Translate this page into:
Pseudoxanthoma elasticum with cerebrovascular accident
2 Department of Dermatology and Venereology, Medical College Hospital, Trivandrum, Kerala, India
Correspondence Address:
G Nanda Kumar
Department of Pathology, Medical College Hospital, Trivandrum - 695 011, Kerala
India
| How to cite this article: Kumar G N, Ragi K V, Nair PS. Pseudoxanthoma elasticum with cerebrovascular accident. Indian J Dermatol Venereol Leprol 2007;73:191-193 |
Abstract
A 65-year-old male presented with right hemiparesis and skin lesions. On examination, the patient had multiple, discrete, skin-colored papules on the neck and upper chest with wrinkling of the skin. The lateral part of the trunk and medial aspect of both upper arms showed atrophic plaques. A computerized tomography scan of the head showed dilatation of the basilar artery with a frontoparietal infarct. Funduscopic examination showed characteristic angioid streaks. Skin biopsy of the papule and atrophic plaques showed epidermal atrophy, calcium deposits in the mid-dermis and basophilic clumped and fragmented elastic fibers in the mid- and lower dermis, all findings consistent with pseudoxanthoma elasticum. We are reporting here a case of pseudoxanthoma elasticum with cerebrovascular accident.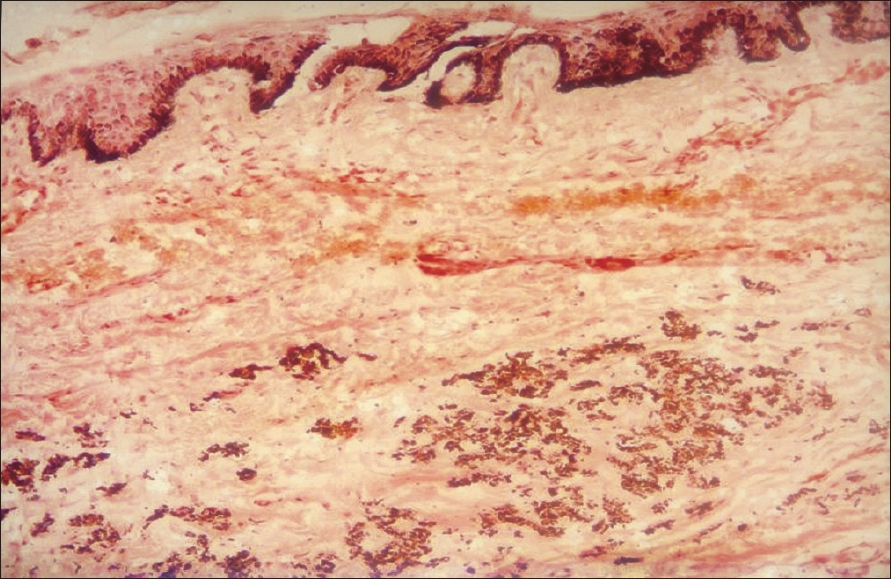 |
| Figure 5: Fragmented and clumped elastic fi bers in mid dermis, (Von Kossa stain, x400) |
