Translate this page into:
Psoriasis and risk of incident atrial fibrillation: A systematic review and meta-analysis
2 Department of Internal Medicine, Division of Pulmonology and Critical Care Medicine, Mayo Clinic, Rochester, MN, USA
3 Department of Internal Medicine, Division of Nephrology and Hypertension, Mayo Clinic, Rochester, MN, USA
Correspondence Address:
Patompong Ungprasert
Division of Rheumatology, Mayo Clinic, 200 First Street SW, Rochester, MN 55905, USA
| How to cite this article: Ungprasert P, Srivali N, Kittanamongkolchai W. Psoriasis and risk of incident atrial fibrillation: A systematic review and meta-analysis. Indian J Dermatol Venereol Leprol 2016;82:489-497 |
Abstract
Background and Objectives: Patients with psoriasis might have a higher risk of developing atrial fibrillation as a result of chronic inflammation. This study aimed to investigate this association by comprehensively reviewing all available evidence. Methods: We conducted a systematic review and meta-analysis of cohort studies that reported relative risk, hazard ratio, incidence ratio or standardized incidence ratio with 95% confidence intervals comparing the risk of incident atrial fibrillation in patients with psoriasis versus participants without psoriasis. Both retrospective and prospective cohort studies were eligible. Pooled risk ratio and 95% confidence intervals were calculated using random-effect, generic inverse variance methods of DerSimonian and Laird. Results: Three retrospective studies with 110,568 cases of psoriasis and 5,352,817 participants without psoriasis were included in this meta-analysis. The pooled risk ratio of subsequent development of atrial fibrillation in patients with psoriasis versus participants without psoriasis was 1.21 (95% confidence interval, 1.14–1.29). The statistical heterogeneity was low with an I2 of 29%. Limitations: Coding-based design of the primary studies that had limited accuracy. Conclusions: Our meta-analysis demonstrated a statistically significant increase in the risk of incident atrial fibrillation among patients with psoriasis.Introduction
Psoriasis is a chronic immune-mediated skin disorder characterized by hyperproliferation of keratinocytes. It is a common disease with an estimated prevalence of 2–4% in the adult population.[1] The etiology of psoriasis is unknown but is believed to be related to the interplay between genetic predisposition and acquired factors such as smoking, obesity and excessive alcohol consumption.[2],[3],[4] T helper 1 (Th1) and T helper 17 (Th17) lymphocytes are the major regulatory cells involved in the pathogenesis.[1]
Over the past decades, several epidemiologic studies have demonstrated a higher prevalence of co-morbidities among patients with psoriasis compared to the general population, especially metabolic syndrome and cardiovascular diseases.[5],[6],[7] Chronic inflammation is believed to play a pivotal role for this increased risk as several studies have illustrated the detrimental effect of oxidative stress and inflammatory cytokines on endothelial function resulting in accelerated atherosclerosis.[8],[9],[10],[11]
Patients with psoriasis might also be at an increased risk of developing atrial fibrillation as the chronic inflammatory state is also increasingly recognized as an independent risk factor for this arrhythmia.[12],[13],[14] Nevertheless, the number of epidemiologic studies addressing this association is still limited. Thus, to further investigate this possible relationship, we conducted a systematic review and meta-analysis of cohort studies that compared the risk of developing atrial fibrillation in patients with psoriasis with those who did not have psoriasis.
Methods
Search strategy
Two investigators (PU and NS) independently searched published articles indexed in the MEDLINE and EMBASE database from inception to September 2015 using the search strategy described in Supplementary Data 1. References of included studies and selected review articles were also manually searched.[SUPPORTING:1]
Inclusion criteria
The eligibility criteria included the following:
- Cohort study (prospective or retrospective) reporting incident atrial fibrillation, after the diagnosis of psoriasis for cases, and after the corresponding index date for controls
- Relative risk, hazard ratio, incidence ratio, or standardized incidence ratio with 95% confidence intervals or sufficient raw data for the calculation were provided and
- Participants without psoriasis were used as comparator.
Assessment of study eligibility was independently performed by the two aforementioned investigators. The search and literature review process were overseen by the senior investigator (WK) who served as the deciding vote for any difference in decisions between the first two investigators. Newcastle–Ottawa quality assessment scale was used to evaluate the quality of the included studies.[15] This scale assessed each study in three domains including (1) recruitment of the cohorts, (2) similarity and comparability between the cohorts and (3) ascertainment of outcomes of interest.
