Translate this page into:
Primary mucocutaneous histoplasmosis presents as oral ulcer
Correspondence Address:
Chippi Vijayan
Dept of Dermatology and Venereology, Medical College, Trivandrum
India
| How to cite this article: Vijayan C, Suprakasan S, Kumar G N, Nair PS, Jayapalan S. Primary mucocutaneous histoplasmosis presents as oral ulcer. Indian J Dermatol Venereol Leprol 2007;73:209 |
Abstract
We are reporting a rare case of primary mucocutaneous histoplasmosis. A 47-year-old male with a part-time job of rearing pigeons presented with a non-healing oral ulcer with no associated systemic symptoms. Differential diagnosis of oral ulcerative lichen planus, squamous cell carcinoma and mucocutaneous leishmaniasis was considered. Histopathology showed multiple organisms with a peripheral halo, stained strongly with Gomori methenamine silver stain.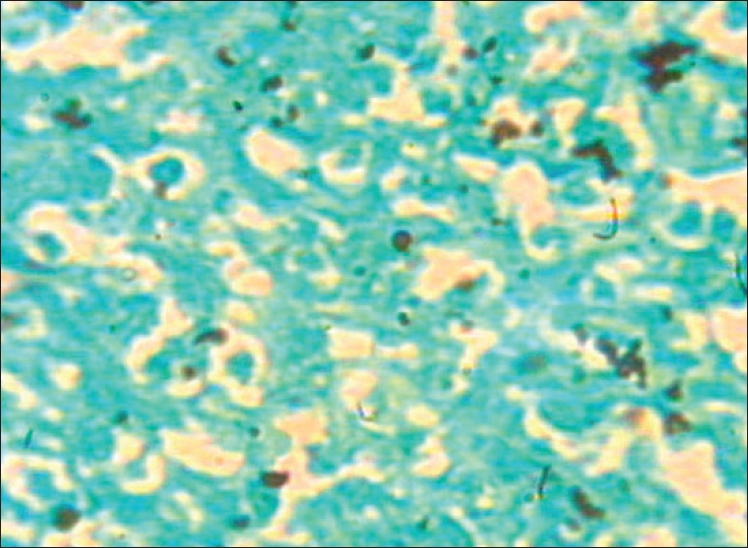 |
| Figure 4: Yeast cells with peripheral halo of size 2-5 �m, GMS stain |
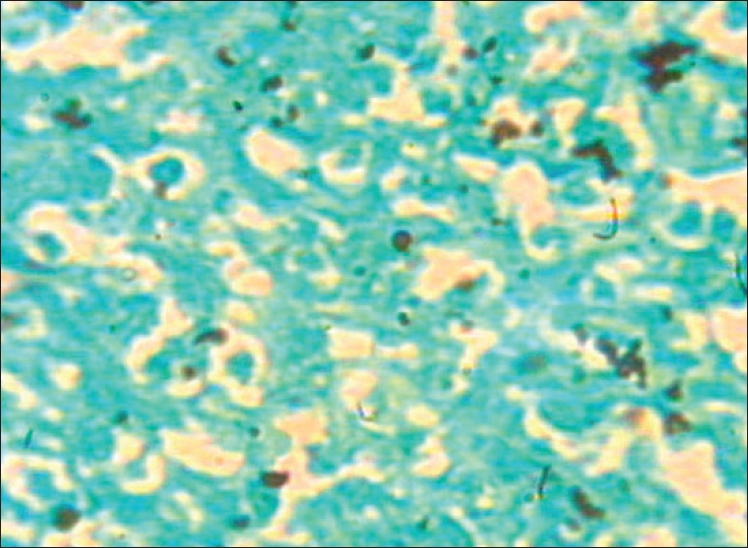 |
| Figure 4: Yeast cells with peripheral halo of size 2-5 �m, GMS stain |
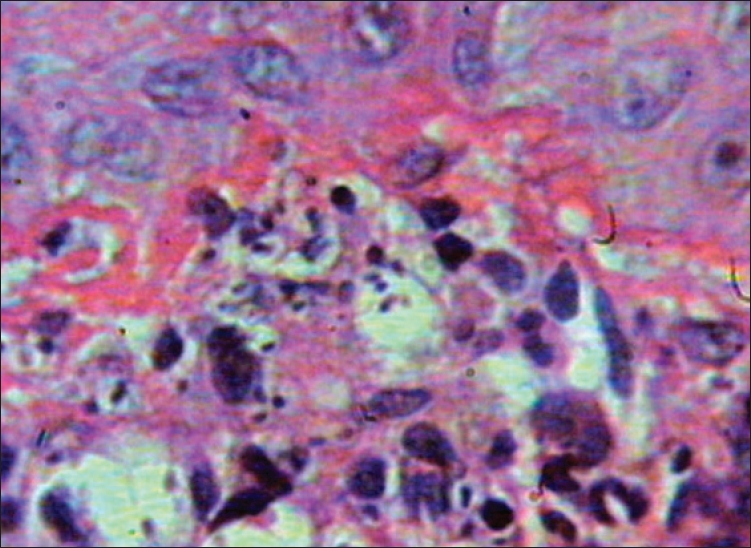 |
| Figure 3: Yeast cells within and outside macrophages (H and E stain, x100) |
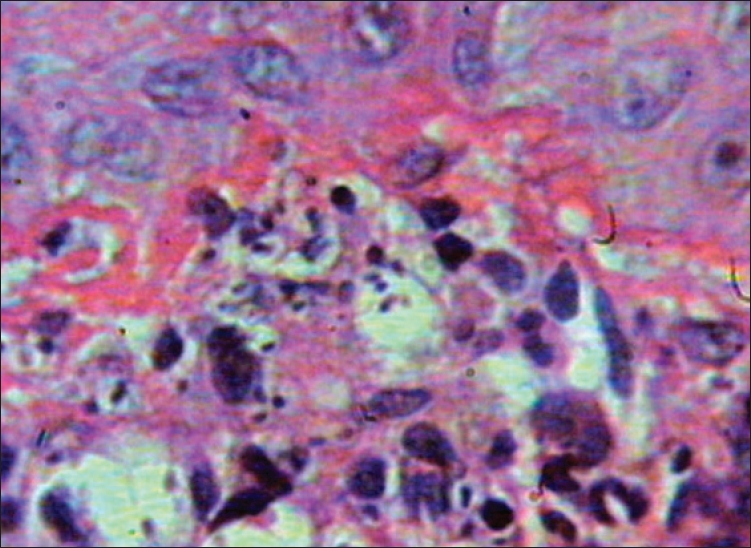 |
| Figure 3: Yeast cells within and outside macrophages (H and E stain, x100) |
 |
