Translate this page into:
Primary cutaneous extranodal natural killer/T-cell lymphoma presenting as bilateral erythematous patches on the arms
Correspondence Address:
Woo Jin Lee
Department of Dermatology, Asan Medical Center, University of Ulsan College of Medicine, 88 Olympic-ro 43-gil, Songpa-gu, Seoul 05505
Republic of Korea
| How to cite this article: Moon IJ, Kang HJ, Lee MW, Lee WJ. Primary cutaneous extranodal natural killer/T-cell lymphoma presenting as bilateral erythematous patches on the arms. Indian J Dermatol Venereol Leprol 2017;83:453-456 |
Abstract
Natural killer/T-cell lymphoma is a rare, Epstein–Barr virus-associated type of cytotoxic lymphoma thatpresents mainly in the nasal cavity and its vicinity. Very few cases of primary cutaneous extranodal natural killer/T-cell lymphoma have been reported till date. All the previously reported cases of primary cutaneous extranodalnatural killer/T-cell lymphoma presented as lesions resembling cellulitis, subcutaneous nodules or ulcers. We report a rare case which presented as erythematous and purpuric round patches on the arms and was finally diagnosed as primary cutaneous extranodalnatural killer/T-cell lymphoma, following a skin biopsy. The atypical patchy lesions presented a diagnostic challenge. We herein describe this clinically novel atypical patch-like presentation of primary cutaneous extranodalnatural killer/T-cell lymphoma together with the key histopathologic features and highlights of the previously reported cases.Introduction
Extranodal natural killer/T-cell lymphoma is a rare type of cytotoxic lymphoma which is known to be associated with Epstein–Barr virus infection and is more common in East Asia than in Western populations.[1] Extranodal natural killer/T-cell lymphoma is subcategorized into two distinct subtypes: “Nasal” and “nasal-type.” The former mainly presents as locally destructive tumors in the nasal cavity, maxillary sinuses or palate.[2] The latter affects extranodal sites such as the gastrointestinal tract, lung or skin without involvement of the nasal cavity. Very few cases of extranodal natural killer/T-cell lymphoma affecting the skin as the primary site have been reported so far, most of which presented as lesions resembling cellulitis, plaque or ulcer.[3],[4],[5] We report an extremely rare case of primary cutaneous extranodal natural killer/T-cell lymphoma, that presented as erythematous to purpuric patches on both the arms, together with its histopathological findings and a concise review of the literature.
Case Report
A 47-year-old man was referred to the department of dermatology with multiple erythematous macules and patches of varying sizes on both arms. At that time, he was an in-patient in the hospital, undergoing evaluation for relapsing fever accompanied by pancytopenia of unknown cause since 3 months. Initial blood tests revealed leukopenia (1600/μL), thrombocytopenia (7000/μL) and low hemoglobin (8.2 g/dL). A bone marrow biopsy revealed hemophagocytosis and a presumptive clinical diagnosis of hemophagocytic lymphohistiocytosis was made, but anti-nuclear antibody-negative systemic lupus erythematosus was also considered as the patient suffered from chronic arthritis of the hands and feet. While being investigated for the etiology of his deteriorating medical condition, multiple erythematous macules of sudden onset were observed on his right [Figure - 1] and left [Figure - 2] forearm. The skin lesions were asymptomatic. Topical mometasone was prescribed with a clinical suspicion of nummular eczema and applied for a couple of weeks with little success. Thus, a skin biopsy was performed on his left forearm. The histopathological examination revealed infiltration of small- to medium-sized lymphoid cells along the dermoepidermal junction and around the blood vessels. Vasculopathy with extravasation of red blood cells and fibrinoid change of blood vessels were also noted [Figure - 3] and [Figure - 4]. Immunohistochemical staining with markers including CD2, cytoplasmic CD3, CD4, CD8 (CD4:CD8 ratio being approximately 3:1), CD56 [Figure - 5], Epstein–Barr virus in situ hybridization [Figure - 6] and T-cell intercellular antigen showed positive results, whereas immunophenotyping for CD20 was negative. Put together, the histopathological and immunohistochemical findings were suggestive of natural killer/T-cell lymphoma. A computed tomographic scan from the head to abdomen revealed no hepatosplenomegaly, enlarged lymph nodes or visceral infiltration of lymphoma. Following the final diagnosis of primary cutaneous extranodal natural killer/T-cell lymphoma, systemic corticosteroids were initiated. However, the patient expired within 2 weeks of the diagnosis, owing to persistent pancytopenia accompanied by intracranial hemorrhage.
