Translate this page into:
Procedural dermatology and its unmet need
Corresponding author: Dr. Somesh Gupta, Professor, Department of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi, Delhi, India. someshgupta@aiims.edu
-
Received: ,
Accepted: ,
How to cite this article: Mehta N, Sharma A, Sindhuja T, Dudani P, Sahni K, Khanna N, et al. Procedural dermatology and its unmet need. Indian J Dermatol Venereol Leprol 2023;89:807-18.
Abstract
Procedural dermatology includes invasive conventional dermatologic surgeries which involve significant use of knife and suture, minimally invasive procedures and device-based procedures. Device-based procedures are the easiest to learn and are less prone to human errors due to automation but can lead to monotony, while conventional surgeries require significant skill, craftsmanship and interest. There has been a recent shift in the approach to procedural dermatology as a therapeutic option with complementary and combination models replacing the conventional hierarchical model in which procedures were last in the step-ladder approach. The demand for both conventional dermatologic surgeries and minimally invasive cosmetic procedures is increasing. Unfortunately, this demand has not been met with adequate supply. Consequently, the number of trained professionals with expertise in these procedures is very limited; they are far outnumbered by unqualified practitioners. A limited number of dermatologic surgeons practicing conventional surgeries has resulted in huge waiting lists for vitiligo surgeries, inappropriate excisions for skin cancers and poor cosmetic outcomes of excisions without proper knowledge of flaps and grafts. Increasingly procedures are being performed by inadequately trained personnel, resulting in complications. There is also an absence of good quality research on the subject of procedural dermatology, which has resulted in a lack of standardisation of various procedures and knowledge about the efficacy of various drug-procedure and procedure-procedure combinations. An increasing variety of gimmicky but costly procedures are being offered to the public without much evidence of efficacy. Individual institutional and broad policy directives are needed to address these issues. Special emphasis is required on formal hands-on procedural dermatology training during residency and beyond it.
Keywords
Procedural dermatology
dermatologic surgery
dermatosurgery resident training
dermatology curriculum
cosmetic surgery
Introduction
Procedural dermatology has become an integral and essential component of dermatology practice. The American Society for Dermatologic Surgery refers to dermatologic surgery as “a specialty dealing with the diagnosis and treatment of medically necessary and cosmetic conditions of the skin, hair, nails, veins, mucous membranes and adjacent tissues by various surgical, reconstructive, cosmetic, and non-surgical methods.”1 They propose that dermatologic surgery aims to repair and/or improve the function and cosmetic appearance of skin tissue. The University of North Carolina School of Medicine defines procedural dermatology as “the subspecialty within dermatology that is concerned with the study, diagnosis, and surgical treatment of diseases of the skin and adjacent mucous membranes, cutaneous appendages, hair, nails, and subcutaneous tissue.”2 ‘Procedural dermatology’ is a broader and perhaps better term which also includes the usage of energy-based devices, simple and less invasive cosmetic procedures like botulinum toxin and filler injections and other ‘non-surgical’ and ‘semi-surgical’ techniques, in addition to the core ‘scalpel and blade’ procedures which come to mind when the conventional term ‘dermatologic surgery’ Is used.
Classification
Procedural dermatology can be divided into three categories, based on the invasiveness and complexity of procedures, the skills required to learn them and their technological dependence.
Conventional dermatologic surgeries include invasive techniques involving significant tissue cutting and suturing. These reasonably complex interventions are aimed at alleviating symptoms and/or enhancing cosmesis.
Minimally invasive procedures (excluding device-based procedures) include ‘non-surgical’ less invasive techniques such as botulinum toxin injections and fillers. Many, but not all of them, are aesthetically enhancing and relatively newer than conventional dermatologic surgeries.
Laser, light and energy device-based procedures primarily involve using these devices and require less skill than conventional dermatologic surgeries. Apart from their primary use in cosmetic procedures, these devices can also be used to aid conventional dermatologic surgery; an example is laser-assisted recipient epidermis removal during grafting procedures in vitiligo.
In Table 1, we summarise the skills required, the monetary investment needed and the perceived return on investment for common procedures in dermatology, based on an online survey using Google Forms from 53 procedural dermatologists (authors’ unpublished data). Neither is this list exhaustive, nor are the categories watertight. In general, conventional dermatologic surgeries are skill-intensive, have a longer learning curve, involve significant craftsmanship and require low-to-moderate monetary investment. They are not automated and are thereby more prone to human errors and complications. Currently, they are performed by limited well-trained experts in dermatologic surgery. Minimally invasive procedures are relatively easily mastered, require low initial monetary investment but have a moderate-to-high return. As evident from Table 1, even the seemingly ‘simple’ and quick minimally invasive procedures like botulinum toxin and filler injections are considered to require significant skills, because they necessitate a comprehensive knowledge of complex facial anatomy and carry the risk of complications. They are among the most common procedures done by procedural dermatologists. Though they are often initiated early in their careers by most beginners, significant experience is required to master them. The device-based procedures tend to suffer from the drawback of a high ratio of investment: initial return. They are generally automated with few predetermined selected parameters; thus they are safer, less prone to human errors and are easy to deliver by minimally-trained professionals. Automation and overdependence on technology can bring boredom and monotony to practice that could possibly even outweigh the monetary returns. One needs to balance both skill-intensive and technology-intensive procedures in practice.