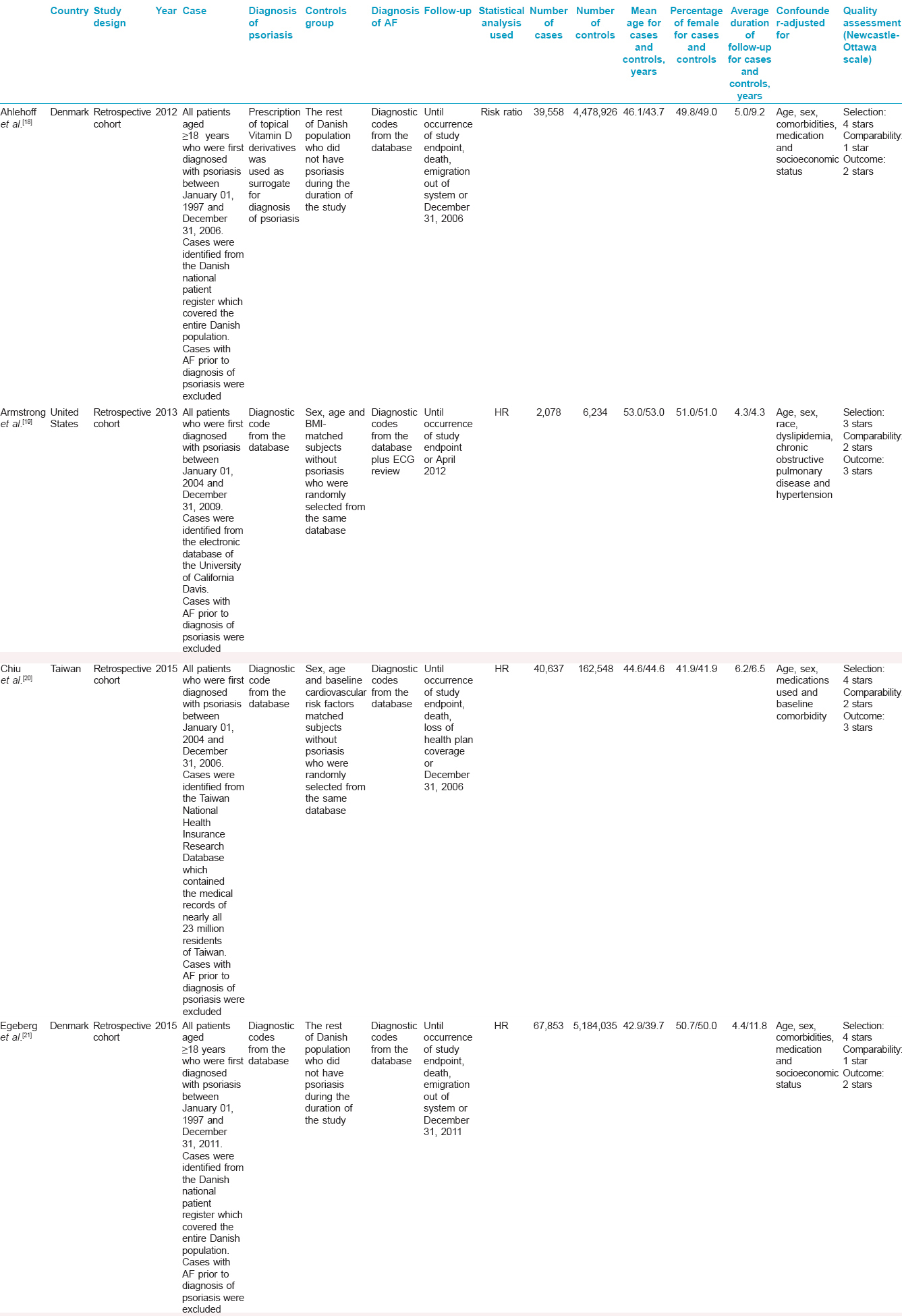
Data extraction
A standardized data collection form was used to extract the following information: first author's name, title of the study, year of publication, year of study, country of origin, study population, method used to identify cases and controls, method used to diagnose the outcome of interest (atrial fibrillation), number of participants, average duration of follow-up, mean age of participants, percentage of females in each cohort, confounders that were adjusted and adjusted effect estimates with 95% confidence interval.