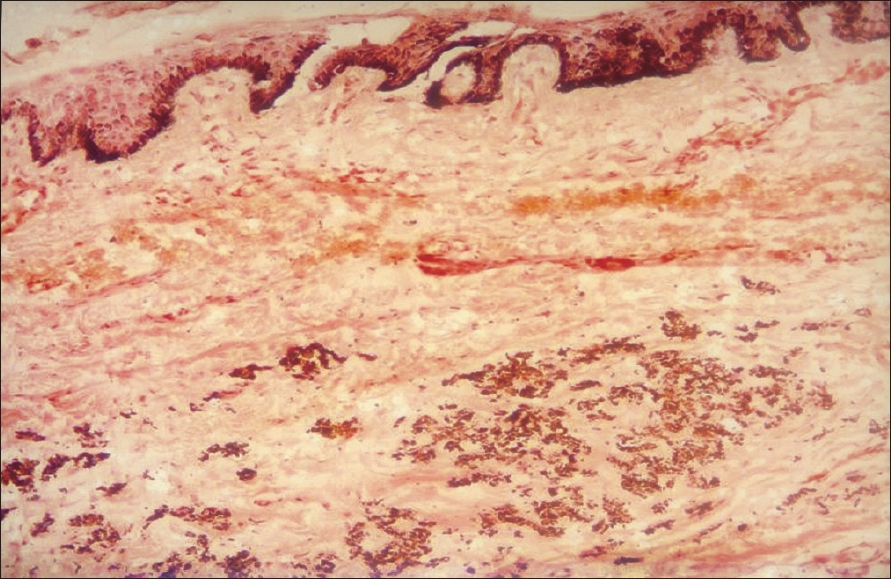 |
| Figure 5: Fragmented and clumped elastic fi bers in mid dermis, (Von Kossa stain, x400) |
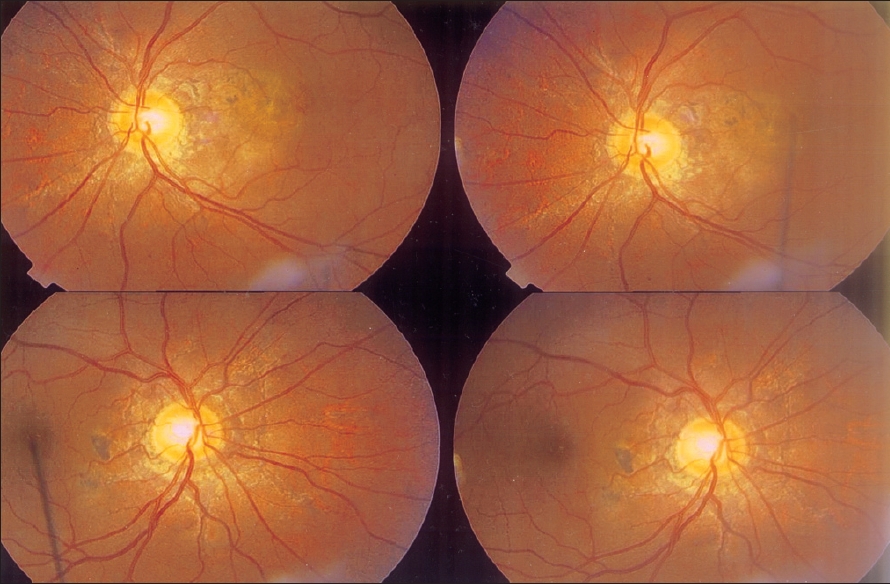 |
| Figure 4: Fundoscopic examination showing �angioid streaks� |
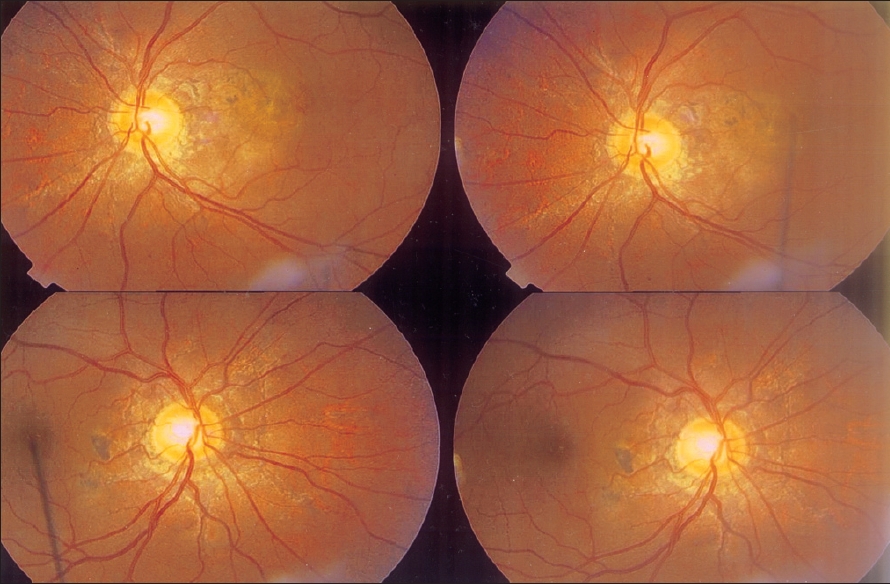 |
| Figure 4: Fundoscopic examination showing �angioid streaks� |
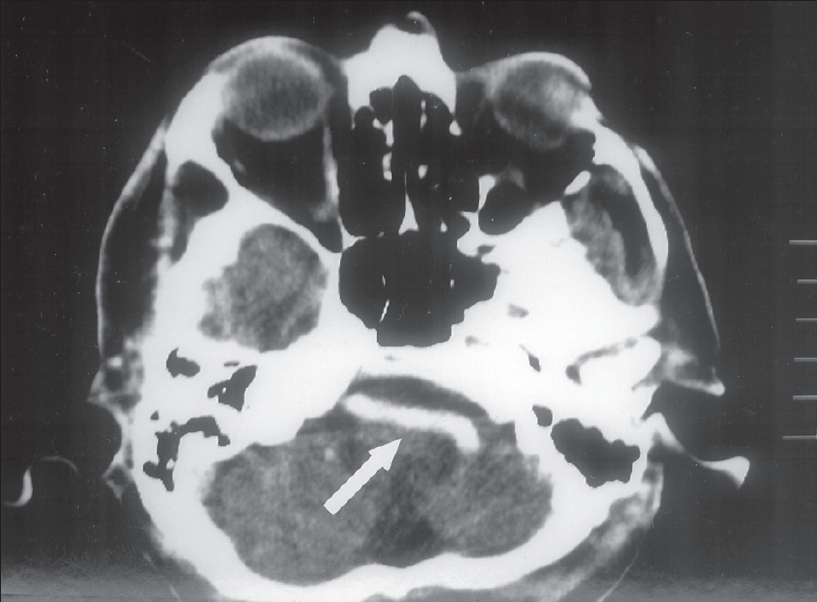 |
| Figure 3: CT-scan showing basilar artery dilatation (Arrow) |
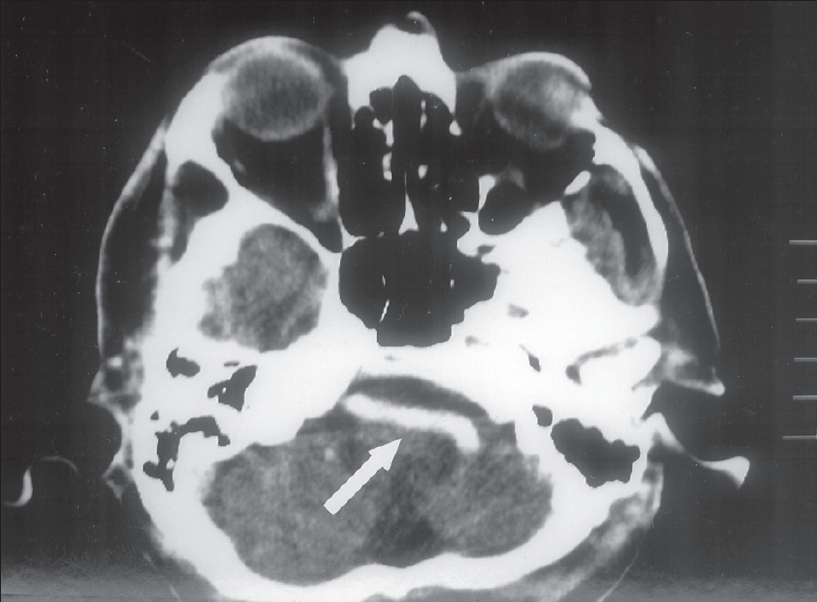 |
| Figure 3: CT-scan showing basilar artery dilatation (Arrow) |
 |
| Figure 2: Atrophic plaques on the upper arm |
 |
| Figure 2: Atrophic plaques on the upper arm |
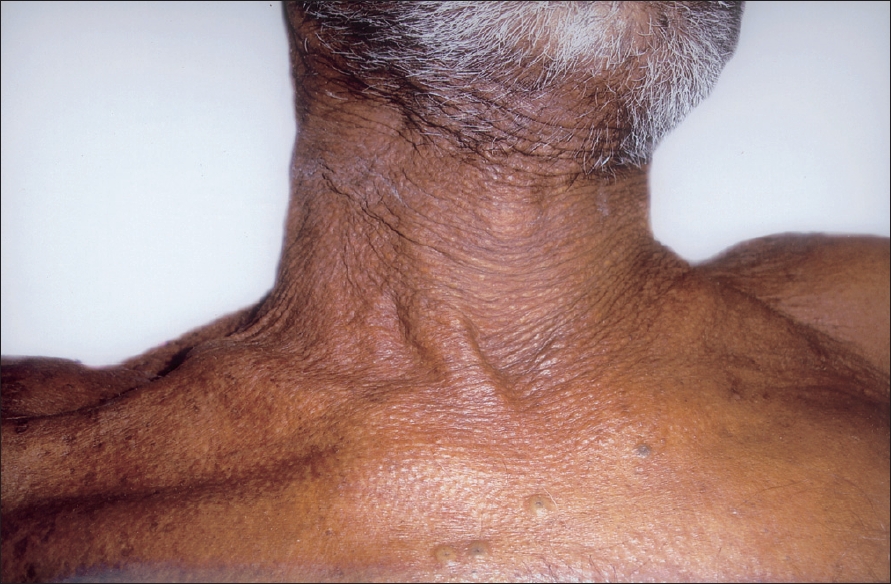 |
| Figure 1: Skin colored papules and wrinkling of skin of neck resembling �plucked chicken� |
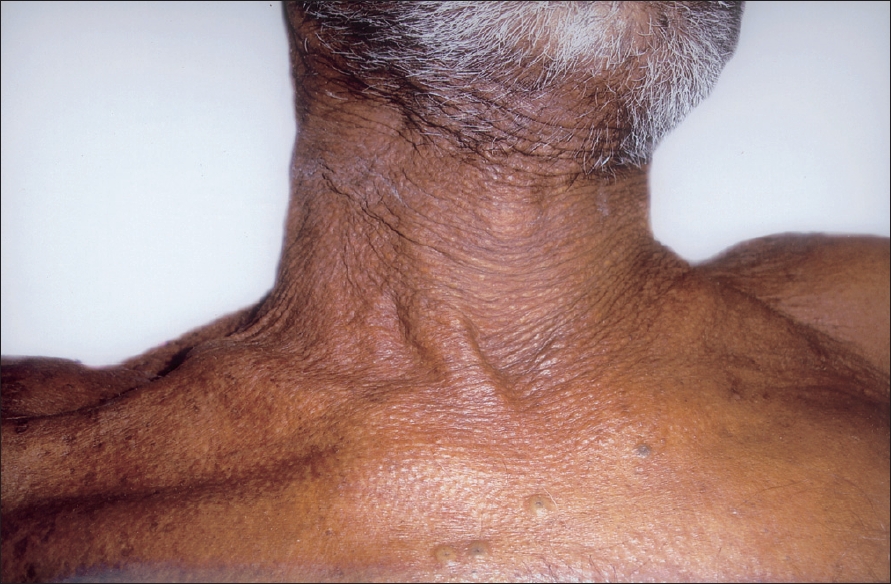 |
| Figure 1: Skin colored papules and wrinkling of skin of neck resembling �plucked chicken� |
Introduction
Pseudoxanthoma elasticum (PXE) also known as Gr φnblad-Strandberg syndrome or generalized elastorrhexis is an inherited disorder of the connective tissue mainly involving the elastic fibers of the dermis, eyes and cardiovascular system. Previously, there was a controversy regarding the mode of its transmission, but now it is thought to be exclusively autosomal recessive. [1] The