Translate this page into:
Primary cutaneous amyloidosis of auricular concha
Correspondence Address:
Xin Zhou
Guangzhou Institute of Dermatology, Guangzhou, Guangdong
China
| How to cite this article: Zhou X, Chen Q, Tian X. Primary cutaneous amyloidosis of auricular concha. Indian J Dermatol Venereol Leprol 2020;86:230 |
Sir,
Primary cutaneous amyloidosis of the auricular concha is a rare disease, characterized by yellow, flesh-colored, waxy or pearly papules and plaques in the auricular concha. We report a case of a 50-year-old female patient with primary cutaneous amyloidosis of the auricular concha and describe the dermatoscopic findings. This case represents the first dermatoscopic description of primary cutaneous amyloidosis of the auricular concha.
A 50-year-old female presented with a history of more than 1 year duration of asymptomatic, flesh-colored papules on both ears and a 3-year history of pruritic, light-brown macules on the upper back and extensor surfaces of the extremities. The patient was otherwise systemically well. Dermatological examination revealed multiple, flesh-colored, dome-shaped papules with a waxy surface, 1–3 mm in diameter, located on the auricular conchae bilaterally [Figure - 1]a. In addition, symmetrical dusky-brown macules were found on her upper back and extensor surfaces of the extremities [Figure - 1]b.
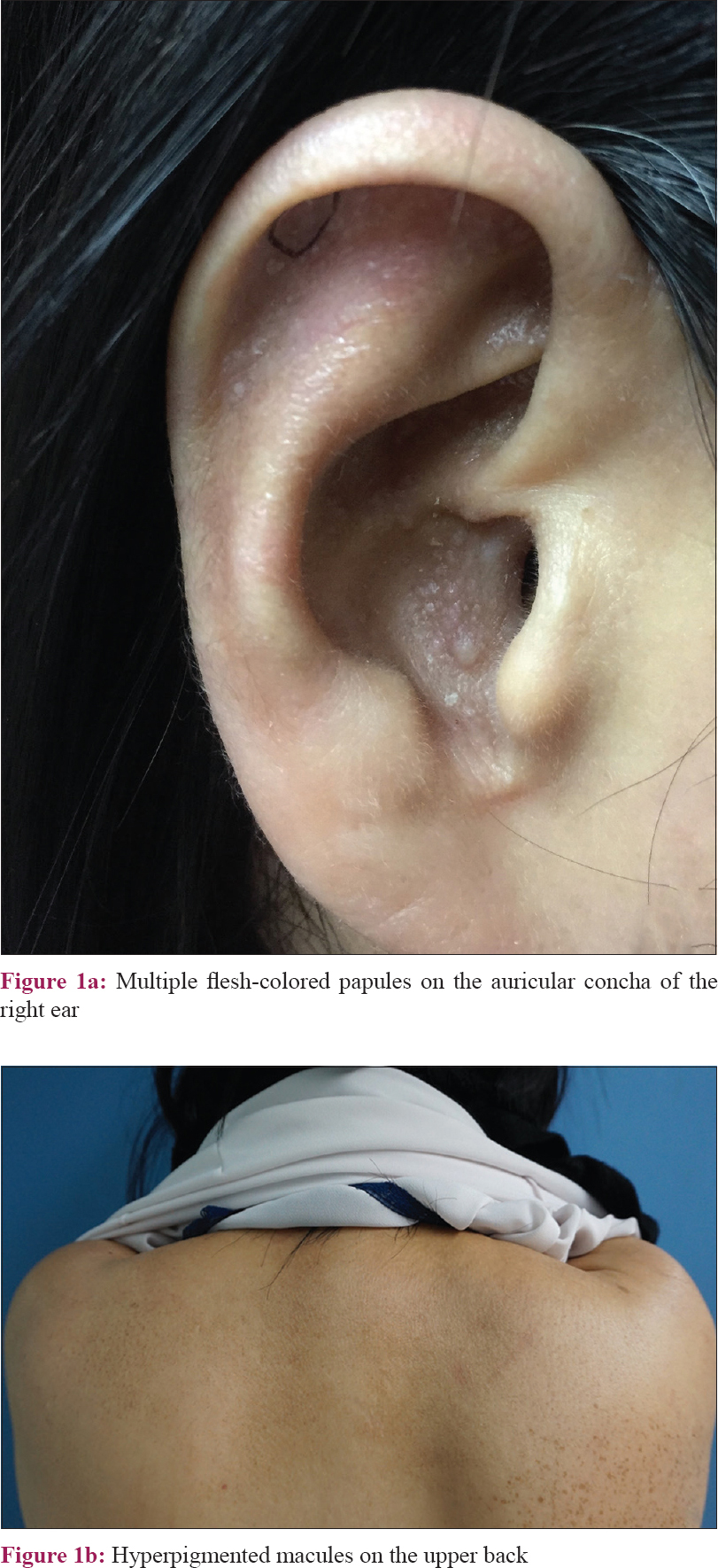 |
| Figure 1: |
There were no abnormal laboratory findings suggestive of systemic disease. The patient denied any significant medical, surgical, or family history.