To ensure the accuracy of the data extraction, all investigators independently performed this extraction. Any discrepancy was resolved by referring back to the original studies.
Statistical analysis
Data analysis was performed using Review Manager 5.3 software from the Cochrane Collaboration (London, United Kingdom). We pooled the point estimates from each study using the generic inverse-variance method of DerSimonian and Laird.[16] In light of the high likelihood of between-study variance, we used a random-effect model rather than a fixed-effect model. Cochran's Q-test which is complemented with the I2 statistic was used to assess statistical heterogeneity. This I2 statistic quantifies the proportion of total variation across studies that are due to heterogeneity rather than chance. A value of I2 of 0–25% represents insignificant heterogeneity, more than 25% but ≤50% low heterogeneity, more than 50% but ≤75% moderate heterogeneity and more than 75% high heterogeneity.[17]
Results
Our search strategy yielded 230 potentially relevant articles (177 articles from EMBASE and 53 articles from MEDLINE). After exclusion of 50 duplicated articles, 180 articles underwent title and abstract review. One hundred and sixty-six articles were excluded at this stage since they were not cohort studies, did not report the outcome of interest (incident atrial fibrillation) or were not conducted in patients with psoriasis, leaving 14 articles for full-length article review. Four studies were excluded as they were descriptive studies without comparators while six of them were excluded since they reported the prevalence of atrial fibrillation in psoriasis cohorts, not the incidence. Four retrospective cohort studies met our inclusion criteria.[18],[19],[20],[21] However, two studies from the same group of authors used the same database (Danish National Patient Register).[18],[21] To avoid patient duplication, the study by Ahlehoff et al. was included in this review but was excluded from the meta-analysis as the study by Egeberg et al. was more comprehensive and was conducted over a longer period of time.[18],[21] Therefore, three retrospective cohort studies with 110,568 cases of psoriasis and 5,352,817 controls were included in this meta-analysis. [Figure - 1] outlines the search and literature review process. The clinical characteristics and Newcastle–Ottawa scales of the included studies are described in [Table - 1]. It should be noted that the inter-rater agreement for quality assessment was high with the kappa statistic of 0.59.
 |
| Figure 1: Search methodology and literature review process |
All studies did reveal an increased risk of incident atrial fibrillation among patients with psoriasis, even though one study did not achieve statistical significance.[19] The pooled analysis demonstrated a statistically significant increased risk of development of incident atrial fibrillation in patients with psoriasis compared to participants without psoriasis, with the pooled risk ratio of 1.21 (95% confidence interval, 1.14–1.29). The individual risk ratios from each study were adjusted for age, sex and co-morbidities. The study by Chiu et al. and Egeberg et al. also adjusted for current medications.[20],[21] The statistical heterogeneity was low with an I2 of 29%. The crude incidence rate was provided in only one study which was 261.0 per person-year among cases and 202.7 per person-year among comparators.[20] Forest plot of this meta-analysis is shown in [Figure - 2].
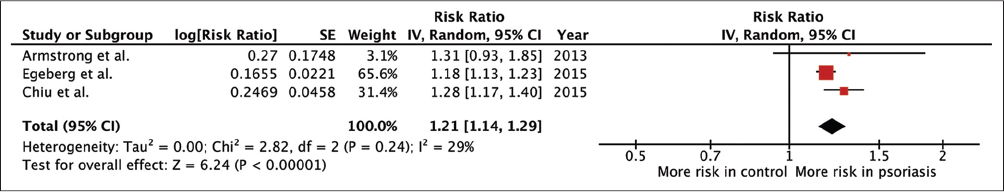 |
| Figure 2: Forest plot of this meta-analysis |
Evaluation for publication bias
Since only three studies were included in this meta-analysis, evaluation for publication bias was not performed.
Discussion
Cardiovascular disease is well recognized as one of the major co-morbidities of psoriasis. Previous studies have shown increased incidence of myocardial infarction, cerebrovascular accident and venous thromboembolism among these patients.[6],[22] However, the association between arrhythmia, specifically atrial fibrillation and psoriasis has not been comprehensively studied. This meta-analysis was conducted with the aim of shedding more light on this area. We were able to demonstrate a statistically significant 21% excess risk of incident atrial fibrillation among patients with psoriasis, as compared to trial participants without this disease.
