Translate this page into:
Primary cutaneous aspergillosis caused by Aspergillus terreus in an immunocompetent woman
Corresponding authors: Dr. Fangfang Bao & Dr. Qing Yang Department of Microbiology, Hospital for Skin Diseases, Department of Dermatology, Shandong First Medical University, Shandong Provincial Institute of Dermatology and Venereology, Shandong Academy of Medical Sciences. baofangfang2008@163.com & yangqing79@126.com
-
Received: ,
Accepted: ,
How to cite this article: Jiao Y, Li H, Zhang Y, Sun L, Chen S, Yang Q, et al. Primary cutaneous aspergillosis caused by Aspergillus terreus in an immunocompetent woman. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_1178_2024
Dear Editor,
Aspergillosis is primarily reported in immunocompromised individuals. Primary cutaneous aspergillosis (PCA) caused by Aspergillus flavus and Aspergillus fumigatus is quite common. Cutaneous Aspergillus terreus infections secondary to systemic aspergillosis caused by Aspergillus terreus are also familiar. A case of PCA caused by Aspergillus terreus characterised by a thick crust on a finger was diagnosed based on histopathology, mycology, culture, and gene sequencing in an immunocompetent woman. It was successfully treated with oral itraconazole and topical terbinafine.
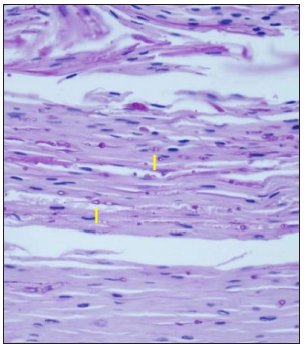
A 64-year-old woman presented with a thick yellow crust on the dorsum of the right index finger for two months, accompanied by occasional mild itching [Figure 1]. The patient stated that there was a red patch on the affected area over the past 2 years and denied any bleeding or preceding trauma. Topical medications were applied on this patch but gave no relief. She had a history of diabetes but was well-controlled with medication for years.

- Primary cutaneous aspergillosis on the dorsum of the right index finger as the thick yellow crust.
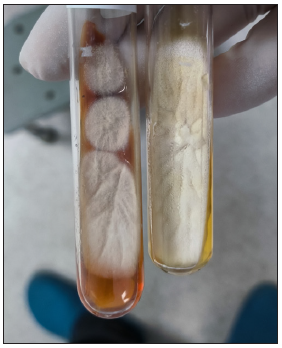
Histopathological examination revealed epidermal hyperkeratosis, parakeratosis, acanthosis, and localised acantholysis with a small infiltration of eosinophils and neutrophils and active proliferation of basal cells. In the upper dermis, bands of infiltrating lymphocytes, plasma cells, and a small number of eosinophils were observed, along with collagen fibre hyperplasia and small blood vessel proliferation. Periodic acid-Schiff (PAS) staining and fungal fluorescence microscopy revealed hyphae and spores in the stratum corneum, while acid-fast staining was negative [Figure 2a].
- Hyphae and spores in the stratum corneum, indicated by the yellow arrows (Periodic acid-Schiff staining, 400x)
Fungal microscopy was positive. The biopsy sample was cultured twice, yielding Aspergillus colonies without any growth of mycobacteria [Figure 2b, 2c]. We extracted the partial internal transcribed spacer (ITS) region of the rRNA for gene sequencing and uploaded the result on the national centre for biotechnology information (NCBI) for alignment. It showed 99% homology with Aspergillus terreus sequences. Considering its colony morphology and microscopic features, the isolate was confirmed as Aspergillus terreus. Drug susceptibility test (DST) performed using the broth microdilution method, Thermo Scientific™ Sensititre™ YeastOne™ (SYO), demonstrated resistance to anidulafungin, micafungin, caspofungin, voriconazole, fluconazole, and amphotericin B, while showing sensitivity to itraconazole, 5-fluorocytosine, and posaconazole.
- Culture of Aspergillus terreus- cinnamon-brown colonies with velvety texture on Sabouraud dextrose agar
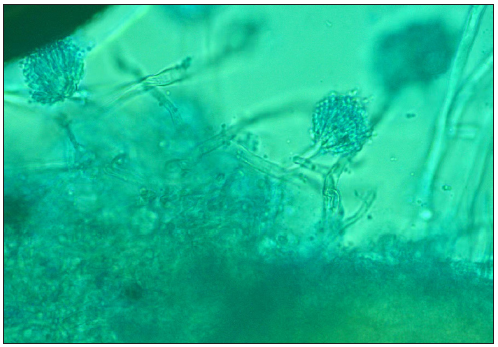
- Fluorescent staining of the culture: conidiophores ending in a vesicle covered by phialides bearing conidia (400x).
