Translate this page into:
Primary subcutaneous hydatid cyst of the leg: An unusual location and review of the literature
2 Department of Radiology and Medical Imaging Centre, Shohada-e-Tajrish Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Correspondence Address:
Fahimeh Abdollahimajd
Skin Research Center, Shahid Beheshti University of Medical Sciences, Shohada-e-Tajrish Hospital, Shahrdari St., 1989934148, Tehran
Iran
| How to cite this article: Moravvej H, Haghighatkhah HR, Abdollahimajd F, Aref S. Primary subcutaneous hydatid cyst of the leg: An unusual location and review of the literature. Indian J Dermatol Venereol Leprol 2016;82:558-562 |
Sir,
Hydatid disease is an endemic zoonotic infestation caused by the larval form of Echinococcus species.[1],[2] The most commonly afflicted organ is the liver but any tissue other than hair, nails and teeth may be involved.[3],[4] Primary subcutaneous involvement is rare and in these cases, even with inflammatory signs, a painless mass is the usual presentation.[1],[5] We describe a case of solitary subcutaneous hydatid cyst on the anterior aspect of the leg with clinical features of cellulitis.
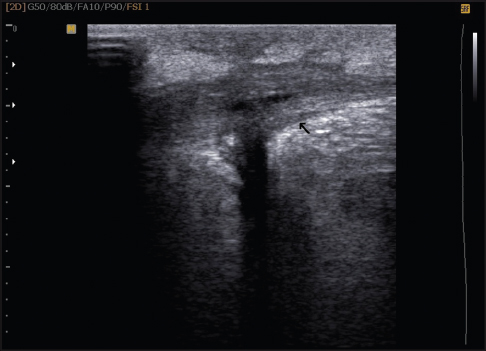
A 34-year-old Iranian man presented with a painful erythematous swelling on the anterior aspect of his right leg for 5 months. At onset, he noticed purulent discharge from the swelling. He had taken multiple courses of antibiotics and had used 10% ichthyol ointment topically which led to a partial improvement in erythema but no change in the swelling. On examination, there was a tender, ill defined, skin-colored swelling of size 6 cm × 8 cm with two visible sinus tracts covered with hemorrhgic crusts [Figure - 1]. Ultrasonography revealed a thick-walled collapsed cystic lesion in the superficial part of the anterior tibialis with a sinus tract extending into the underlying muscle. The wall thickness was 5 mm [Figure - 2]. The lesion was excised in its entirety and macroscopic examination revealed a cystic mass. On histopathologic examination, the lesion showed a periodic acid–Schiff-positive laminated membrane with no germinal epithelium or protoscolex. Therefore, the diagnosis of a hydatid cyst was made [Figure - 3]. The patient denied close contact with animals, prior history of trauma at the site or any previous surgery for hydatid cysts. Serum anti-Echinococcus granulosus immunoglobulin G (IgG) was positive. A thorough radiologic evaluation of other organs (including total bone scan and computed tomography of the chest, abdomen and pelvis) failed to detect a primary focus. Following excision, the patient received 400 mg of albendazole twice a day for 1 month and he remained free of recurrence at follow up 6 months later.
 |
| Figure 1: Preoperative subcutaneous mass of the leg after antibiotic therapy |
 |
| Figure 2: Ultrasonography of the cystic lesion |
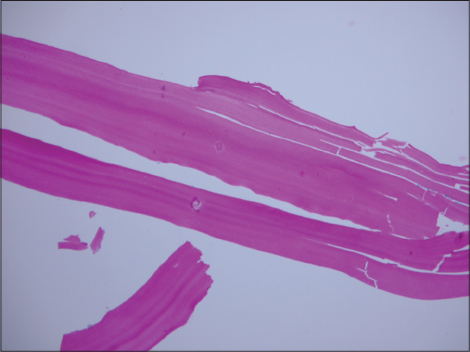 |
| Figure 3: The periodic acid–Schiff-positive laminated wall, characteristic of Echinococcus cyst (periodic acid–Schiff stain, ×400) |
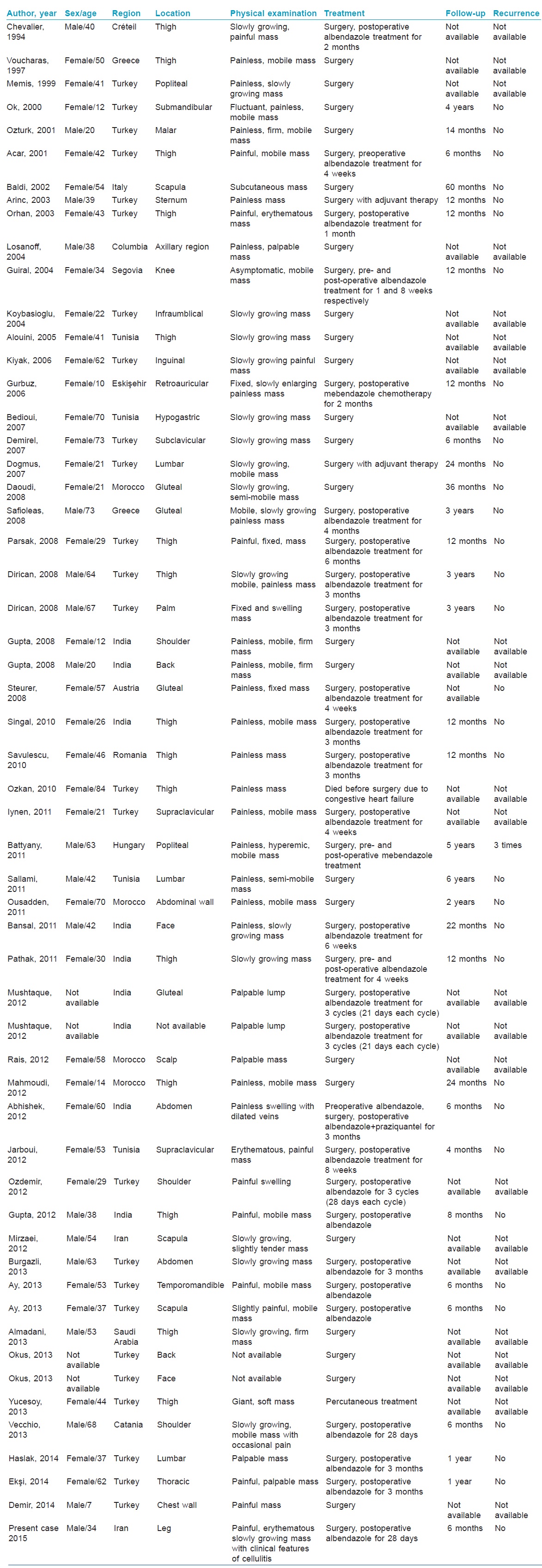
Echinococcus granulosus infection may remain asymptomatic for years or may manifest with dangerous complications such as infection, rupture, anaphylaxis and death.[5] We were able to find 55 reported cases of primary subcutaneous hydatid cysts [Table - 1].[1],[4],[5] However, we were unable to find any previous case of primary subcutaneous hydatid cyst located on the leg.
