Translate this page into:
Primary cutaneous extranodal natural killer/T-cell lymphoma
Correspondence Address:
Vijaya Basavaraj
Professor of Pathology, JSS Medical College, Shivarathreeshwar Nagar, Mysore, Karnataka
India
| How to cite this article: Basavaraj V, Kumararadhya R, S, Vimala M. Primary cutaneous extranodal natural killer/T-cell lymphoma . Indian J Dermatol Venereol Leprol 2014;80:562-564 |
Sir,
Extranodal natural killer/T-cell (ENK/T) lymphoma is a rare neoplasm, subcategorized into T-nasal and T-nasal type lymphomas. A T-nasal type lymphoma with the initial presentation in the skin is known as a primary cutaneous extranodal natural killer/T-nasal type lymphoma.
A 32-year-old male presented with multiple erythematous patches, plaques and ulcers over the left thigh, right inguinal region and left forearm for a month. On examination, multiple large ulcers were noted [Figure - 1]. The ulcers were indurated and the floor showed granulation tissue and slough in a few of them. A few erythematous plaques were seen over the abdomen. The differential diagnoses of neutrophilic dermatosis, cutaneous lymphoma and pyoderma gangrenosum were considered. He was admitted to the hospital for evaluation. In the course of hospitalization, the patient developed difficulty in swallowing and burning sensation in the throat. The patient was a smoker since 6 years. His general physical examination revealed normal vital signs. Left inguinal lymph nodes were enlarged. Indirect laryngoscopy revealed oedematous and congested epiglottis and slough over right arytenoids. A skin biopsy was done and sent for histopathological examination.
 |
| Figure 1: Large, irregular ulcerative lesion |
Routine haematological examination revealed counts within normal limits with peripheral blood smear showing normocytic normochromic blood picture with neutrophilia and eosinophilia. Ultrasonographic examination of the abdomen revealed mild splenomegaly, hepatomegaly and mild ascites. ELISA for HIV and HBSAg and the VDRL test were non-reactive. Radiological examination showed a soft tissue swelling in the supraglottic region. Fine-needle aspiration cytology of the inguinal lymph nodes showed features of reactive lymphadenitis. Bone marrow examination was not performed. Histopathological examination of the skin biopsy showed focal ulceration of the epidermis. The dermis showed marked edema and infiltration by atypical lymphoid cells having scant cytoplasm, a large nucleus with irregular nuclear membrane and coarse chromatin. There was perivascular accentuation of the infiltrate. A few blood vessels showed fibrinoid degeneration and angiolysis. Nuclear dust and necrosis were seen. There were a few plasma cells and neutrophils amidst the neoplastic lymphocytic infiltrate [Figure - 2]. No epidermotropism was noted. The features were suggestive of cutaneous lymphoma possibly extranodal NK/T-cell lymphoma. The tissue paraffin block was sent to a higher centre for immunohistochemical analysis which revealed positive staining of the tumour cells for CD56 and CD2 and negative staining for surface CD3 [Figure - 3].
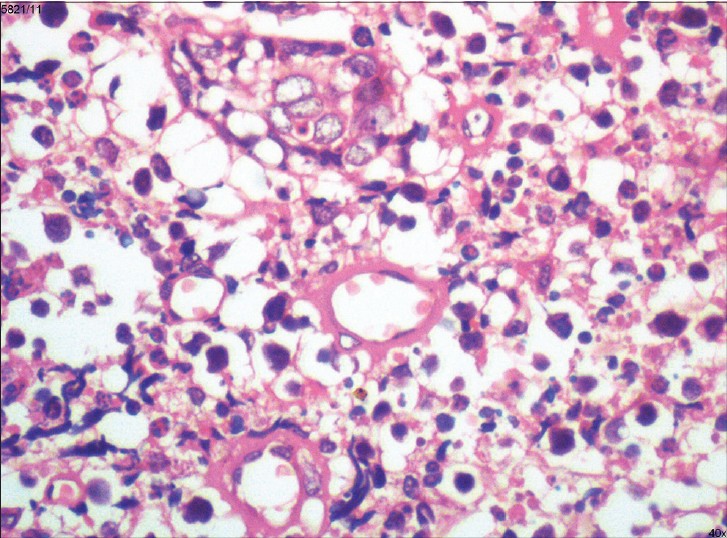 |
| Figure 2: Angiocentric disposition of tumour cells with presence of a few neutrophils and eosinophils. (H and E, ×400) |
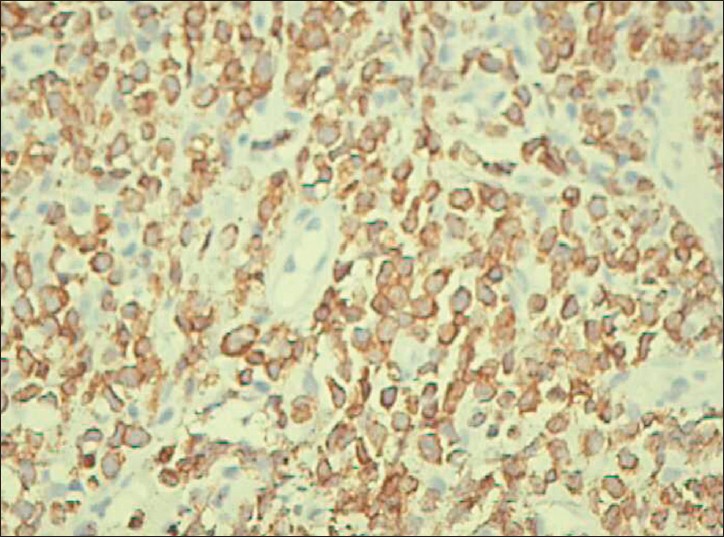 |
| Figure 3: Membrane positivity of CD56 in the tumor cells (DAB, ×400) |