| Procedure | Skill level, on a Likert scale of 1-5* | Monetary investment, on a Likert scale of 1-5* | Return on investment, on a Likert scale of low-moderate-high* |
|---|---|---|---|
| Median (range) | Median (range) | (Mode) | |
| Conventional dermatologic surgery | |||
| Reconstructive flaps and grafts | 5 (1-5) | 4 (1-5) | Moderate |
| Scar revision | 4 (1-5) | 3 (1-5) | Moderate |
| Autologous fat transfer | 4 (1-5) | 4 (1-5) | Moderate |
| Hair restoration surgery | 4 (1-5) | 4 (1-5) | High |
| Vitiligo surgeries | 4 (2-5) | 3 (1-5) | Moderate |
| Nail surgeries | 4 (2-5) | 2 (1-5) | Moderate |
| Serial excision | 4 (1-5) | 3 (1-5) | Moderate |
| Simple excision and punch excision | 3 (1-5) | 2 (1-5) | Low |
| Minimally invasive procedures | |||
| Dermabrasion | 3 (1-5) | 2 (1-4) | Moderate |
| Microdermabrasion | 2 (1-5) | 2 (1-4) | Moderate |
| Injectable fillers | 4 (1-5) | 4 (1-5) | High |
| Botulinum toxin | 4 (1-5) | 3 (1-5) | High |
| Chemical peels | 3 (1-5) | 3 (1-5) | Moderate |
| Microneedling | 2 (1-5) | 2 (1-4) | Moderate |
| Thread lift | 4 (2-5) | 3 (1-5) | Moderate |
| Intralesional injections | 2 (1-5) | 2 (1-5) | Moderate |
| Subcision | 3 (1-5) | 2 (1-5) | Moderate |
| Laser, light and energy-based devices | |||
| Vascular lasers | 4 (2-5) | 5 (2-5) | Moderate |
| Pigment lasers | 4 (2-5) | 4 (2-5) | Moderate |
| Phototherapy | 3 (1-5) | 3 (1-5) | Moderate |
| Hair removal lasers | 3 (1-5) | 4 (2-5) | High |
| Non-ablative fractional lasers | 3 (1-5) | 4 (2-5) | Moderate |
| Electrosurgery and radiofrequency | 3 (1-5) | 3 (1-5) | High |
| Microneedling radiofrequency | 3 (1-5) | 3 (1-5) | Moderate |
| Skin tightening and body contouring devices | 3 (1-5) | 4 (1-5) | Moderate |
| Fat reduction devices | 3 (1-5) | 4 (1-5) | Moderate |
*Unpublished data obtained from survey of 53 experts in dermatologic surgery by circulating an online form
History and current status
Milestones
The beginning of procedural dermatology perhaps predates recorded history.3 Skilled dermatologic surgeons extensively use flaps and reconstructions, and this use dates back to the time of Sushruta, an Indian pioneer in dermatologic and plastic surgery.4 Modern “procedural dermatology” formally started around half a century ago when various like-minded dermatologists practicing different procedural interventions collaborated and started a separate publication focusing on this sub-division of dermatology.5 Prof. Lawrence Field is considered the father of modern dermatologic surgery.6 In India, two organisations dedicated to the field of dermatologic surgery, namely, the Association of Dermatological Surgeons of India and the Indian Academy of Cutaneous Surgeons, were launched in 1993 in Manipal and Kolkata, respectively. They were later merged to form the Association of Cutaneous Surgeons of India.7
Dermatologists have been pioneers in chemical peeling,8 cryosurgery,9 vitiligo surgeries,10 hair transplantation surgeries,11 soft tissue augmentation and rejuvenation procedures. A large number of aesthetic or cosmetic procedures, like hair transplantation, were started first by dermatologists and later adopted by others.6 Although not primarily discovered by dermatologists, dermatologists perform the maximum number of botulinum toxin injections,12 skin cancer excisions including Mohs’ surgery,13 liposuction14 and electrosurgery15 [Table 2]. In the USA, the volume of reconstructive surgical procedures by dermatologists exceeds that of any other specialty, including plastic surgery.16 Not only do dermatologists perform more excisions for skin cancers, but they also do so better and more adequately than other practitioners.17 Dermatology probably utilises the highest numbers of lasers, light sources and energy-based devices amongst the various medical specialties.
| Procedure | First described in modern history by? | Year of first description | Currently predominant practitioners |
|---|---|---|---|
| Chemical peeling | Ferdinand von Hebra, Austrian dermatologist | 1860 | Dermatologists |
| William Tilbury Fox, British dermatologist | 1871 | ||
| Vitiligo surgeries | Pran Nath Behl, Indian dermatologist, thin Thiersch skin grafts | 1964 | Dermatologists |
| Rafael Falabella, Italian dermatologist, suction blister grafting and mini-punch grafting | 1971 1978 |
||
| Cryosurgery and cryosurgery using refrigerants | James Arnott, English physician, for various tumours and some skin conditions | 1845-1851 | Dermatologists |
| Archibald Campbell White, American physician, for skin conditions | 1899 | ||
| Electrosurgery | Joseph Riviere, French physician | 1900 | All surgical fields for hemostasis, dermatologists for most indications including resurfacing |
| Harvey Cushing, American neurosurgeon, along with William T Bovie, biophysicist | 1926 | ||
| Botulinum injections | Alan Brown Scott, American ophthalmologist, for strabismus | 1980 | Many surgical specialties, but most commonly performed by dermatologists for cosmetic reasons |
| Jean Carruthers and Alastair Caruthers, Canadian ophthalmologist and dermatologist, respectively, for glabellar frown lines | Procedure in 1987, article published in 1992 | ||
| Mohs’ surgery | Frederic Mohs, American surgeon | Procedure in 1936, article published in 1941 | Mostly by dermatologists, also by plastic surgeons and general surgeons |
| Liposuction | Arpad Fischer and Giorgio Fischer, Italian gynaecologists, blunt cannula liposuction | 1975 | Plastic surgeons and dermatologists |
| Jeffrey Klein, American dermatologist, tumescent liposuction without requirement of general anaesthesia | 1987 | ||
| Hair transplant for patterned baldness | Norman Orentreich, American dermatologist | 1959 | Dermatologists and plastic surgeons |
Shift in models
Earlier, a conservative mindset was supported by limited availability and experience of procedural modalities, hence the general hierarchical approach of dermatologists was to first try medical interventions while procedures played a supplementary role and often required referral to surgical disciplines [Figure 1a]. Many diseases were considered untreatable as they were not amenable to any medical therapy, and patients were counselled without attempting any procedure in line with the ‘first do no harm’ principle. For diseases like early-stage androgenetic alopecia, melasma and other pigmentary disorders, a hierarchical model is still valid, that is, they are generally treated first with medical treatment and if medical treatment fails, procedures can be tried.18,19
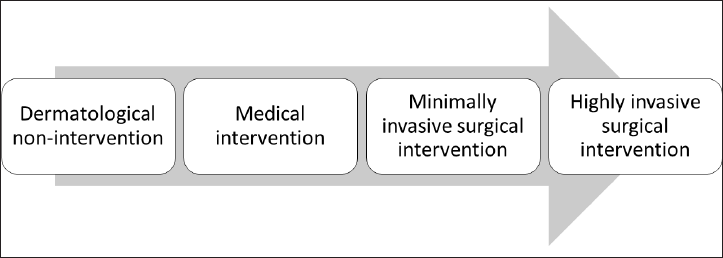
- Models of dermato-therapeutics: (a) Conventional hierarchical model
However, with the established efficacy, safety and wide availability of a variety of procedures, the hierarchical model has given way to complementary [Figure 1b] and combination models [Figure 1c]. Many diseases previously considered untreatable are now offered procedures as the first-line modality for management (e.g., acrochordons, vascular malformations, tattoos, epidermal, pigmented and vascular nevi, mucoceles, cysts and malignant tumours).20-22 Procedures are also indicated to tackle residual changes following successful medical management of certain conditions (e.g., leprosy, panniculitis, linear morphea and infantile haemangiomas).23-25 Certain conditions involve utilising a combination of medical and physical modalities initially itself (e.g., keloids, acne scars and chromoblastomycosis).26,27 Hence, medical and procedural dermatology should now be considered complementary to each other.