defective gene has now been identified and localized in the chromosome 16p13.1. [2] This gene codes for an ATP-binding cassette transporter (ABCC6). It is postulated that mutation in this gene may affect the transport of anionic peptides, which in turn causes progressive calcification of the elastic fibers of the tissues. [2] Clinically the patient presents with skin-colored or yellowish papules on the neck, axilla and groin. The skin in these regions may hang in folds.
The papular lesions on the neck resemble a "cobblestone", "plucked chicken" or "Moroccan leather". Involvement of the elastic fibers of the Bruch membrane of the eye leads to characteristic "angioid streaks". Cardiovascular manifestations such as angina pectoris and myocardial infarction result from affected blood vessels of the heart and elastic fibers of the valves. Although cerebral vessels are rarely involved, involvement of the arteries of the legs may lead to intermittent claudication. We present a case of PXE with unusual cutaneous presentation and serious systemic manifestation.
Case Report
A 65-year-old man was admitted to the Medical casualty with loss of consciousness and skin lesions. History was obtained from a bystander. The patient did not have any history of hypertension, diabetes, cardiovascular or neurological disorder. The patient was not on any drugs and had the skin lesions for 45 years. There was no similar history in the family members nor was there any consanguinity. On examination, the patient had altered consciousness and plantar reflexes were upgoing. Neurological examination revealed a right hemiparesis. Dermatological examination showed multiple, discrete, skin-colored papules distributed on the neck and upper chest with wrinkling of the skin [Figure - 1].
A few acneiform papules were present on the front of the chest. The lateral part of the trunk and medial aspect of both upper arms showed multiple discrete and confluent atrophic plaques with peripheral hyperpigmentation [Figure - 2]. Oral and genital mucosa was normal. Routine hemogram, urine examination, liver and renal function tests were within normal limits. Serological tests for syphilis and human immunodeficiency virus (HIV) were negative. Chest X-ray and ultrasound of the abdomen were within normal limits. Electrocardiogram (ECG) and echocardiogram were normal. A Doppler scan of the lower limbs showed normal blood flow. CT-scan of the head showed basilar dolichoectasia-dilatation and thickening of the basilar artery with a frontoparietal infarct [Figure - 3]. No other arterial involvement was seen in the CT-scan. When the patient regained consciousness, a funduscopic examination showed characteristic "angioid streaks" [Figure - 4].