In the interim, flexible laryngoscopy was performed which showed edema of left arytenoids, left aryepiglottic folds and minimal slough over arytenoids. A biopsy from the left arytenoid showed diffuse infiltration by large lymphoid cells with hyperchromatic nuclei in the subepithelial region. Keeping in mind both the skin and laryngeal biopsies, a final diagnosis of extranodal primary cutaneous NK/T-cell lymphoma with laryngeal dissemination was made.
NK/T-cell lymphomas show significant variations in incidence in different geographical regions and racial populations with a higher incidence in Asians. [1] Cutaneous lesions show morphologic heterogeneity with varied manifestations namely, multiple erythematous nodules, erythematous to violaceous well-demarcated plaques and nodules, ulcero-necrotic lesions with bulla formation, poorly circumscribed erythematous patches and multiple large ulcers as in the present case. [2],[3]
Histopathologically, these tumours show atypical lymphoid cells characteristically showing angiocentric infiltration. Necrosis is a conspicuous feature. Admixed plasma cells and neutrophils which are usually a constant feature may sometimes mask the diagnosis. The careful recognition of atypical lymphoid cells, their angiocentric disposition and presence of conspicuous necrosis should raise the suspicion of NK/T-cell lymphoma. The expression of cytotoxic molecules in the lymphoid cells may predispose to apoptosis by tumour cells and normal bystander cells. The mainstay in confirming the diagnosis is the immunohistochemical features of the tumour cells. The common immunophenotype is CD2 + , CD56 + , surface CD3− , cytoplasmic CD3∈ + , cytotoxic granules associated proteins and EBV-encoded RNA (EBER)-EBV + . [4] In the present case, the neoplastic cells were positive for CD56, CD2 and negative for surface CD3. However, analysis for EBV and cytoplasmic CD3 were not performed.
Extranodal NK/T-cell lymphoma carries a poor prognosis. Distant dissemination occuring early in the clinical course of the disease has been well documented. [5] When disease is disseminated to the aerodigestive tract as in our case, the prognosis is considered still poorer
| 1. |
Au WY, Ma SY, Chim CS, Choy C, Loong F, Lie AK, et al. Clinicopathologic features and treatment outcome of mature T-cell and natural killer-cell lymphomas diagnosed according to the World Health Organization classification scheme: A single center experience of 10 years. Ann Oncol 2005;16:206-14
[Google Scholar]
|
| 2. |
Seishima M, Yuge M, Kosugi H, Nagasaka T. Extranodal NK/T-cell Lymphoma, Nasal Type, Possibly Arising from Chronic Epstein-Barr Virus Infection. Acta Derm Venerol 2010;90:102-3.
[Google Scholar]
|
| 3. |
Pincus LB, Zehnder JL, Neuhaus IM, Andreadis C, McCalmont TH. Presentation of extranodal natural killer T-Cell lymphoma, nasal type, with poorly circumscribed erythematous patches J Clin Oncol 2010;28:e94-5.
[Google Scholar]
|
| 4. |
Schwartz EJ, Molina-Kirsch H, Zhao S, Marinelli RJ, Warnke RA, Natkunam Y. Immunohistochemical Characterization of Nasal-Type Extranodal NK/T-Cell lymphoma using a tissue microarray. Am J Clin Pathol 2008;130:343-51.
[Google Scholar]
|
| 5. |
Gill H, Liang RH, Tse E. Extranodal natural-killer/t-cell lymphoma, nasal type. Adv Hematol 2010;2010:627401.
[Google Scholar]
|
Fulltext Views
1,832
PDF downloads
1,273