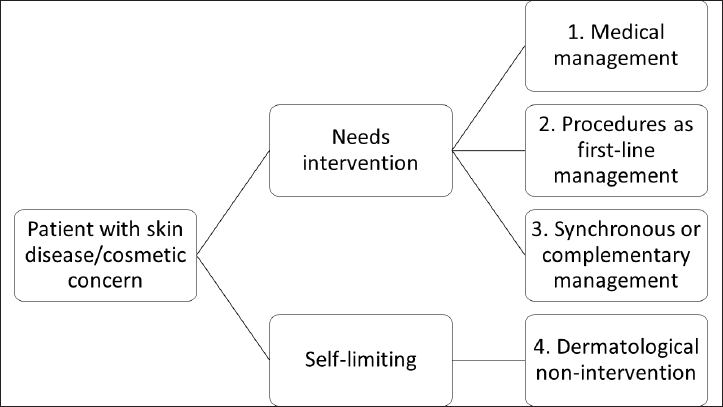
- Models of dermato-therapeutics: (b) Complementary model
- Models of dermato-therapeutics: (c) Combination model
The division of management of diseases into these models is not clear-cut or uniformly accepted. The choice of order of utilising these modalities is also subjective and based on physician preference. Often clear guidelines do not exist and even if they do, patient preference is also a determining factor, examples being the choice of utilising medical treatment versus a surgical modality as the first-line treatment for segmental vitiligo. Similarly, for many conditions, the levels of the traditional hierarchical approach are also in the process of rearrangement, the classic example being the utility of early surgical intervention versus prolonged antibiotic therapy in moderate-to-severe hidradenitis suppurativa.28,29 The decision of whether to use a procedure as the first-line or medical treatment or combination should be need-, cost- and evidence-based.
Current demand
The demand for procedural dermatology is growing exponentially. A total of 11.3 million surgical and 13.6 million non-surgical procedures were performed worldwide in 2019, 3.8% and 1.6% of which respectively were done in India. India ranked fourth amongst all included countries in liposuction, sixth in hair removal and eighth in facial rejuvenation.30 Hair transplantation,31,32 botulinum toxin injections33 and medical aesthetic device-based procedures34 have either shown or are predicted to show, a double-digit annual growth rate in India and the world. In the USA, there has been an exponential increase in body sculpting procedures, laser/light and energy-based treatments, fillers, wrinkle-relaxing procedures and procedures to remove non-melanoma skin lesions.35
This rise in demand has been consistent despite the global financial crisis of 2007-2008 and the COVID-19 pandemic.36,37 The USA had a 54% increase in botulinum toxin injections and a 75% increase in filler treatments in 2020 compared to 2019.38 In 2020, while conventional surgical procedures dropped by 10%, there was a 5% rise in minimally invasive cosmetic procedures worldwide. India accounted for 5% of these procedures, with hair removal and facial rejuvenation being the most common.39
The social factors contributing to this rapid rise in the patient pool include an enhanced consciousness about looks, a direct perceived correlation between attractiveness and ‘success’ at work and in relationships, minimal downtime of the newer procedures, social-media-driven goals of appearance, the background lack of regulatory controls over such procedures and increasing disposable incomes in contrast to earlier economic frugality.40-42
Training and research opportunities
There are many fellowships in procedural dermatology in India and the rest of the world, including the USA, UK, Europe, Australia, Middle East and South-East Asia. These range from six months to two years in duration. The American Society for Dermatologic Surgery has certified fellowship programmes in cosmetic dermatologic surgery and procedural dermatology. The latter has 47 participating programmes offering 55 positions annually, which are highly contested.43 The American Society for Dermatologic Surgery has four other internationally recognised procedural dermatology training programmes in South Africa, Romania, Pakistan and the Netherlands,44 and programmes for international graduates. The International Traveling Mentorship Program was established in 2010 through the Lawrence Field, MD, International Dermatologic Surgery Education Exchange Fund to enhance the surgical skills of dermatologists and to facilitate the exchange knowledge between international counterparts.45 Through the International Traveling Mentorship Program, the American Society for Dermatologic Surgery and Dermatologic and Aesthetic Surgery International League assist dermatologic surgeons to visit a host institution in another country or host a dermatologic surgeon from another country for a defined period of training. The list of approved mentors/hosts under the International Traveling Mentorship Program is mentioned in Table 3. The UK’s British Society for Dermatological Surgery offers post-residency fellowships in Mohs and advanced dermatological surgery at eight centres.46 The Netherlands also has a fellowship training programme,47 and Australia offers multiple 1-2 years of procedural dermatology training programmes.48
| S. no | Sponsoring organisation | Country | Centres/Doctors | Programme and duration | Eligibility |
|---|---|---|---|---|---|
| 1. | ASDS and DASIL | USA | Variable. Established through the Lawrence M. Field, MD, International Dermatologic Surgery Educational Exchange Fund73 |
International Preceptorship Program, 1-3 weeks | International dermatologic surgeons (i.e., not American or Canadian and not residents-in-training) practicing full-time in an academic institution or private practice Current member of the ASDS or another internationally recognised dermatologic surgery organisation |
| Saudi Arabia | Salman AlSaad, MD | International Traveling Mentorship Program,45 up to 4 weeks | Considered hosts must be an ASDS or other member. Be in an authoritative position in dermatologic surgery at a hosting institution | ||
| USA | Brett Coldiron, MD Terrence Cronin, MD Roberto L. Davila-DePedro, MD Daniel Eisen, MD Michael Gold, MD Patrick Lillis, MD Peter J. Panagotacos, MD Thomas Rohrer, MD Christine H. Weinberger, MD |
||||
| Indonesia | Khairuddin Djawad, MD Moerbono Mochtar, MD Chadijah Rifai, MD Indah Julianto, MD, PhD |
||||
| Canada | Sahar Ghannam, MD | ||||
| India | Somesh Gupta, MD Nilesh N. Goyal, MD |
||||
| Germany | Michael Haeberle, MD Eckart Haneke, MD, PhD Mark Tanner, MD |
||||
| Hungary | Istvan Juhász, MD | ||||
| Netherlands | Gertruud Kreckels, MD | ||||
| Israel | Marina Landau, MD Isaac Zilinsky, MD |
||||
| Romania | Mihaela Leventer, MD | ||||
| Dubai | Mahaveer Mehta, MD Syed A.A. Shah, FRCP (UK), CCST (UK) |
||||
| UK | Richard J. Motley, FRCP | ||||
| Greece | Constantine Noutsis, MD, PhD | ||||
| South Africa | Derek Odendaal, MD Marc B. Roscher, MD |
||||
| Brazil | Ramos-e-Silva, MD, PhD | ||||
| Philippines | Manalo-Manuel Remedios, MD | ||||
