=0.0005) in patients of psoriasis than in controls, [Table - 1]. Such an association prompts one at looking upon atherosclerotic and psoriatic plaques as related closely to each other but the conclusion awaits establishment of a common or at least closely related etiopathogenetic mechanism. Studies on such an association, till now, point toward the primary role of insulin resistance for both metabolic syndrome and chronic inflammatory state of the body. Therapeutic intervention based on methotrexate and tumor necrosis factor (TNF)-a antagonists seem to diminish the insulin resistance state. An atherogenic lipid profile at the onset of psoriasis has been observed in a well-designed study, which excluded the possible role of confounding factors such as obesity, hypertension, cigarette smoking and physical activity. [10]
| 1. |
Schon MP, Boehncke WH. Psoriasis. N Engl J Med 2005;352:1899-912.
[Google Scholar]
|
| 2. |
Gelfand JM, Weinstein R, Porter SB, Neimann AL, Berlin JA, Margolis DJ. Prevelance and treatment of psoriasis in the United Kingdom: A population-based study. Arch Dermatol 2005;141:1537-41.
[Google Scholar]
|
| 3. |
Henseler T, Christophers E. Disease concomitance in psoriasis. J Am Acad Dermatol 1995;32:982-6.
[Google Scholar]
|
| 4. |
Gelfand JM, Neimann AN, Shin DB, Wang X, Margolis DJ, Troxel AB. Risk of myocardial infarction in patients with psoriasis. JAMA 2006;296:1735-41.
[Google Scholar]
|
| 5. |
Gisondi P, Tessari G, Conti S, Piaserico S, Schianchi S, Peserico A, et al. Prevalence of metabolic syndrome in patients with psoriasis: A hospital - based case - control study. Br J Dermatol 2007;157:68-73.
[Google Scholar]
|
| 6. |
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Ecke RH, Franklin BA, et al. Diagnosis and Management of the Metabolic Syndrome. Circulation 2005;112:2735-52.
[Google Scholar]
|
| 7. |
Ross R. Atherosclerosis: an inflammatory disease. N Engl J Med 1999;340:115-26.
[Google Scholar]
|
| 8. |
Rocha-Pereira P, Santos-Silva A, Rebelo I, Figueiredo A. The inflammatory response in mild and in severe psoriasis. Br J Dermatol 2004;150:917-28.
[Google Scholar]
|
| 9. |
Neimann AL, Shin DB, Wang X, Margolis DJ, Troxel AB, Gelfand JM. Prevalence of cardiovascular risk factors in patients with psoriasis. J Am Acad Dermatol 2006;55:829-35.
[Google Scholar]
|
| 10. |
Mallbris L, Granath F, Hamsten A, Stahle M. Psoriasis is associated with lipid abnormalities at the onset of skin disease. J Am Acad Dermatol 2006;54:614-21.
[Google Scholar]
|
| 11. |
Sterry W, Strober BE, Menter A. Obesity in psoriasis: The metabolic, clinical and therapeutic implications. Report of an interdisciplinary conference and review. Br J Dermatol 2007;157:649-55.
[Google Scholar]
|
| 12. |
Wysocki J, Skoczynski S, Strozik A, Hochul B, Zygula M. Metabolic or immunometabolic syndrome? Wiad Lek 2005;58:124-7.
[Google Scholar]
|
| 13. |
Sommer DM, Jenisch S, Suchan M, Christophers E, Weichental M. Increased prevalence of metabolic syndrome in patients with moderate to severe psoriasis. Arch Dermatol Res 2006;298:321-8.
[Google Scholar]
|
| 14. |
Cohen AD, Sherf M, Vidavsky L, Vardy DA, Shapiro J, Meyerovitch J. Association between psoriasis and the metabolic syndrome. Dermatol 2008;216:152-5.
[Google Scholar]
|
| 15. |
Akhyani M, Ahsani AH, Robati RM, Robati AM. The lipid profile in psoriasis: A controlled study. J Eur Acad Dermatol Venereol 2007;21:1330-2.
[Google Scholar]
|
| 16. |
Solak TN, Tekin IO, Barut F, Sipahi EY. Accumulation of oxidized low density lipoprotein in psoriatic skin and changes of plasma lipid levels in psoriatic patients. Mediators Inflam 2007;2007:1-5.
[Google Scholar]
|
| 17. |
Cohen AD, Gilutz H, Henkin Y, Zahger D, Shapiro J, Donneh DY, et al. Psoriasis and the metabolic syndrome. Acta Dermatol Venereol 2007;87:506-9.
[Google Scholar]
|
| 18. |
Shapiro J, Cohen AD, David M, Hodak E, Chodik G, Viner A. The association between psoriasis, diabetes mellitus and atherosclerosis in Israel: A case control study. J Am Acad Dermatol 2007;56:629-34.
[Google Scholar]
|
Fulltext Views
6,663
PDF downloads
2,483