Routine hematological and biochemical evaluations revealed no abnormal findings. Given the localised lesion and laboratory findings, a diagnosis of PCA was established. The patient was treated with oral itraconazole (200 mg twice daily) for 4 weeks along with topical 1% terbinafine ointment. The lesion showed improvement after 4 weeks of treatment [Figure 3] and completely resolved after 3 months.
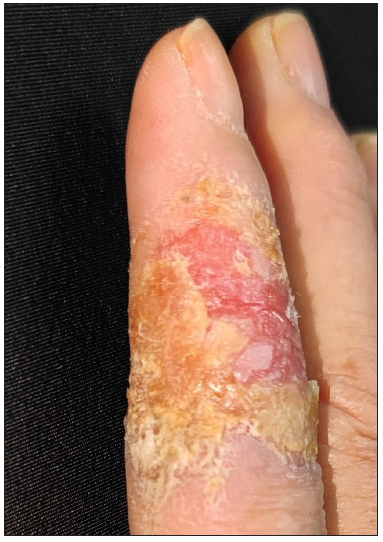
- The lesion showing improvement after 4 weeks of treatment.
Cutaneous aspergillosis can be categorised into PCA and secondary cutaneous aspergillosis (SCA). The most frequently reported PCA pathogens and their morbidity rates are Aspergillus fumigatus (42.3%), Aspergillus flavus (35.1%), and Aspergillus niger (10.8%).1 Aspergillus flavus appears to be more common in PCA, whereas Aspergillus fumigatus is more frequently associated with SCA.2,3 PCA is usually diagnosed in immunocompetent individuals as well as immunocompromised individuals with conditions such as haematologic malignancy, HIV/AIDS, solid organ transplantation, corticosteroid use, stem cell transplantation, diabetes mellitus, and trauma.1,4 The clinical presentation of PCA is diverse; lesions usually begin as erythematous, fluctuant nodules and pustules that gradually evolve into crust-covered ulcers.5 SCA often presents as multiple fulminant maculopapular lesions, typically due to direct or haematogenous spread from an infectious source.2
Diagnosis of PCA relies on multiple methods. Histopathological examination using PAS staining is based on the identification of septate hyphae branching dichotomously at acute angles, which invade the skin. This helps exclude environmental contamination and confirms pathogenicity. However, species identification is challenging based solely on histopathology. Therefore, culture is essential for determining the aetiological agent, given that morphological characteristics vary among different Aspergillus species. Gene sequencing further aids in confirming the diagnosis. Since Aspergillus is ubiquitous in nature, it is necessary to take primary specimens for repeated cultures to avoid misdiagnosis.
Currently, there are no standard guidelines available for the treatment of PCA. Antifungal therapy combined with surgical debridement may show a lower rate of mortality (13.8%) compared with monotherapy with antifungals (34.6%) or surgery(31.3%).1 Recurrence rates, dissemination rates, and mortality associated with PCA are reported to be 10.8%, 18.5%, and 31.5% respectively. Diabetes patients tend to have an even higher rate of recurrence (66.7%). However, PCA in immunocompetent individuals generally has a favourable prognosis.1 For Aspergillus terreus, it may be sensitive to itraconazole, voriconazole, posaconazole, isavuconazole, caspofungin, anidulafungin and micafungin, but shows reduced susceptibility to amphotericin B.6 As an increasing problem in aspergillosis, voriconazole resistance was mostly described in the isolates of Aspergillus fumigatus, Aspergillus flavus, and cross-resistance between itraconazole, posaconazole, and voriconazole was frequently observed.7
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Shandong Provincial Natural Science Foundation (ZR2024MH192), Shandong Provincial Medical and Health Science and Technology Development Plan (202004120466), Jinan Science and Technology Program (Clinical Medical Science and Technology Innovation Program, 202134012) and Taishan Scholar Special Foundation of Shandong Province (tsqn202211345)
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Factors affecting patient outcome in primary cutaneous aspergillosis. Medicine (Baltimore). 2016;95:e3747.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Cutaneous aspergillosis. J Clin Microbiol. 1998;36:3115-21.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Cutaneous invasive aspergillosis: Retrospective multicenter study of the French invasive-aspergillosis registry and literature review. Medicine. 2015;94:e1018.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Invasive aspergillosis by aspergillus flavus: Epidemiology, diagnosis, antifungal resistance, and management. J Fungi (Basel). 2019;5:55.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Primary cutaneous aspergillosis: Our experience in 10 years. J Infect. 1998;37:24-7.
- [CrossRef] [PubMed] [Google Scholar]
- Species identification and in vitro antifungal susceptibility of aspergillus terreus species complex clinical isolates from a French multicenter study. Antimicrob Agents Chemother. 2018;62:e02315-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Acquired antifungal drug resistance in aspergillus fumigatus: Epidemiology and detection. Med Mycol. 2011;49:S90-5.
- [CrossRef] [PubMed] [Google Scholar]