| South Korea | Ki Hoon Song, MD | ||||
| Thailand | C. Treewittayapoom, MD | ||||
| 2. | NYU Langone’s Health | USA | Skin and cancer unit of the Ronald O. Perelman, Department of Dermatology at NYU Langone ambulatory care center, and faculty practice of Jerry Shapiro, MD74 | International Observership Program in Dermatology, 1 month* | Completed documented formal training in dermatology at least equivalent to a residency or in another subspecialty or area of interest relevant to the practice of dermatology, such as public health or infectious disease |
| 3. | Cleveland Clinic | USA | Dermatology and Plastic Surgery Institute, Center for International Medical Education75 | International Physician Observership Program, 1 month | Fully trained international practicing physicians and specialists International residents, fellows and medical students currently enrolled in a residency/fellowship programme at a foreign institution and who are expected to graduate from that same school/institution |
| 4. | MD2B Connect | USA | St. Louis, Missouri76 | Outpatient externship in dermatology** | International medical graduates and students seeking hands-on patient care experience in dermatology |
| 5. | Wake Forest School of Medicine | USA | Rita Pichardo-Geisinger, MD, Department of Dermatology77 | International Dermatology Fellowship Program, 6 months-1 year | International dermatology residents or dermatology graduates |
| 6. | National Skin Centre | Singapore | National Skin Centre78 | Clinical Hands-On Fellowship, 3-12 months** | A recognised basic degree in medicine and traineeship or specialist degree in dermatology |
| 7. | Seoul National University Hospital | Korea | Dong Hun Lee, Department of Dermatology79 | Short-term visiting fellowship programme, 2-4 weeks*** | Dermatologists |
| 8. | Mahidol University | Thailand | Department of Dermatology at Faculty of Medicine Siriraj Hospital80 | Clinical fellowship in dermatologic surgery, 1 year | Dermatologist, MSc in dermatology |
| 9. | Rajiv Gandhi University of Health Sciences | India (Bengaluru) | Bangalore Medical College and Research Institute81 CUTIS Academy of Cutaneous Sciences82 Kempegowda Institute of Medical Sciences83 St. John’s Medical College84 Venkat Charmalaya85 |
Dermatosurgery, Aesthetic Dermatology, Lasers (6 months-1 year); hair Transplantation (1-2 weeks) |
MD/DVD/DNB in dermatology Three years’ experience DM/MCH/DNB in concerned specialty Plastic surgeons (preferably with 2 years of professional experience after post-graduation) |
| 10. | Maharashtra University of Health Sciences | India | Institute of Skin Cosmetology and Lasers, Solapur86 | Basic phototherapy and lasers, 1 year | MD, DNB or DVD in dermatology, venereology and leprosy |
| 11. | DY Patil University | India | Shrilata Suresh Trasi, Pradeep Sethi, Mumbai87 | Fellowship in cosmetology (6 months), hair transplant (1 year) | MD or diploma in dermatology |
| 12. | Datta Meghe Institute of Medical Sciences | India | Jawaharlal Nehru Medical College & AVBRH88 | Fellowship in dermatosurgery | MD/DNB in dermatology |
| 13. | JIPMER | India | JIPMER89 | Lasers and dermatosurgery, 1 year | MD/DNB in dermatology |
| 14. | Christian Medical College | India | Department of Dermatology90 | Post-Doctoral Fellowship in Dermatosurgery, 1 year | MD/DNB in dermatology |
| 15. | IADVL (https://www.iadvl.org/) | India | Chiranjiv Chhabra and Kavish Chouhan, New Delhi Dasika Subba Rao, Eluru Sachin Varma, Kolkata Sumit Sharma, Panipat |
Training course in procedural dermatology, 3 months91 | Candidates who have obtained their MD or diploma or DNB in dermatology |
| 16. | IADVL (https://www.iadvl.org/) | India | Yogesh M Bhingradia, Surat Suruchi Garg, Chandigarh Parmjit Singh Walia, Mohali Muhammed Razmi, Calicut Debjit Kar, Odisha Mahendra Deora, Pune Sumit Gupta, Lucknow Koushik Lahiri, Kolkata Vishalakshi Viswanath, Thane Subrata Malakar, Kolkata Rohit Bansal, Chandigarh Madhavi Pudi, Hyderabad J K Sadana, Patiala Sachin Varma, Kolkata Sumit Sharma, Panipat Imran Majid, Srinagar |
Dermatosurgery, aesthetic dermatology, lasers, phototherapy, phlebology, hair transplant; 2-4 weeks92 | Candidates who have obtained their MD or diploma or DNB in dermatology |
| 17. | ACS(I) | India | Dhanashree Bhide, Pradyumna Vaidhya, Pune Imran Majid, Srinagar Jaishree Sharad, Mumbai Koushik Lahiri, Kolkata Niteen Dhepe, Pune Niti Khunger, New Delhi Raj Kirit, Rajyalakshmi, Hyderabad Venkataram Mysore, Bengaluru |
Training observerships in dermatosurgery, laser surgery and cosmetic dermatology; 2-4 weeks49 | Life members of the ACS(I) who are not working in the same institution and who have completed their degree or diploma. |
ASDS: American Society for Dermatologic Surgery; DASIL: Dermatologic and Aesthetic Surgery International League; USA: United States of America; JIPMER: Jawaharlal Institute of Postgraduate Medical Education and Research; IADVL: Indian Association of Dermatologists, Venereologists and Leprologists; ACS(I): Association of Cutaneous Surgeons of India; *general hair disorders observership, also focuses on procedures to treat alopecia; **general dermatology observership with significant focus on dermatosurgery; ***general dermatology observership with significant focus on dermatosurgery, but no hands-on experience
Not many formal training opportunities in this sub-division of dermatology are available in India and dermatologists depend on short-term training programmes and observerships, and live and cadaveric workshops in conferences, which cannot be considered as adequate training for a specialty involving invasive procedures. Under the Indian Association of Dermatologists, Venereologists and Leprologists, fellowship programmes in procedural or cosmetic dermatology for 1-3 months are offered every year and receive a large number of applications. The Association of Cutaneous Surgeons of India offers observerships in dermatologic surgery and aesthetics for 2-4 weeks in eight cities biannually for its members.49 The universities/institutes offering fellowships/observerships in dermatologic surgery or aesthetics are also summarised in Table 3.45,49,73-93 Qualified dermatologists from India and other countries are eligible for the international fellowships and training programmes mentioned in Table 3.