Subcutaneous hydatid cyst can be either secondary or primary. The secondary type is associated with an underlying primary focus of hydatid disease such as the liver.[2] On the other hand, the mechanism of primary subcutaneous localization is still not completely clear. There are two potential mechanisms: systemic dissemination via the lymphatic route or direct subcutaneous contamination through injured skin. In our patient, the first mechanism seems plausible as he had no history of skin injury.[6]
In a review of 22 cases of primary subcutaneous hydatid cysts, the age and sex distribution of patients was found to be similar to patients with liver hydatid cysts.[6] The most frequent subcutaneous location was the thigh followed by the gluteal region whereas the upper extremities were least commonly involved.[1],[6] The usual presentation of subcutaneous hydatid cyst is in the form of a painless, non-inflammatory and slowly growing mass without any deterioration of the patient's general condition; but our patient initially presented with clinical signs of cellulitis.[3],[7] Diagnosis of hydatid cysts, especially the subcutaneous form is very difficult in patients from non-endemic areas. Preoperative diagnosis is important because of the risk of anaphylactic reaction or local recurrence due to accidental leakage of contents of the cyst during surgery undertaken without a diagnosis; but these have not been reported in the subcutaneous type.[2],[6] Radiologic investigations such as ultrasonography, magnetic resonance imaging and computed tomography are useful in the diagnosis of soft tissue masses and also to delineate the relationship of the cyst to adjacent structures.[6] Although serology is helpful particularly for liver hydatid cysts, it is negative in 79% of subcutaneous cysts; but our patient had a positive test. It is recommended that all patients with subcutaneous hydatid cyst must have a whole body screening to detect any additional foci.[4],[6]
The main treatment of subcutaneous hydatid cyst is surgical excision. Subcutaneous cysts need less extensive surgery than visceral cysts and contrary to liver hydatidosis, complete excision of subcutaneous cysts is possible but they are more susceptible to rupture because of the difficulty of preoperative diagnosis.[2],[6] In cases of rupture, the cyst pouch should be irrigated with protoscolocidal solutions and the patient must receive a cover of antihelminthic drug like albendazole.[1],[6] In general, the prognosis of primary subcutaneous hydatid cyst is quite good and relapse is very uncommon if the lesion is excised completely.[1]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Vecchio R, Marchese S, Ferla F, Spataro L, Intagliata E. Solitary subcutaneous hydatid cyst: Review of the literature and report of a new case in the deltoid region. Parasitol Int 2013;62:487-93.
[Google Scholar]
|
| 2. |
Dirican A, Unal B, Kayaalp C, Kirimlioglu V. Subcutaneous hydatid cysts occurring in the palm and the thigh: Two case reports. J Med Case Rep 2008;2:273.
[Google Scholar]
|
| 3. |
Ousadden A, Elbouhaddouti H, Ibnmajdoub KH, Mazaz K, Aittaleb K. A solitary primary subcutaneous hydatid cyst in the abdominal wall of a 70-year-old woman: A case report. J Med Case Rep 2011;5:270.
[Google Scholar]
|
| 4. |
Mirzaei T, Hooshyar H. Primary subcutaneous hydatid cyst in scapula. Iran J Pathol 2012;7:259-61.
[Google Scholar]
|
| 5. |
Almadani N, Almutairi B, Alassiri AH. Primary subcutaneous hydatid cyst with palisading granulomatous reaction. Case Rep Pathol 2013;2013:126541.
[Google Scholar]
|
| 6. |
Kayaalp C, Dirican A, Aydin C. Primary subcutaneous hydatid cysts: A review of 22 cases. Int J Surg 2011;9:117-21.
[Google Scholar]
|
| 7. |
Abhishek V, Patil VS, Mohan U, Shivswamy BS. Abdominal wall hydatid cyst: Case report and review of literature. Case Rep Surg 2012;2012:583294.
[Google Scholar]
|
Fulltext Views
4,171
PDF downloads
1,879