On polarized light dermatoscopic [Figure - 2]; ×10; DermLite DL3N, 3Gen, Long Island, New York, USA] examination, multiple, white globular structures of variable sizes were seen on a background of a light brown and pink network. Some cysts aggregated into a cobblestone pattern.
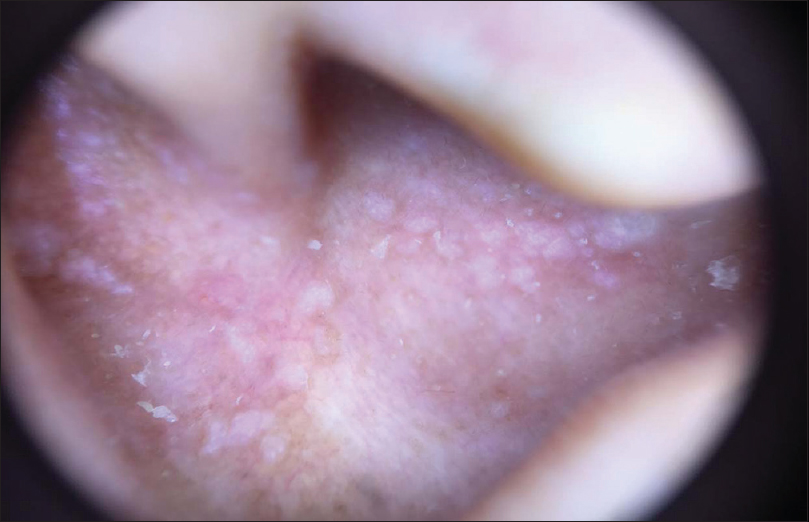 |
| Figure 2: Dermatoscopic findings revealed white globules on a background of a delicate network (×10) |
A biopsy specimen was taken from one of the lesions on the ear; histological examination revealed hyperkeratosis, elongation of the rete ridges, pigment incontinence, and eosinophilic amorphous deposits in the widened dermal papillae [Figure - 3]. The material was positive for crystal violet and Congo red staining. Immunohistochemical staining of the deposits was CK34βE12-positive.
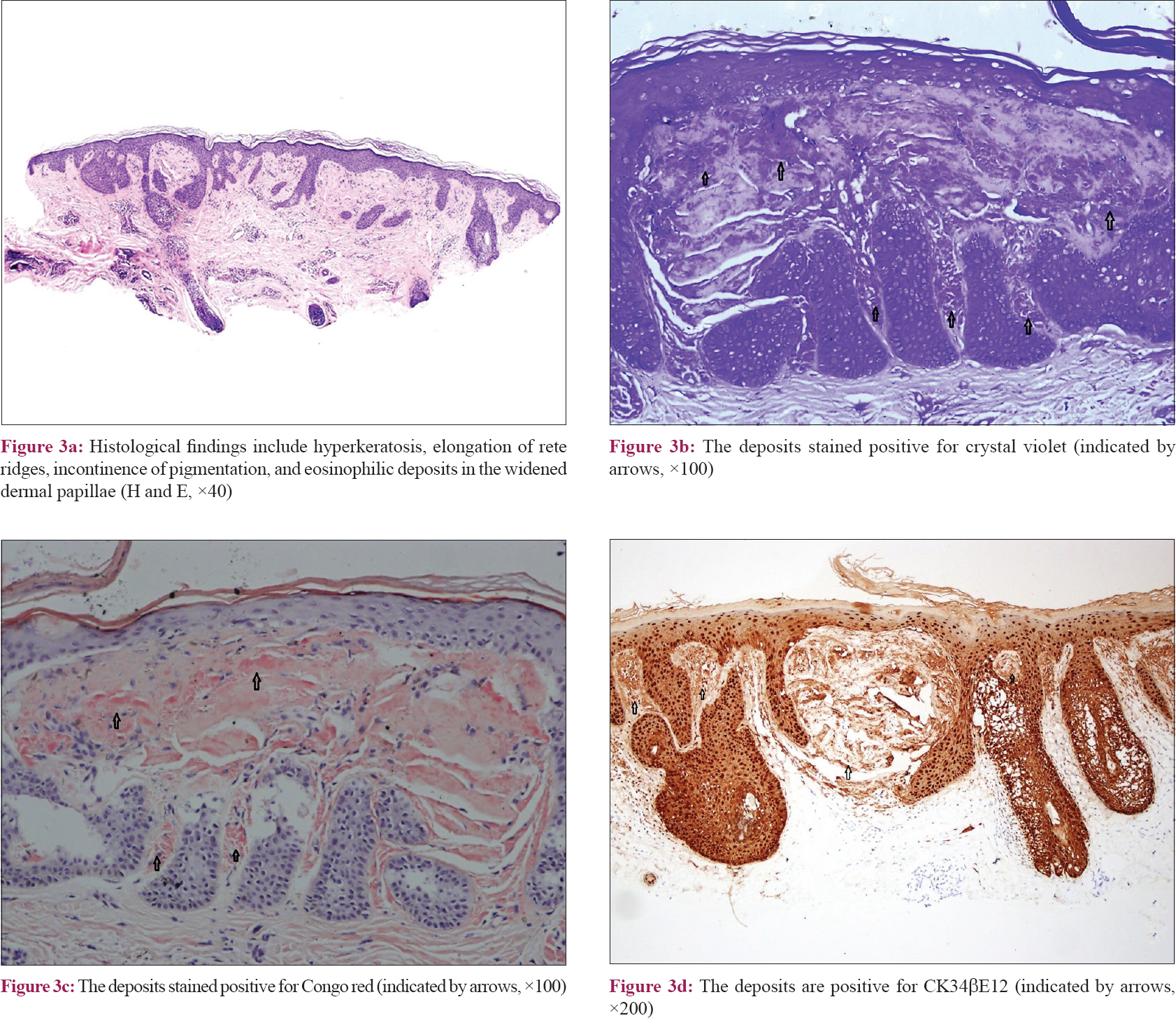 |
| Figure 3: |
Primary cutaneous amyloidosis of the auricular concha is a rare disease that was first described in 1988 by Hicks et al.[1] Clinically, it presents as small papular lesions on the external ear, including the auricular concha and external auditory canal with unilateral or bilateral involvement. The lesions may be yellow or flesh-colored or waxy or pearly papules and plaques. In contrast to classical lichen amyloidosus, it usually lacks pruritus. It is unrelated to systemic amyloidosis. The pathological findings include hyperkeratosis and homogeneous eosinophilic deposits within widened dermal papillae. These materials stained positively with crystal violet and Congo red, and they also reacted strongly on immunohistochemistry with CK34βE12 antibody, which suggests that the amyloid material has an epidermal origin. Patients with primary cutaneous amyloidosis of the auricular concha often have a good prognosis and can be treated by surgical resection.
Lichen amyloidosus and macular amyloidosis are two major forms of primary localized cutaneous amyloidosis. They are likely the result of focal epidermal damage, but the exact relationship between them is unknown. Coexistence of lichen and macular amyloidosis in the same patient is termed “biphasic amyloidosis.” There are currently only four case reports of the biphasic form of amyloidosis, whose lichenoid counterpart consists of papules on the external ear.[2],[3],[4] Involvement of the auricular concha in biphasic amyloidosis further supports the point that lichen amyloidosus and macular amyloidosis are clinical variants of the same process.
