Translate this page into:
Proteus syndrome
2 Departments of Plastic Surgery, M. K. C. G. Medical College and Hospital, Berhampur-760 004, India
Correspondence Address:
Basanti Debi
Department of Skin and VD, M. K. C. G. Medical College and Hospital, Berhampur-760 004, Orissa
India
| How to cite this article: Debi B, Nayak S, Da RP, Acharjya B. Proteus syndrome. Indian J Dermatol Venereol Leprol 2005;71:357-359 |
Abstract
Proteus syndrome is a variable and complex disorder characterized by multifocal overgrowths affecting any tissue or structure of the body. We present a girl aged 3 years and 8 months with an epidermal nevus, port-wine stain, macrodactyly with gigantism of the feet, lymphohemagiomas and multiple lipomas.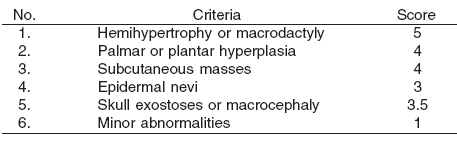
 |
 |
 |
 |
INTRODUCTION
Proteus syndrome was first identified by Michel Cohen in 1979 and named by Rudolf Wiedmann in 1983. It is a rare condition that can be loosely categorized as a hamartomatous disorder with great clinical variability. Major clinical findings include hemihypertrophy, symmetric megalodactyly, sub-cutaneous masses (vascular, lymphatic and lipomatous), epidermal nevi and skull hyperostosis. The disease was named after the Greek god Proteus in order to stress the polymorphic nature of the clinical presentation. Partial gigantism of a limb or digital overgrowth is pathognomonic with an unusual body habitus and often, cerebriform thickening of soles of feet.[1] We present a patient with this exceedingly rare disorder, estimated to affect 100-200 individuals worldwide and having a prevalence less than 1 per 1,000,000 live births.[1]
CASE REPORT
A girl aged 3 years and 8 months presented with enlargement of both feet with macrodactyly, swelling on the left side of the flank, a hyperpigmented nevus and multiple soft subcutaneous swellings over the chest and abdomen. There was no family history of a similar disorder. All lesions were present since birth. There was no history of epilepsy, mental retardation or consanguinity.
On examination, she had a flat, soft, velvety, hyperpigmented linear nevus along the entire right arm, extending to the neck and then downward parallel to the mid-spinal line [Figure - 1]. The nevus followed the lines of Blaschko. A bluish red plaque about 5 inches x 4 inches in size with an ill-defined border, studded with multiple, thick walled, light-to-dark colored vesicles, a few discharging serosanguineous fluid, was present on the left flank. Multiple, soft, ill-defined, non-tender subcutaneous masses were present on the chest and right posterolateral abdominal wall [Figure - 2]. There was gigantism of both feet, with macrodactyly and flaying of toes, and soft tissue overgrowth on both soles. A firm hypopigmented plaque, 1 cm x 1 cm in size, was present on the coccyx since birth. The hair, teeth and nails were normal.
Oral examination revealed no macroglossia or gum disorder. Cardiovascular and neurological examinations were normal.
Radiological examination revealed spina bifida at the level of L5-S1, with a sixth lumbar vertebra. X-rays of both feet were consistent with partial gigantism, macrodactyly and soft tissue hyperplasia of the sole.
Histopathology of the nevus showed mild hyperkeratosis, parakeratosis, acanthosis and papillomatosis, reflecting its epidermal nature. Histopathology of the left flank lesion was consistent with findings of a vascular malformation (lymphohemangioma).
CT scans of the abdomen were suggestive of multiple lipomas and vascular malformations, corresponding to masses on the chest, right posterolateral abdominal wall and left flank respectively. Ultrasonography of the pelvis and abdomen was normal.
DISCUSSION
Proteus syndrome is a disorder of mesodermal malformation. Its cause is not known.[2] There is no male or female predominance and all cases appear to be sporadic.[2],[3] It reflects mosaicism for a genetic mutation that is thought to be lethal in the non-mosaic state.[3] It is characterized by multifocal overgrowth affecting any tissue or structure of the body and its manifestations are polymorphous.
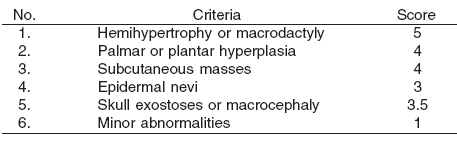
Our patient demonstrated most of the common features, like macrodactyly, gigantism, epidermal nevus, vascular malformations and lipomas. According to the scoring system devised by Hotamisligil in 1990[4] (with modifications by Darmstadt and Lane in 1994), our patient scored 16 points (13 or more points are required for diagnosis),[5] thus establishing the diagnosis.
Our patient also fulfilled the general and specific criteria for Proteus syndrome proposed by Biesecker et al.[5],[6] The findings of spina bifida occulta underlying a skin tag and an extra lumbar vertebra in our patient have not been described earlier in Proteus syndrome. [Table - 1]
The differential diagnosis includes Klippel-Trenaunay syndrome, Bannayan-Riley-Ruracalba and Maffucci syndrome, which were easily excluded on the basis of the distinctive clinical features of these disorders.[7]
The aim of treatment in Proteus syndrome is to minimize disability, and hence prompt attention should be paid to complications and early detection of potential problems so as to reduce the morbidity and mortality. A multidisciplinary approach involving plastic surgeons, orthopedic surgeons and physiotherapists was planned in our patient.
| 1. |
Pletcher BA. Proteus syndrome: http://www.emedicine.com/ped/topic1913.htm Last update 12-12-2003 Last accessed 04-09-04.
[Google Scholar]
|
| 2. |
Samalaska CP, Levin SW, James WD. Proteus syndrome. Arch Dermotol 1989;125:1109-14.
[Google Scholar]
|
| 3. |
Atherton DJ. Nevi and other developmental defects. In: Champion RH, Burton JL, Burns DA, editors. Rook/Wilkinson/Ebling Textbook of dermatology. 6th edn. Oxford: Blackwell Science; 1998. p. 222-6.
[Google Scholar]
|
| 4. |
Hotamisligil GS. Proteus syndrome and hamartosis with overgrowth. Dysmorph Clin Genet 1990:87-102.
[Google Scholar]
|
| 5. |
Bieskar LG, Happle R, Mulliken JB. Proteus syndrome: diagnostic criteria, differential diagnosis and patient correlation. Am J Med Gen 1999;84:389-95.
[Google Scholar]
|
| 6. |
Biesecker LG, The multifaceted challenges of proteus syndrome. JAMA 2001;285:2240-3.
[Google Scholar]
|
| 7. |
Bialer MG, Rieder MJ Banayan-Zonana syndrome: a problem in differential diagnosis. Eur J Pediatrics 1988;148:122-5.
[Google Scholar]
|
Fulltext Views
3,912
PDF downloads
3,371