The unmet need
The extent of the unmet need
There is a great unmet need for procedural dermatologists globally. The extent of unmet need for conventional dermatologic surgery can be gauged by the data from the waiting list of a tertiary centre that performs these procedures frequently and at a low cost. Five minor procedural dermatology operation theatres run five days a week at All India Institute of Medical Sciences, New Delhi, India, with an average of 86 conventional dermatological surgeries, 372 minimally invasive procedures, 402 device-based interventions and 287 skin biopsies carried out per month in the year 2019. In a retrospective analysis of records (authors’ unpublished data), the waiting period was 8.5 months for various lasers, 3.5 months for vitiligo surgeries, five months for fat grafting, three months for scar revisions and 1.75 months for radiofrequency ablation or sclerotherapy for vascular malformations. Even excision of skin cancers had a waiting period of 1.25 months despite trying to accommodate patients at the earliest possible date.
Many conventional dermatologic surgeries require specialised skills that are frequently not available even in dermatology departments of tertiary care hospitals. Procedural dermatologists or plastic surgeons are best suited to perform them, but they are frequently done by general surgeons and other specialists entailing inappropriate, incomplete or excessive revisions with poor cosmetic outcomes. In the authors’ experience, many patients with stable vitiligo and volume defects who are suitable candidates for phototherapy/cellular grafting and volume restoration surgeries respectively, are never offered these modalities despite many years of treatment in many government hospitals due to lack of availability. In developing nations where the majority of the population depends on socialised medicine and welfare systems, patients with these conditions stand virtually abandoned.
The unmet need for cosmetic procedures
The World Health Organization defines Health as “a state of complete physical, mental and social well-being and not merely the absence of disease and infirmity.”50 This implies that ideally, to be healthy, patients must be free of mental and social distress which results from diseases leading to disfigurement. The lack of beauty and attractiveness is associated with a significant social disadvantage and a ‘beauty premium’.51,52 Skin aging is also considered a disease by many experts.53 Cosmetic manifestations of aging like androgenetic alopecia lead to significant distress and loss of social advantage.54 Conventional surgeries for androgenetic alopecia, minimally invasive cosmetic procedures for reversing skin aging, and liposuction for various indications can improve quality of life and body image and reduce psychological distress and anxiety.55-57
Despite the huge demand and benefits, the so-called ‘cosmetic’ minimally invasive procedures are frowned upon in academic settings. In the authors’ experience, Indian tertiary government hospitals have limited expertise in cosmetic procedures for aging and rejuvenation, and only a few minimally invasive procedures to treat benign growths or symptomatic diseases are carried out. The alleviation of impact on quality of life due to aging is not considered a priority in resource-limited settings. The majority of these procedures are uninsured and are done in private set-ups for the affording segment of the population. Even if people with limited economic means have a high willingness to pay for these procedures, their aesthetic and perceived social concerns are paternalistically disregarded by many dermatologists. This perpetuates social disparities due to economic disparities. Aesthetic socialism dictates that everyone should have the opportunity to enhance or restore beauty where it is lacking or when it is lost due to disease, trauma or aging.51
Limited training
Due to the limited number of specialists and centres providing training in various conventional surgeries and procedures, there is a large unmet need for training opportunities.
Some medical institutions in India do train residents in procedural dermatology, but the training needs to be standardised, formalised and modularised, and research be included as a component of the training. In an online survey of 103 dermatologists trained in India and practicing across the world, 59% felt that greater exposure to cosmetic and procedural dermatology was required to improve the training programme (authors’ unpublished data).
There are significant differences between the dermatology residency training programmes in India and internationally. The Indian residency programme is three years long, akin to other specialties, whereas, the length of dermatology residency is 3-4 years in the USA,58 four years in the UK59 and Australia60 and five years in Ireland.61 Procedural dermatology training in the US incorporates dedicated hours in the first, second and third years of residency.62 The residents need to maintain a detailed logbook or portfolio for supervised and independently done procedures in these countries.59,61 A minimum number for each procedure is required to be eligible for the final qualification.61 Third-year dermatology residents in the US are expected to perform procedures independently and also train other trainee doctors in these techniques.62 In India, this level of autonomy and independence is hard to achieve due to limited training, but efforts are underway. Recently All India Institute of Medical Sciences, New Delhi incorporated live supervised procedures on patients by the examinees as part of the final MD (Dermatology and Venereology) practical exam. This can be replicated in other institutions in a phased manner as the training level improves. Most large institutions in the USA have about one-third of their 25-30 board-certified faculty focusing nearly entirely on procedural dermatology,63 with dermatologic surgery sessions happening both pre-noon and afternoon five days a week.
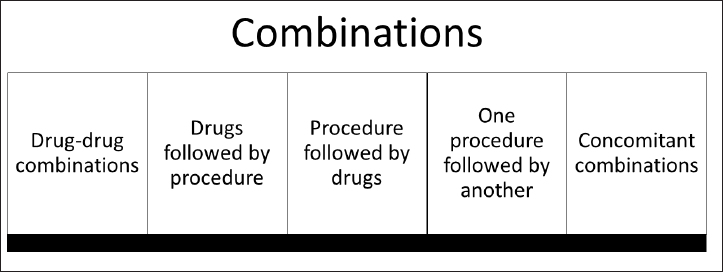
The unmet need for research
There is a significant lack of evidence-based guidelines and consensus for the procedural treatment of various dermatological diseases. For example, while surgical excision is the definitive and potentially curative treatment for hidradenitis suppurativa, there is no definite recommendation on surgical modalities in the Cochrane review of its treatment, as good-quality controlled studies are lacking.64 The same is the case for procedural management of post-acne scars.65 It is difficult to perform controlled studies in surgical procedures, and even well-conducted studies are downgraded when compiling evidence due to the lack of a sham surgery control. Individuals and centres treat patients based on individual preference, training and availability.66 Similarly, there is a lack of standardisation of platelet-rich plasma protocols for various indications. Many procedures have different risk-benefit ratios or procedural parameters in the skin of colour, while most published research originates in fairer skin types.65 Amongst the public as well as in academic circles, there is a perception that aesthetic procedures are more commerce-driven than based on sound scientific research and principles. This is because high-quality research is lacking for many cosmetic procedures and devices.