 |
| Figure 1: Multiple erythematous and purpuric patches on the right forearm |
 |
| Figure 2: A well-defined, round, purpuric patch on the left forearm |
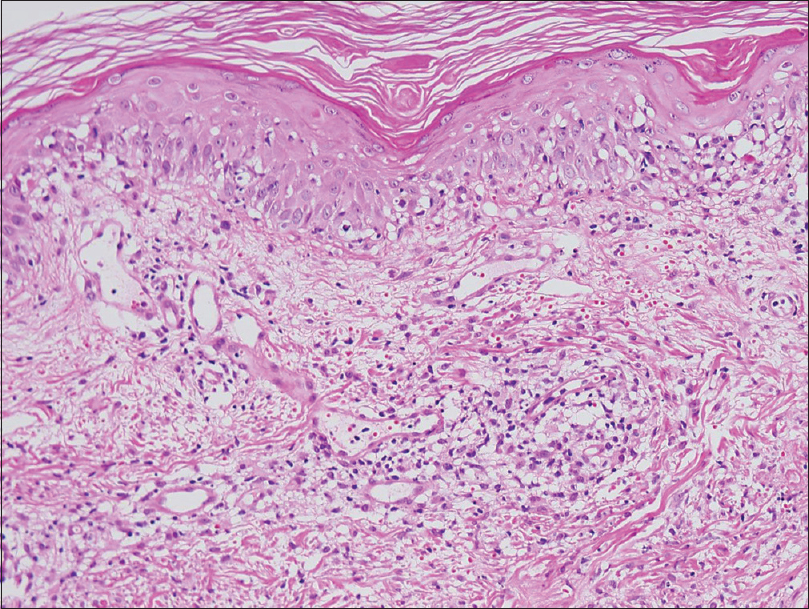 |
| Figure 3: Superficial to deep dermal infiltration of lymphoid cells resembling interface dermatitis (H and E, ×100) |
 |
| Figure 4: Perivascular infiltration of small to medium-sized, atypical lymphoid cells in the dermis (H and E, ×200) |
 |
| Figure 5: The lymphoid cells show positive immunohistochemical staining with CD56 (×200) |
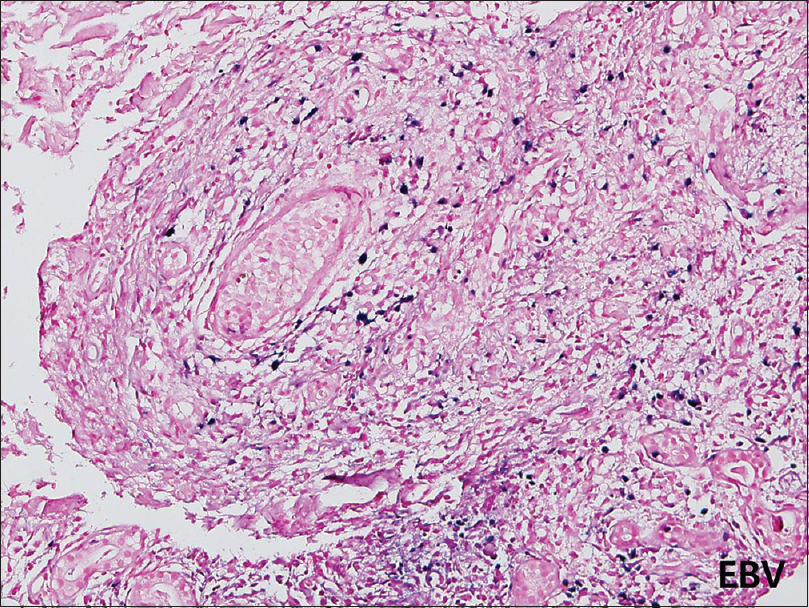 |
| Figure 6: Positive immunohistochemical staining with Epstein–Barr virus insitu hybridization support the diagnosis of primary cutaneous extranodal natural killer/T-cell lymphoma (×200) |
Discussion
Extranodal natural killer/T-cell lymphoma may present either primarily in extra-nasal sites or as disseminated disease secondary to nasal involvement. Among primary extra-nasal sites, the skin is the second most common site of involvement of extranodal natural killer/T-cell lymphoma, following the upper aerodigestive tract.[6] However, the incidence of primary cutaneous extranodal natural killer/T-cell lymphoma is known to be extremely rare. In most cases of primary cutaneous extranodal natural killer/T-cell lymphoma reported in the literature, the morphology of the skin lesions were cellulitis-like or abscess-like lesions, subcutaneous nodules, ulcerations or generalized rashes.[7] Thus, multiple erythematous patches are a novel clinical presentation of primary cutaneous extranodal natural killer/T-cell lymphoma. Yet, it is possible that the lesions were in their early phase and probably evolving into a different morphology such as nodules or plaques, a fact which we were not able to confirm due to the death of the patient soon after the diagnosis.
