Translate this page into:
Primary melanoma in rare locations: Clinical and dermatoscopic features
2 Department of Oncology, Lower Silesian Oncology Center, Wroclaw, Poland
3 Dermato-Oncology Unit, The Center for Cancer Prevention and Treatment, Katowice; Department of Conventional and Intraoperative Radiotherapy, Maria Sk?odowska-Curie Memorial Cancer Center and Institute of Oncology Gliwice Branch, Gliwice, Poland
4 Department of Dermatology, Preventive Medicine and Pathology, Rutgers New Jersey Medical School, Rutgers University, Newark, New Jersey, USA
5 Department of Dermatology, Sexually Transmitted Diseases and Immunodermatology, Ludwik Rydygier Medical College in Bydgoszcz, Nicolaus Copernicus University, Torun, Poland
Correspondence Address:
Grazyna Kaminska-Winciorek
Dermato-Oncology Unit, The Center for Cancer Prevention and Treatment, 16 Fliegera Street, 40-060 Katowice
Poland
| How to cite this article: Kaminska-Winciorek G, Calik J, Wydmanski J, Schwartz RA, Czajkowski R. Primary melanoma in rare locations: Clinical and dermatoscopic features. Indian J Dermatol Venereol Leprol 2014;80:369-371 |
Sir,
We present two histopathologically proven cases of melanoma in rare locations, documented both clinically and by means of dermatoscopy. Dermatoscopy was performed with the use of a standard, non-polarized hand-held dermatoscope (Dermatoscope Delta 20; Heine, Herrsching, Germany; Handyscope Fotofinder Systems) and videodermatoscope (Medicam 500 Fotofinder Dermoscope).
Case 1
A 41-year-old male farmer and long-time smoker had a mucosal melanoma on the upper lip and palate. Its onset was evident as a brownish macule on the upper lip. It spread rapidly approximately one year prior to evaluation after which a small, pinkish nodule appeared, growing over the next 2 months. The brownish macules enlarged rapidly and extended on to parts of the upper lip, vermillion and palate, as well as the buccal mucosa. The nodule located on the central part of the upper lip was excised and biopsy confirmed the presence of an ulcerated melanoma (Breslow 4.4 mm). Further evaluation with chest X-ray, sonogram of the abdomen and basic biochemical parameters revealed no abnormalities. Later, the melanoma also spread to the skin of the upper part of the vermillion edge (April, 2011) [Figure - 1]a. Dermoscopy was performed on this lesion at various stages of its clinical course. On the first dermatoscopy (January, 2010) of the brownish, mucosal macules, a typical multi-component pattern was observed, including a homogeneous and partly ring-like pattern [Figure - 1]b. In the course of several months, a blue-veil sign appeared, with disorganized dermatoscopic structures. One year later, a multi-component pattern was described, demonstrating pseudo-reticular, homogenous and non-specific patterns. In addition, within the vermillion edge, the granular-annular pattern was noted. The hair follicles were accentuated by annular rings surrounding the follicular ostium [Figure - 1]c. Because of the mucosal progression and metastases to the submandibular lymph nodes with distant metastases to lungs and liver, the patient underwent lymph node dissection of the submandibular region. He also received adjuvant chemotherapy with dacarbazine (DTIC), cisplatin (CDDP) and paclitaxel. The patient died 24 months after recognition of the initial melanoma because of advanced metastatic disease.