Pioneer tertiary research centres must encourage research studies in procedural dermatology to generate more evidence about the benefit of various procedures and combinations, their adaptability to low resource settings and the standardisation of various techniques. This will encourage more dermatologists to practice procedures and more medical institutions and national boards to add them to their residency training curriculum.
Unqualified practitioners and complications
The rapid rise in demand for procedural dermatology has not been paralleled with a proportionate increase in trained personnel or the establishment of treatment guidelines or quality control methods. There are no National Medical Commission of India guidelines on minimal qualifications required to perform these procedures, unlike in some other countries, like Singapore.42 This has resulted in unsupervised procedures done by untrained and unqualified practitioners often resulting in serious potential consequences. Many of these procedures warrant the application of sound scientific principles on a background of detailed knowledge of the anatomy and physiology of the skin; they also require standard operating protocols with emphasis on asepsis.
The majority of practitioners of medical aesthetics in China are illegal.67 There were 28 lawsuits of severe injuries due to elective cosmetic procedures by untrained individuals from the USA in a single year (2013). Out of these 28 cases, 25% had resulted in death and a further 50% required hospitalisation.68 The majority of laser surgery lawsuits involved non-physician operators.69 Exhaustive data are lacking, and these figures likely represent the tip of the iceberg.70
The Centers for Disease Control and Prevention, USA released a warning in 2008 regarding unlicensed cosmetic procedures when three women suffered acute renal failure after being injected with unlicensed liquid silicone products.71 The Singapore Medical Council subsequently introduced guidelines on the practice of aesthetic procedures for Singapore medical practitioners,42 and England’s Department of Health also launched a similar campaign to tackle ‘botched’ cosmetic procedures in 2019.72
Conclusion
There is a rising unmet need for various dermatologic procedures, and consequently, a growing demand for more procedural dermatologists, hands-on training programmes as well as research in procedural dermatology. The residency programme in dermatology needs to incorporate formal training in procedures, and maintenance of logbook records of procedures assisted and performed independently by trainees during residency. Organisations and associations such as the Indian Association of Dermatologists, Venereologists and Leprologists, Dermatologic and Aesthetic Surgery International League, Association of Cutaneous Surgeons of India and American Society for Dermatologic Surgery should facilitate actual hands-on training opportunities to dermatologists, rather than just observership programmes. The practice of cosmetic procedures should be based on sound scientific principles and unbiased evidence. Individual institutional and broad policy directives must be undertaken to address this gap.
Declaration of patient consent
Patient’s consent is not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Available from: https://www.asds.net/skin-experts/dermatologic-surgery [Cited 2022 Jan 20]
- Procedural Fellowship. Available from: https://www.med.unc.edu/derm/medical-education/postdoctoral-training/procedural-fellowship/ [Cited 2022 Mar 12]
- [Google Scholar]
- History of dermatologic surgery. From the beginnings to late antiquity. Clin Dermatol. 1987;5:1-10.
- [CrossRef] [PubMed] [Google Scholar]
- Sushruta: Father of plastic surgery. Ann Plast Surg. 2014;73:2-7.
- [CrossRef] [PubMed] [Google Scholar]
- A history of dermatologic surgery in the United States. Dermatol Surg. 2000;26:5-11.
- [CrossRef] [PubMed] [Google Scholar]
- Practice points from Prof. Lawrence M. Field-father of modern dermatosurgery: Bi-level anesthesia and blunt dissection. J Cutan Aesthet Surg. 2021;14:359-61.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- ACS(I) History. Available from: https://www.acsinet.net/about3/ [Cited 2022 Mar 16]
- [Google Scholar]
- The rise of chemical peeling in 19th-century European dermatology: Emergence of agents, formulations and treatments. J Eur Acad Dermatol Venereol. 2020;34:1890-9.
- [CrossRef] [PubMed] [Google Scholar]
- The history of cryosurgery. J R Soc Med. 2001;94:196-201.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Tissue grafts in vitiligo surgery—Past, present, and future. Indian J Dermatol. 2009;54:150-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Autografts in alopecias and other selected dermatological conditions. Ann N Y Acad Sci. 1959;83:463-79.
- [CrossRef] [PubMed] [Google Scholar]
- History of the clinical use of botulinum toxin A and B. Clin Dermatol. 2003;21:469-72.
- [CrossRef] [PubMed] [Google Scholar]
- A journey through liposuction and liposculture: Review. Ann Med Surg. 2017;24:53-60.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Electrosurgery: History, principles, and current and future uses. J Am Coll Surg. 2006;202:520-30.
- [CrossRef] [PubMed] [Google Scholar]
- Dermatologists perform more reconstructive surgery in the Medicare population than any other specialist group: A cross-sectional individual-level analysis of Medicare volume and specialist type in cutaneous and reconstructive surgery. J Am Acad Dermatol. 2018;78:171-3.e1.
- [CrossRef] [PubMed] [Google Scholar]
- Who should carry out skin cancer excisions? A systematic review. J Cutan Aesthetic Surg. 2019;12:153-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Expert consensus on the management of Androgenetic Alopecia in India. Int J Trichology. 2019;11:101-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Medical management of melasma: A review with consensus recommendations by Indian Pigmentary Expert Group. Indian J Dermatol. 2017;62:558-77.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Efficacy of the ruby laser in the treatment of Ota’s nevus previously treated using other therapeutic modalities. Plast Reconstr Surg. 1998;102:2352-7.
- [CrossRef] [PubMed] [Google Scholar]
- American Academy of Dermatology Issues New Guidelines for Treatment of Nonmelanoma Skin Cancer. Available from: https://www.aad.org/news/guidelines-to-treat-nonmelanoma-skin-cancer [Cited 2022 Mar 16]
- [Google Scholar]
- Lupus erythematosus panniculitis-induced facial atrophy: Effective treatment with poly-L-lactic acid and hyaluronic acid dermal fillers. J Am Acad Dermatol. 2013;69:e260-2.
- [CrossRef] [PubMed] [Google Scholar]
- Hand atrophy in a leprosy patient—Treatment with polymethylmethacrylate. Lepr Rev. 2010;81:216-20.