The dermatoscopic findings of this case showed multiple, white, globule-like structures of variable sizes on a background of a light-brown and pink network. Some cysts aggregated into a cobblestone pattern. We suggest that the globule-like structures and cobblestone pattern are due to amyloid deposits in the widened dermal papillae. This structure is consistent with the “central hub,” which was mentioned by Chuang et al.[5] Hyperpigmentation is less prominent in this form of primary cutaneous amyloidosis. This report is the first description of the dermatoscopic features of primary cutaneous amyloidosis of the auricular concha. More studies are essential to establish the definite dermatoscopic patterns.
The patient denied any surgical treatment and was given a follow-up examination.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Open subject of Key Laboratory of Dermatology Department of Education (201702042).
Science and Technology Program of Guangzhou, China (201804010058).
Conflicts of interest
There are no conflicts of interest.
| 1. |
Hicks BC, Weber PJ, Hashimoto K, Ito K, Koreman DM. Primary cutaneous amyloidosis of the auricular concha. J Am Acad Dermatol 1988;18:19-25.
[Google Scholar]
|
| 2. |
Bakos L, Weissbluth ML, Pires AK, Müller LF. Primary amyloidosis of the concha. J Am Acad Dermatol 1989;20:524-5.
[Google Scholar]
|
| 3. |
Barnadas MA, Pérez M, Esquius J, Curell R, de Moragas JM. Papules in the auricular concha: Lichen amyloidosus in a case of biphasic amyloidosis. Dermatologica 1990;181:149-51.
[Google Scholar]
|
| 4. |
Errol C. Lichen amyloidosis of the auricular concha: Report of two cases and review of the literature. Dermatol Online J 2006;12:1.
[Google Scholar]
|
| 5. |
Chuang YY, Lee DD, Lin CS, Chang YJ, Tanaka M, Chang YT, et al. Characteristic dermoscopic features of primary cutaneous amyloidosis: A study of 35 cases. Br J Dermatol 2012;167:548-54.
[Google Scholar]
|
Fulltext Views
3,852
PDF downloads
3,959