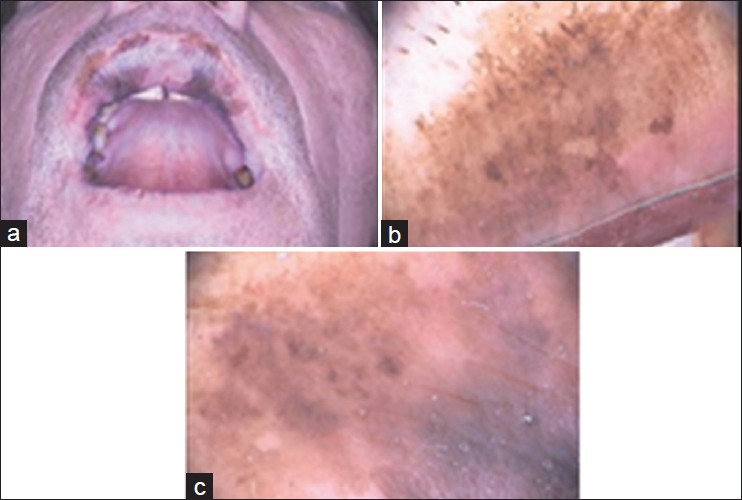 |
| Figure 1: (a) Melanoma (thickness Breslow 4.4 mm) involving the upper lip, vermillion edge and the skin above the upper lip. A whitish post-surgical scar is seen at the center. (b) Dermatoscopic appearance of the melanoma of the upper lip and vermillion in January, 2010: A typical multi-component pattern was observed, including a homogeneous and partly ring-like pattern. According to classification of the mucosal changes by Blum et al.[1] 3 patterns of pigmented lines were noted: Reticular and parallel lines, a pattern of dots, and circles. (c) Dermatoscopic appearance of the mucosal part of the upper lip in March, 2011: Partially arranged multiple dots and a blue pseudo-veil sign are noted |
Case 2
A 42-year-old woman was diagnosed with primary melanoma on the left auricle. She presented with a slowly enlarging asymptomatic patch of two years duration. Clinically, the lesion was 1.0 × 0.7 cm in size, with asymmetric, irregular borders and colors. This patch covered the posterior part of the helix of the ear, being brownish-blackish and oval-shaped [Figure - 2]a. On dermatoscopy, the multi-component pattern consisted of pigmented reticular structures, an atypical inverse network, the "island sign" with its irregular focal of the pigmented network, and whitish-bluish, homogenous structures. [Figure - 2]b. The patient underwent partial excision of the auricle with a satisfactory cosmetic result and clear surgical margins. Histopathology later confirmed the presence of lentigo maligna. The patient remains without any signs of local reccurrence after 16 months of follow-up.
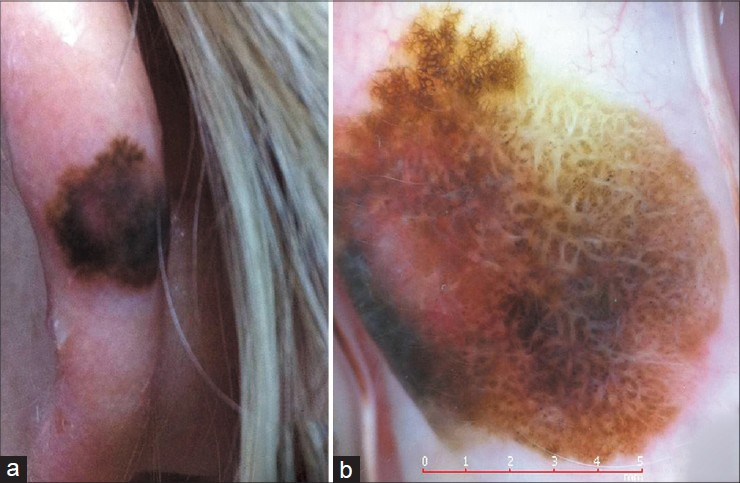 |
| Figure 2: (a) Lentigo maligna of the left auricle (helix). The lesion is 1.0 x 0.7 cm, with asymmetric, irregular borders and colors. (b) On dermatoscopy, a multi-component pattern with the presence of an atypical reticular with homogenous patterns is evident. The lesion shows multiple (6) colors, including light brown, brown, black, reddish, grayish and whitish. An inverse network, the �island sign� with its irregular foci, pigmented networks, dotted vessels distributed peripherally and whitish-bluish structureless zones was observed |
According to the results of a multicenter study by the International Dermoscopy Society, mucosal pigmented lesions located on lips were characterized by the occurrence of dermatoscopic patterns such as: structureless, lines, circles, dots and rarely globules or clods. [1] Overall, the most common detectable colors of the lesions on lips were brown, grey and red with black, white and purple colors being not very commonly detectable. [1] Comparing studies of Blum et al. [1] to Lin et al. [2] there are some differences in terminology of the mucosal changes. With regard to patterns, structureless was also referred to as homogenous pattern, globules/clods correspond to dotted-globular pattern, lines to finger-print, circles to ring-like pattern, and fish-scale to hyphal pattern. [1],[2] The most common patterns in mucosal melanoma of lips were structureless (100%), lines (54%) especially reticular (27%) and parallel (9%). [1] According to Blum et al. only the presence of structureless zones was significantly