- [CrossRef] [PubMed] [Google Scholar]
- Persistence of hyaluronic acid filler for subcutaneous atrophy in a case of circumscribed scleroderma. J Cutan Aesthet Surg. 2015;8:69-71.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Standard guidelines of care: Keloids and hypertrophic scars. Indian J Dermatol Venereol Leprol. 2011;77:94-100.
- [CrossRef] [PubMed] [Google Scholar]
- Chromoblastomycosis. Postepy Dermatol Alergol. 2014;31:310-21.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Patient satisfaction and quality of life following surgery for hidradenitis suppurativa. Dermatol Surg. 2017;43:125-33.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term results of wide surgical excision in 106 patients with hidradenitis suppurativa. Dermatol Surg. 2000;26:638-43.
- [CrossRef] [PubMed] [Google Scholar]
- ISAPS Global Statistics. Available from: https://www.isaps.org/wp-content/uploads/2021/12/2020-Press-release-final.pdf [Cited 2022 Feb 26]
- [Google Scholar]
- Hair Transplant Market Size By Method (Follicular Unit Extraction [FUE], Follicular Unit Transplantation [FUT]), By Product (Gel, Serum, Drugs Finasteride, Minoxidil, Multivitamins), By Therapy (Platelet Rich Plasma, Stem Cell Therapy, Laser Therapy), By Gender (Male, Female), By Service Provider (Hospitals, Clinics, Surgical Centers), Industry Analysis Report, Regional Outlook, Application Potential, Price Trends, Competitive Market Share & Forecast, 2020-2026. Available from: https://www.gminsights.com/industry-analysis/hair-transplant-market [Cited 2022 Feb 26]
- [Google Scholar]
- India, A Potential Market for Hair Restoration Services: Survey. The Hindu; December 25, 2013
- [Google Scholar]
- Allergan Eyes Middle Class to Boost Botox Sales in Indian Market. Business Insider; August 15, 2018. Available from: https://www.business-standard.com/article/companies/allergan-eyes-middle-class-to-boost-botox-sales-in-indian-market-118081401543_1.html
- [Google Scholar]
- India Medical Aesthetic Devices Market—Growth, Trends, COVID-19 Impact, and Forecasts (2022-2027) Available from: https://www.mordorintelligence.com/industry-reports/india-aesthetic-devices-market [Cited 2022 Feb 26]
- [Google Scholar]
- ASDS Survey on Dermatologic Procedures. Available from: https://www.asds.net/medical-professionals/practice-resources/asds-survey-on-dermatologic-procedures [Cited 2022 Feb 26]
- [Google Scholar]
- ISAPS Global Statistics. Available from: https://www.isaps.org/wp-content/uploads/2020/12/Global-Survey-2019.pdf [Cited 2022 Feb 26]
- [Google Scholar]
- American Society of Plastic Surgeons Unveils COVID-19’s Impact and Pent-up Patient Demand Fueling the Industry’s Current Post-pandemic Boom. Available from: https://www.plasticsurgery.org/news/press-releases/american-society-of-plastic-surgeons-unveils-covid19s-impact-and-pent-up-patient-demand-fueling-the-industrys-current-post-pandemic-booms [Cited 2022 Feb 26]
- [Google Scholar]
- Aesthet Surg J. 2021;41:1-16.
- [CrossRef] [PubMed]
- ISAPS Global Survey Results 2020. Available from: https://www.isaps.org/medical-professionals/isaps-global-statistics/ [Cited 2022 Feb 26]
- [Google Scholar]
- Physical attractiveness and the accumulation of social and human capital in adolescence and young adulthood: Assets and distractions. Monogr Soc Res Child Dev. 2013;78:1-137.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Appearance discrimination, lookism and lookphobia in the workplace. J Appl Bus Res. 2012;28:791-802.
- [CrossRef] [Google Scholar]
- The need for evidence-based aesthetic dermatology practice. J Cutan Aesthet Surg. 2009;2:65-71.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Cosmetic Dermatologic Surgery Fellowship Accreditation Program. Available from: https://www.asds.net/medical-professionals/education/cosmetic-dermatologic-surgery-fellowship [Cited 2022 Feb 5]
- [Google Scholar]
- International Dermatologic Surgery Fellowship Recognition Program. Available from: https://www.asds.net/medical-professionals/education/for-international-dermatologists/international-fellowship-recognition [Cited 2022 Feb 5]
- [Google Scholar]
- International Traveling Mentorship Program. Available from: https://www.asds.net/medical-professionals/education/for-international-dermatologists/international-traveling-mentorship-program [Cited 2022 Mar 7]
- [Google Scholar]
- Post-CCT Fellowship Opportunities. Available from: https://bsds.org.uk/s [Cited 2022 Feb 5]
- [Google Scholar]
- Mohs Fellowship. Available from: https://www.eadv.org/mohs-fellowship [Cited 2022 Feb 5]
- [Google Scholar]
- Becoming an ACD Approved Mohs Specialist. Available from: https://www.dermcoll.edu.au/for-fellows-and-trainees/continued-learning-cpd/mohs-surgery [Cited 2022 Feb 5]
- [Google Scholar]
- Training Observerships. Available from: https://www.acsinet.net/observership/ [Cited 2022 Mar 7]
- [Google Scholar]
- Chron World Health Organ. 1947;1:29-43.
- [PubMed]
- It is the cooperation, stupid! J Cutan Aesthet Surg. 2016;9:274-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Lonely, poor, and ugly? How cultural practices and forms of capital relate to physical unattractiveness. Cult Sociol. 2020;14:80-105.
- [CrossRef] [Google Scholar]
- The pathobiology of skin aging: New insights into an old dilemma. Am J Pathol. 2020;190:1356-69.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Quality of life assessment in male patients with androgenetic alopecia: Result of a prospective, multicenter study. Ann Dermatol. 2012;24:311-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Quality of life following aesthetic liposuction: A prospective outcome study. J Plast Reconstr Aesthet Surg. 2019;72:1363-72.
- [CrossRef] [PubMed] [Google Scholar]
- General quality of life of patients with acne vulgaris before and after performing selected cosmetological treatments. Patient Prefer Adherence. 2017;11:1357-61.
- [CrossRef] [PubMed] [Google Scholar]
- Make-up improves the quality of life of acne patients without aggravating acne eruptions during treatments. Eur J Dermatol. 2005;15:284-7.