| Figure 2: Well-defined non-indurated ulcer near right mucocutaneous junction |
 |
| Figure 2: Well-defined non-indurated ulcer near right mucocutaneous junction |
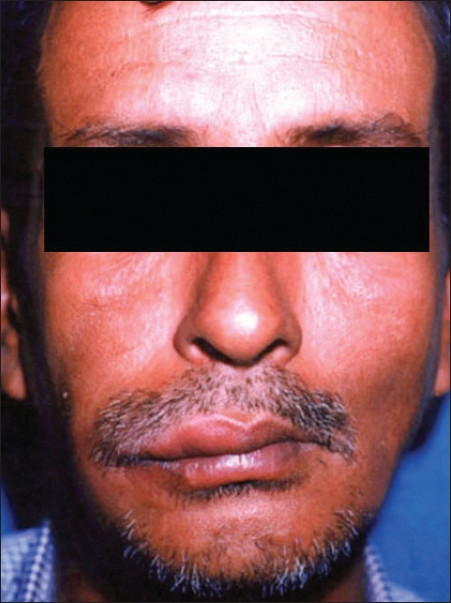 |
| Figure 1: Erythema and edema of right cheek |
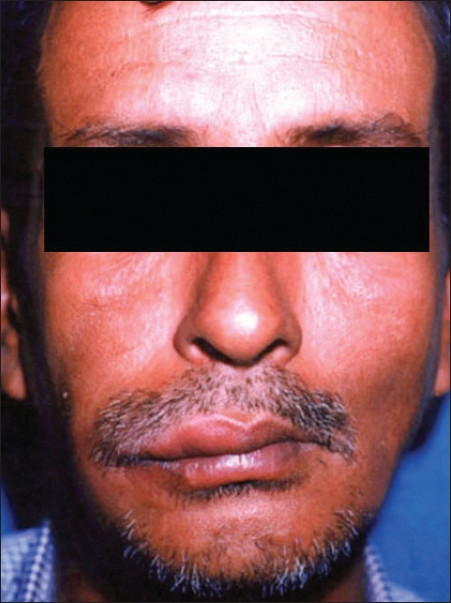 |
| Figure 1: Erythema and edema of right cheek |
Introduction
Histoplasmosis is a highly infectious mycosis, caused by Histoplasma capsulatum and affecting primarily the lungs, where it is generally asymptomatic. The fungus is intracellular, parasitizing the reticuloendothelial system and involving the spleen, liver, kidney, central nervous system and other organs. [1] It is a thermally dimorphic fungus. In human and animal tissue it forms small round budding yeast cells. [2] Two varieties of Histoplasma capsulatum are recognized: var capsulatum and var Duboisii . They have different sizes, the capsulatum variety producing cells from two to five mm in diameter, the Duboisii form 10 to 15 mm. [1]
Case Report
A 47-year-old male from Tamil Nadu, rearing pigeons as a part-time job, who was fond of petting and kissing them presented with a non-healing progressive oral ulcer of two months duration. He had incidentally noticed a small ulcer on his buccal mucosa, which gradually increased in size. Later, pain and edema of the corresponding cheek occurred. There were no other constitutional symptoms.