The reasons for this increased risk remain unclear, clarification of which requires further investigation. However, there could be a few possible explanations:
- This association might just be the result of confounding, as smoking is an established risk factor for both psoriasis and atrial fibrillation.[2],[23] It has been shown that smoking induces an overproduction of oxidative stress and several cytokines including interleukin 1-beta and transforming growth factor alpha which are involved in the pathogenesis of psoriasis.[2],[24],[25] It is possible that the psoriasis cohorts might have included more smokers as compared to controls and thus, may have had a higher likelihood of developing atrial fibrillation. We are not able to adjust for the confounding effect of smoking as two out of three studies included in this meta-analysis did not have information on the smoking status of their participants.[20],[21] However, the third study (by Armstrong et al. did demonstrate that the frequency of smoking was not significantly different between the two groups (P = 0.2, although it did not adjust for the effect estimate for smoking either.)[19]
- As previously mentioned, coronary artery disease is more prevalent among patients with psoriasis compared with the general population.[5],[22] and since this is one of the strongest risk factors for atrial fibrillation, its higher prevalence might account for the increased risk of developing atrial fibrillation [23]
- Chronic inflammation from psoriasis could have a direct effect on initiation and continuation of atrial fibrillation. Histopathological studies of the atrium in patients with atrial fibrillation have revealed that infiltration of inflammatory cells and necrosis of cardiomyocytes are regularly seen.[26],[27] Epidemiological studies have also demonstrated higher levels of acute inflammatory markers including C-reactive protein, IL-1, IL-6 and tumor necrosis factor among patients with atrial fibrillation compared with those in sinus rhythm.[27],[28],[29],[30] The higher level of inflammatory markers is also associated with a lower success rate of cardioversion.[31] These pro-inflammatory cytokines, particularly tumor necrosis factor, have been shown to directly impact the atrial myocardium leading to structural and electrical remodeling through several mechanisms.[30],[32] Tumor necrosis factor activates the transforming growth factor-beta signaling pathway and increases the secretion of matrix metalloproteinases-2 and matrix metalloproteinases-9 from myofibroblasts which has been shown to mediate atrial structural remodeling in an animal model.[33] Platelet-derived growth factor-A which is synthesized and secreted by infiltrating mast cells promotes cell proliferation and collagen expression in cardiac fibroblasts and thus helps increase atrial fibrosis and structural remodeling.[34],[35]
Electrical remodeling is also signaled by tumor necrosis factor and platelet-derived growth factor-A. It has been shown that tumor necrosis factor could interfere with the calcium influx of pulmonary vein cardiomyocytes which could be arrhythmogenic.[36] Platelet-derived growth factor-A reduces the duration of action potential and calcium transients which is also pro-arrhythmic.[35] The combination of structural and electrical remodeling could well serve as the cornerstone for the development of atrial fibrillation.
It should be noted that depression may also play a role in the development of atrial fibrillation among those with psoriasis, as the study by Egeberg et al. found that patients with psoriasis who also had depression had a higher risk of incident atrial fibrillation compared to those without depression.[21]
The major strength of this study was that systematic review and meta-analysis comprehensively combined all available data resulting in a more accurate estimated risk. We were also able to provide a temporal relationship between psoriasis and atrial fibrillation, as we included only studies that compared the risk of incident atrial fibrillation after the diagnosis of psoriasis.
Nevertheless, the study has some limitations as detailed below, and we acknowledge that the results should be interpreted with caution.
- All the included studies were conducted using coding-based medical registry which carried the risk of coding inaccuracy. The study by Armstrong et al. was the only study that verified the diagnosis of atrial fibrillation with a review of the electrocardiogram [19]
- We could not perform an evaluation for publication bias either, because the number of the included studies was too low. Therefore, we cannot exclude a possibility of publication bias in favor of positive studies
- Moreover, this study was a meta-analysis of observational studies that could only establish an association but not causality
- The possibility of detection bias also could not be excluded as patients with psoriasis might have more physician visits and thus have laboratory investigations performed more frequently leading to a higher likelihood of detection of atrial fibrillation.