- [PubMed] [Google Scholar]
- Residency Program. Available from: https://www.hopkinsmedicine.org/dermatology/education/residency/ [Cited 2022 Mar 16]
- [Google Scholar]
- Dermatology Training Curriculum Implementation August 2021. Available from: https://www.bad.org.uk/shared/get-file.ashx?itemtype=document&id=3522 [Cited 2022 Mar 16]
- [Google Scholar]
- Australian Medical Graduates (Becoming A Dermatologist) Available from: https://www.dermcoll.edu.au/for-health-professionals/becoming-a-dermatologist/australian-medical-graduates/ [Cited 2022 Mar 16]
- [Google Scholar]
- Higher Specialist Training in Dermatology. Available from: https://rcpi-live-cdn.s3.amazonaws.com/wp-content/uploads/2021/10/HST-Dermatology-Curriculum-2018-Printable-Version-1-2-1.pdf [Cited 2022 Mar 16]
- [Google Scholar]
- Dermatology Residency (Minnesota) Available from: https://college.mayo.edu/academics/residencies-and-fellowships/dermatology-residency-minnesota/curriculum/ [Cited 2022 Mar 16]
- [Google Scholar]
- Dermatology Residency (Minnesota) Available from: https://college.mayo.edu/academics/residencies-and-fellowships/dermatology-residency-minnesota/department-and-faculty/ [Cited 2022 Mar 16]
- [Google Scholar]
- Interventions for hidradenitis suppurativa: A Cochrane systematic review incorporating GRADE assessment of evidence quality. Br J Dermatol. 2016;174:970-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Evidence-based surgical management of post-acne scarring in skin of color. J Cutan Aesthet Surg. 2020;13:124-41.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A review and update of treatment options using the acne scar classification system. Dermatol Surg. 2019;45:411-22.
- [CrossRef] [PubMed] [Google Scholar]
- Health, Pharma & Medtech: Share of Non-licensed Medical Aesthetics Entities and Practitioners in China in 2019. Available from: https://www.statista.com/statistics/1150716/china-prevalence-of-non-licensed-medical-aesthetics-entities-and-practitioners/ [Cited 2022 Feb 26]
- [Google Scholar]
- Injuries attributable to cosmetic procedures performed by unlicensed individuals in the United States. J Clin Aesthet Dermatol. 2015;8:35-7.
- [PubMed] [PubMed Central] [Google Scholar]
- Causes of injury and litigation in cutaneous laser surgery: An update from 2012 to 2020. Dermatol Surg. 2022;48:315-9.
- [CrossRef] [PubMed] [Google Scholar]
- The Health Workforce in India—World Health Organization: Human Resources for Health Observer—Issue No. 16. Available from: http://www.who.int/hrh/resources/hwindia_health-obs16/en/
- [Google Scholar]
- Campaign to Tackle ‘Botched’ Cosmetic Procedures. BBC Victoria Derbyshire Programme; 2019. Available from: https://www.bbc.com/news/health-47967968#:~:text=A%20campaign%20to%20tackle%20%22botched,which%20has%20led%20to%20deaths [Cited 2022 Mar 12]
- [Google Scholar]
- International Preceptorship Program. Available from: https://www.asds.net/medical-professionals/education/for-international-dermatologists/international-preceptorship-program [Cited 2022 Feb 5]
- [Google Scholar]
- International Observership Program in Dermatology. Available from: https://med.nyu.edu/departments-institutes/dermatology/education/international-observership [Cited 2022 Mar 9]
- [Google Scholar]
- International Physician Observership Program. Available from: https://my.clevelandclinic.org/departments/international-medical-education/international-programs/physician-observer#overview-tab [Cited 2022 Mar 9]
- [Google Scholar]
- Outpatient Externship in Dermatology. Available from: https://www.md2bconnect.com/st-louis-dermatology [Cited 2022 Mar 9]
- [Google Scholar]
- International Dermatology Fellowship Program. Available from: https://school.wakehealth.edu/education-and-training/residencies-and-fellowships/international-dermatology-fellowship [Cited 2022 Mar 11]
- [Google Scholar]
- Clinical Hands On. Available from: https://www.nsc.com.sg/Professional-Education/Doctors-Attachment/Overseas/Pages/Clinical-Hands-On.aspx [Cited 2022 Mar 11]
- [Google Scholar]
- Department of Dermatology. Available from: http://www.snuh.org/upload/global/common/Dermatology.pdf [Cited 2022 Mar 9]
- [Google Scholar]
- Applying for Clinical Fellowship in Dermatologic Surgery. Available from: https://www2.si.mahidol.ac.th/siinttraining/course/single/clinical-fellowship-training-program-dermatologic-surgery [Cited 2022 Mar 9]
- [Google Scholar]
- Fellowship Programme. Available from: https://bmcribengaluru.karnataka.gov.in/english [Cited 2022 Feb 5]
- [Google Scholar]
- Fellowship. Available from: https://www.cutis.org.in/fellowship/ [Cited 2022 Feb 5]
- [Google Scholar]
- Fellowship Programmes for Post Graduates. Available from: https://stjohnsadmissions.in/fellowship-courses [Cited 2022 Feb 5]
- [Google Scholar]
- Training at the Venkat Center. Available from: https://www.venkatcenter.com/medical-training/ [Cited 2022 Feb 5]
- [Google Scholar]
- Fellowship Course in Basic Phototherapy and Lasers in Clinical Dermatology. Available from: https://www.muhs.ac.in/showfile.aspx?src1=https://intranet.muhs.ac.in/syllabus.aspx [Cited 2022 Feb 5]
- [Google Scholar]
- Fellowship in Cosmetology. Available from: http://www.dypatil.edu/fellowshipincosmetology/ [Cited 2022 Mar 12]
- [Google Scholar]
- The Postdoctoral Fellowship (PDF) Courses. Available from: https://jipmer.edu.in/department/dermatology-std/academic [Cited 2022 Feb 5]
- [Google Scholar]
- Prospectus Admissions 2021-2022. Available from: https://www.cmch-vellore.edu/sites/education/prospectus.pdf [Cited 2022 Feb 5]
- [Google Scholar]
- Announcement Inviting Applications for IADVL Training Course-2022. Available from: https://www.iadvl.org/announcements.php? AnnouncementId=61cbeb929f2d297dc95f28f2 [Cited 2022 Mar 7]
- [Google Scholar]
- IADVL Observership 2022. Available from: https://www.iadvl.org/announcements.php?AnnouncementId=6194b2c79f2d29200c2e6662 [Cited 2022 Mar 7]
- [Google Scholar]