Skin biopsy from both the papular lesions on the neck and the atrophic plaques on the upper arms showed epidermal atrophy with calcium deposition in the mid-dermis. The mid- and lower dermis showed basophilic stained, clumped, swollen and fragmented elastic fibers. Von Kossa stain showed calcium deposits in the mid- and lower dermis. Elastic Van Gieson stain highlighted the clumped, swollen and fragmented elastic fibers in the mid- and lower dermis [Figure - 5]. Thus, the histopathology of both types of skin lesions was consistent with PXE. Taking into account the skin lesions, angioid streaks and CNS involvement, we made a final diagnosis of PXE with right hemiparesis. The patient was referred to the Neurology department for further management and is at present undergoing physiotherapy.
Discussion
In the present case, the neck lesions were suggestive of PXE; atrophic plaques with peripheral hyperpigmentation are not described in classical cases of PXE. However, the histopathology of both lesions was consistent with PXE. Atrophic, grooved, fissured and verrucous lesions have been described in perforating PXE. [3] Histologically, perforating PXE shows channels and tunnels in the epidermis through which altered elastic fibers are extruded. [4] Even though atrophic plaques are rare in PXE, unusual presentation in the form of acneform lesions, granulomatous and reticulate pigmentation have been described in literature. [5] D-penicillamine-induced PXE with elastosis perforans serpiginosa has been reported. [6]
Involvement of the cerebral arteries is rare in PXE and involvement of the basilar artery as seen in our case is even rarer. [7] Involvement of the pulmonary, renal and mitral valve prolapse has been reported, but investigations in our case did not show any involvement. [8] A study of PXE cases in the Indian subcontinent showed that skin lesions and eye involvement are common but systemic involvement is relatively rare. [9] Lebwohl et al . have devised diagnostic criteria for PXE based on the skin lesions, histopathological changes and angioid streaks. [8]
In addition to angioid streaks, drusen and yellowish mottling of the posterior pole are other ocular findings. [7],[9] Hypertension, aneurysmal dilatation and coronary occlusion are the other cardiovascular findings. Increased risk of miscarriage, mild hypercalcemia and abnormalities of vitamin D metabolism are also reported in PXE. There is no specific treatment for PXE. Laser coagulation may prevent further retinal damage. Dietary restriction of calcium and phosphorus may be advised to the patient. Plastic surgery of the skin lesions may benefit the patient. We are reporting this case to highlight this unusual cutaneous manifestation of atrophic plaques in PXE with the rare presentation of cerebrovascular accident.
| 1. |
Pope FM. Historical evidence for the genetic heterogeneity of pseudoxanthoma elasticum. Br J Dermatol 1975;92:493-509.
[Google Scholar]
|
| 2. |
Ringfeil F, Pulkkinen L, Uitto J. Molecular genetics of pseudoxanthoma elasticum. Exp Dermatol 2001;10:221-8.
[Google Scholar]
|
| 3. |
Kazakis AM, Parish WR. Periumblical perforating pseudoxanthoma elasticum. J Am Acad Dermatol 1988;19:384-8.
[Google Scholar]
|
| 4. |
Hicks J, Carpenter CL Jr, Reed PJ. Periumblical perforating pseudoxanthoma elasticum. Arch Dermatol 1979;115:300-3.
[Google Scholar]
|
| 5. |
Hartman A, Hartman-Visser SR. Pseudoxanthoma elasticum with extensive comedone formation. Dermatologica 1977;154:318-9.
[Google Scholar]
|
| 6. |
Rath N, Bhardwaj A, Kar HK, Sharma PK, Bhardwaj M, Bharija SC. Penicillamine induced pseudoxanthoma elasticum with elastosis perforans serpiginosa. Indian J Dermato Venereol Leprol 2005;71:182-5.
[Google Scholar]
|
| 7. |
Inamadar AC, Palit A. Pseudoxanthoma elasticum. Postgrad Med J 2004;80;297-9.
[Google Scholar]
|
| 8. |
Lebwohl MJ, Distefano D, Prioleau PG, Uram M, Yannuzzi LA, Fleischmajer R. Pseudoxanthoma elasticum and mitral valve prolapse. N Engl J Med 1982;307:228-31.
[Google Scholar]
|
| 9. |
Sehgal N, Singh M, Sharma AK, Nayyar M, Saxena HM. Pseudoxanthoma elasticum in the Indian Sub-continent. Indian J Dermatol Venereol Leprol 1979;45:290-3.
[Google Scholar]
|
Fulltext Views
2,741
PDF downloads
1,244