Recently, we have reported the histopathological characteristics of extranodal natural killer/T-cell lymphoma according to the lesional morphology.[5] As the aforementioned study mainly dealt with secondary cutaneous lesions in patients with already documented extranodal natural killer/T-cell lymphoma, the diagnosis of cutaneous extranodal natural killer/T-cell lymphoma was not difficult. On the other hand, besides the atypical patch-like morphology of the lesion, the diagnosis of primary cutaneous extranodal natural killer/T-cell lymphoma in the patient described in this case was challenging because he had no documented malignancy that could provide a clinical clue. Histopathological features of our case, such as superficial to deep perivascular infiltration of small- to medium-sized lymphoid cells with vasculopathy, matched those of erythematous to purpuric patch-like lesions described in the aforementioned study. Interestingly, our case did not exhibit an angiodestructive pattern which is a typical finding in extranodal natural killer/T-cell lymphoma. The rather benign clinical appearance of the disease in our case may be attributed to this absence of aggressive destruction of dermal vessels, subsequent extravasation of blood cells and resulting edema. However, to define the common characteristic histopathological features of primary cutaneous patch-like extranodal natural killer/T-cell lymphoma lesions, additional investigations are necessary.
Like other types of cutaneous lymphoma, immunohistochemical studies are often essential to establish the diagnosis of cutaneous extranodal natural killer/T-cell lymphoma. Typical tumor cells of cutaneous extranodal natural killer/T-cell lymphoma show positive immunophenotypes with CD2, cytoplasmic CD3 and CD56 and strong positivity for Epstein–Barr virus insitu hybridization.[8] Of note, our case showed positivity for both CD4 and CD8 which is a relatively infrequent immunohistochemical profile of extranodalnatural killer/T-cell lymphoma.[9] Overall, early recognition of this condition and timely confirmation of the diagnosis are of golden value in the treatment of this uncommon disease with a poor prognosis.[10]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Ko YH, Kim CW, Park CS, Jang HK, Lee SS, Kim SH, et al. REAL classification of malignant lymphomas in the Republic of Korea: Incidence of recently recognized entities and changes in clinicopathologic features. Cancer 1998;83:806-12.
[Google Scholar]
|
| 2. |
Sabattini E, Bacci F, Sagramoso C, Pileri SA. WHO classification of tumours of haematopoietic and lymphoid tissues in 2008: An overview. Pathologica 2010;102:83-7.
[Google Scholar]
|
| 3. |
Kim HJ, Kim SH, Oh SH. CD56-negative extranodal NK/T-Cell lymphoma, nasal type, with extranasal cutaneous involvement. Ann Dermatol 2015;27:618-20.
[Google Scholar]
|
| 4. |
Kim SH, Seon HJ, Choi YD, Yun SJ. Clinico-radiologic findings in primary cutaneous extranodal natural killer/T-cell lymphoma, nasal type mimicking cellulitis of the left arm. Iran J Radiol 2015;12:e12597.
[Google Scholar]
|
| 5. |
Lee WJ, Lee MH, Won CH, Chang SE, Choi JH, Moon KC, et al. Comparative histopathologic analysis of cutaneous extranodal natural killer/T-cell lymphomas according to their clinical morphology. J CutanPathol 2016;43:324-33.
[Google Scholar]
|
| 6. |
Lim ST, Hee SW, Quek R, Lim LC, Yap SP, Loong EL, et al. Comparative analysis of extra-nodal NK/T-cell lymphoma and peripheral T-cell lymphoma: Significant differences in clinical characteristics and prognosis. Eur J Haematol 2008;80:55-60.
[Google Scholar]
|
| 7. |
Lee WJ, Lee YJ, Won CH, Chang SE, Choi JH, Lee MW. The applicability and prognostic value of the TNM classification system for primary cutaneous lymphomas other than mycosis fungoides and Sézary syndrome in primary cutaneous NK/T-cell lymphoma patients. J Am AcadDermatol 2015;73:172-4.e1.
[Google Scholar]
|
| 8. |
Jaffe ES, Chan JK, Su IJ, Frizzera G, Mori S, Feller AC, et al. Report of the workshop on nasal and related extranodalangiocentric T/natural killer cell lymphomas. Definitions, differential diagnosis, and epidemiology. Am J SurgPathol 1996;20:103-11.
[Google Scholar]
|
| 9. |
Ng SB, Lai KW, Murugaya S, Lee KM, Loong SL, Fook-Chong S, et al. Nasal-type extranodal natural killer/T-cell lymphomas: Aclinicopathologic and genotypic study of 42 cases in Singapore. Mod Pathol 2004;17:1097-107.
[Google Scholar]
|
| 10. |
Huang H, Lin Z, Lin X, Cai Q, Xia Z, Jiang W. Long-term outcomes of patients with newly diagnosed extranodal natural killer/T-cell lymphoma treated by etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin regimen: A single-institution experience. Leuk Lymphoma 2011;52:1041-8.
[Google Scholar]
|
Fulltext Views
5,849
PDF downloads
2,020