associated with malignant lesions. [1] Structureless patterns were found in all malignant lesions but only in 53.2% of benign lesions. [1] Dots were detectable in 28.6% of the malignant mucosal lesions and in 7.9% of the benign lesions. [1] According to Blum et al. multiple colors are a better clue to malignant lesions than multiple patterns. [1] Lin et al. stated that mucosal melanomas mainly presented with the multicomponent and homogeneous patterns. [2] In the differential diagnosis of benign melanosis of the lip, three major dermatoscopic patterns were identified: a "structureless" pattern with a blue hue, a "parallel pattern", often found in clinically typical melanocytic macules of the lips and the "reticular-like" pattern associated with melanosis, rather rarely occurring on the lips. [3] If a benign lesion was structureless, its color was usually brown but did not include blue, gray, or white. [1] The significant difference between benign and malignant lesions included not only the occurrence of blue, gray and white colors, but their number as well. [1]
According to Stante et al. a recognition of early signs of lentigo maligna on dermatoscopy, before the lesion is associated with the ABCD signs of melanoma, is a clue to early diagnosis. [4] The early dermatoscopic indicators of lentigo maligna are asymmetrical pigmented follicular openings, slate-grey short streaks and rhomboidal structures. [3],[4] Classic dermatoscopic features of extra-facial melanoma (an atypical pigment network, irregularly distributed dots, globules, streaks and pseudo-pods) and dermatoscopic criteria of vertical growth (ulceration, black structureless areas) have rarely been observed in cases of lentigo maligna. [5] In the case of lentigo maligna of the auricle presented above, a large number of colors, an atypical pigment network and a number of black, structureless areas were also noted. Furthermore, the features typical for melanoma in situ such as those described previously by Seidnari et al., were all seen in the present case. [6]
| 1. |
Blum A, Simionescu O, Argenziano G, Braun R, Cabo H, Eichhorn A, et al. Dermoscopy of pigmented lesions of the mucosa and the mucocutaneous junction: Results of a multicenter study by the International Dermoscopy Society (IDS). Arch Dermatol 2011;147:1181-7.
[Google Scholar]
|
| 2. |
Lin J, Koga H, Takata M, Saida T. Dermoscopy of pigmented lesions on mucocutaneous junction and mucous membrane. Br J Dermatol 2009;161:1255-61.
[Google Scholar]
|
| 3. |
Mannone F, De Giorgi V, Cattaneo A, Massi D, De Magnis A, Carli P. Dermoscopic features of mucosal melanosis. Dermatol Surg 2004;30:1118-23.
[Google Scholar]
|
| 4. |
Stante M, Giorgi V, Stanganelli I, Alfaioli B, Carli P. Dermoscopy for early detection of facial lentigo maligna. Br J Dermatol 2005;152:361-4.
[Google Scholar]
|
| 5. |
Pralong P, Bathelier E, Dalle S, Poulalhon N, Debarbieux S, Thomas L. Dermoscopy of lentigo maligna melanoma: Report of 125 cases. Br J Dermatol 2012;167:280-7.
[Google Scholar]
|
| 6. |
Seidenari S, Bassoli S, Borsari S, Ferrari C, Giusti F, Ponti G, et al. Variegated dermoscopy of in situ melanoma. Dermatology 2012;224:262-70.
[Google Scholar]
|
Fulltext Views
3,032
PDF downloads
1,692