On examination, there was a well-defined tender, non-indurated ulcer of size 5x6 cm on the buccal mucosa near the right angle of mouth. There was associated erythema and edema of right cheek [Figure - 1]. The right cervical group of lymph nodes was enlarged and non-tender. There were no other systemic signs and symptoms [Figure - 2]. Differential diagnoses of oral ulcerative lichen planus, squamous cell carcinoma and mucocutaneous leishmaniasis were considered. Investigations revealed normal hemogram, peripheral smear and urine examination. Blood sugar, liver and renal function tests were within normal limits. Blood VDRL and TPHA were non-reactive and ELISA test for HIV was negative. Mantoux test was also negative. Radiography of chest and the right mandible was normal. Ultrasound of abdomen was within normal limits.
Histopathological examination of the ulcer using hematoxylin-eosin stain showed diffuse infiltrate of neutrophils, lymphocytes and macrophages and a few organisms within the dermis. Oil immersion view showed scattered multiple organisms of size 2-5 mm, with a peripheral halo outside and within macrophages and they stained strongly with Gomori methenamine silver (GMS) stain, suggestive of histoplasmosis [Figure - 3],[Figure - 4]. Leishman stain was also negative. Fungal culture carried out on Sabouraud′s dextrose agar did not yield any organisms.
The patient showed a prompt and excellent response to itraconazole given at a dose of 100 mgBD, with rapid healing of the ulcer within a week and the patient did not show any signs of recurrence of ulceration on subsequent follow-up visits.
Discussion
Histoplasmosis is the most common endemic mycosis in North America. Other endemic regions include parts of Africa, Australia and eastern Asia, in particular India and Malaysia. [2] Birds, bats and soil contaminated with their droppings are sources of infection. [3] Spores are infective not only to humans but also to small animals. The disease is transmitted by the inhalation of airborne conidia. Infection may follow introduction of spores through skin and mucous membrane. Histoplasmosis manifests itself in a bewildering array of clinical types and variations. It has been called the syphilis of the fungus world. [3]
There are now many known clinical forms of histoplasmosis. The four main clinical variants of histoplasmosis are acute pulmonary, acute disseminated, chronic disseminated and chronic pulmonary. Primary cutaneous histoplasmosis is very rare and appears after inoculation of the organism into the skin, [1] as in our case where direct inoculation into the mucosa occurred. Primary lesion is a nodule or indurated ulcer and there is often local lymphadenopathy with no systemic involvement. Our patient had no systemic symptoms and investigations ruled out any internal involvement. The lesions of primary cutaneous histoplasmosis involute spontaneously after a few months. Very rarely do such lesions occur in immunosuppressed patients. [3]
Disseminated histoplasmosis is an important complicating infection in patients with A ids0 and other immunocompromised states and is often rapidly fatal. The incidence and severity of fungal infection appears to increase with progression of HIV infection. [5] Oral lesions usually present as ulcers and commonly occur with disseminated disease. Differential diagnosis includes lichen planus, leishmaniasis, tuberculosis and squamous cell carcinoma. [6]
Diagnosis is established by identifying the small intracellular yeast cells (2-5 mm) of histoplasma in smears of mucocutaneous lesions, sputum, peripheral blood, bone marrow or in biopsy specimens. Leishmaniasis is the closest histopathological differential diagnosis where the organisms are of similar size but lack peripheral halo with nucleus and kinetoplast. PAS and GMS stains are positive only in the case of histoplasmosis. Culture is the gold standard for the diagnosis of histoplasmosis but its utility is limited by a two to four weeks waiting period and decreased sensitivity in self-limited disease as could be the reason for a negative culture in our case. Treatment for histoplasmosis has become considerably effective in recent years. For many disseminated or localized forms of the disease oral itraconazole is highly effective. [7] The prompt response to treatment and the rapid healing of the ulcer in our patient could be due to the localized form of the disease.
| 1. |
Hay RJ, Moore MK. Mycology. In : Tony B, Stephen B, Neil C, Christopher G, editors. Rook's Text Book of Dermatology. Blackwell Science Limited: London; 2004. p. 88-90.
[Google Scholar]
|
| 2. |
Richardson MD, Warnock DW. Fungal infection diagnosis and management. 3 rd ed. Blackwell Scientific Publications: London; 2003. p. 265-79.
[Google Scholar]
|
| 3. |
Rippon JW. The Pathogenic fungi and the pathogenic actinomycetes. 3 rd ed. Saunders: Philadelphia; 1988. p. 381-417.
[Google Scholar]
|
| 4. |
Pradeep NS, Vijayadharan M, Maya V. Primary cutaneous histoplasmosis. Indian J Dermatol Venereol Leprol 2000;66:151-3.
[Google Scholar]
|
| 5. |
Sayal SK, Prasad PS, Sanghi S. Disseminated histoplasmosis: Cutaneous presentation. Indian J Dermatol Venereol Leprol 2003;69:90-1.
[Google Scholar]
|
| 6. |
Sullivan MN, Whitby M, Chahoud C, Miller SM. Histoplasmosis in Australia: A report of case with a review of the literature. Aust Dent J 2004;49:94-7.
[Google Scholar]
|
| 7. |
Kurowski R, Ostapchuk M. Overview of histoplasmosis. Am Fam Physician 2002;66;160-2.
[Google Scholar]
|
Fulltext Views
2,084
PDF downloads
1,382