Conclusions
Our meta-analysis demonstrated a statistically significant increased risk of incident atrial fibrillation among patients with psoriasis. Further studies are required to clarify how this risk should be addressed in clinical practice.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Christophers E. Psoriasis – Epidemiology and clinical spectrum. Clin Exp Dermatol 2001;26:314-20.
[Google Scholar]
|
| 2. |
Armstrong AW, Harskamp CT, Dhillon JS, Armstrong EJ. Psoriasis and smoking: A systematic review and meta-analysis. Br J Dermatol 2014;170:304-14.
[Google Scholar]
|
| 3. |
Duffy DL, Spelman LS, Martin NG. Psoriasis in Australian twins. J Am Acad Dermatol 1993;29:428-34.
[Google Scholar]
|
| 4. |
Correia B, Torres T. Obesity: A key component of psoriasis. Acta Biomed 2015;86:121-9.
[Google Scholar]
|
| 5. |
Kokpol C, Aekplakorn W, Rajatanavin N. Prevalence and characteristics of metabolic syndrome in South-East Asian psoriatic patients: A case-control study. J Dermatol 2014;41:898-902.
[Google Scholar]
|
| 6. |
Ungprasert P, Sanguankeo A, Upala S, Suksaranjit P. Psoriasis and risk of venous thromboembolism: A systematic review and meta-analysis. QJM 2014;107:793-7.
[Google Scholar]
|
| 7. |
Ungprasert P, Srivali N, Thongprayoon C. Association between psoriasis and chronic obstructive pulmonary disease: A systematic review and meta-analysis. J Dermatolog Treat 2016;27:316-21.
[Google Scholar]
|
| 8. |
Libby P. Inflammation in atherosclerosis. Nature 2002;420:868-74.
[Google Scholar]
|
| 9. |
Maradit-Kremers H, Nicola PJ, Crowson CS, Ballman KV, Gabriel SE. Cardiovascular death in rheumatoid arthritis: A population-based study. Arthritis Rheum 2005;52:722-32.
[Google Scholar]
|
| 10. |
Ungprasert P, Charoenpong P, Ratanasrimetha P, Thongprayoon C, Cheungpasitporn W, Suksaranjit P. Risk of coronary artery disease in patients with systemic sclerosis: A systematic review and meta-analysis. Clin Rheumatol 2014;33:1099-104.
[Google Scholar]
|
| 11. |
Ungprasert P, Suksaranjit P, Spanuchart I, Leeaphorn N, Permpalung N. Risk of coronary artery disease in patients with idiopathic inflammatory myopathies: A systematic review and meta-analysis of observational studies. Semin Arthritis Rheum 2014;44:63-7.
[Google Scholar]
|
| 12. |
Engelmann MD, Svendsen JH. Inflammation in the genesis and perpetuation of atrial fibrillation. Eur Heart J 2005;26:2083-92.
[Google Scholar]
|
| 13. |
Kim SC, Liu J, Solomon DH. The risk of atrial fibrillation in patients with rheumatoid arthritis. Ann Rheum Dis 2014;73:1091-5.
[Google Scholar]
|
| 14. |
Bacani AK, Crowson CS, Roger VL, Gabriel SE, Matteson EL. Increased incidence of atrial fibrillation in patients with rheumatoid arthritis. Biomed Res Int 2015;2015:809514.
[Google Scholar]
|
| 15. |
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010;25:603-5.
[Google Scholar]
|
| 16. |
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177-88.
[Google Scholar]
|
| 17. |
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60.
[Google Scholar]
|
| 18. |
Ahlehoff O, Gislason GH, Jørgensen CH, Lindhardsen J, Charlot M, Olesen JB, et al. Psoriasis and risk of atrial fibrillation and ischaemic stroke: A Danish nationwide cohort study. Eur Heart J 2012;33:2054-64.
[Google Scholar]
|
| 19. |
Armstrong AW, Azizi S, Wu J, Harskamp CT, Farrow J, Johnson MA, et al. Psoriasis, electrocardiographic characteristics, and incidence of atrial fibrillation. Arch Dermatol Res 2013;305:891-7.
[Google Scholar]
|
| 20. |
Chiu HY, Chang WL, Huang WF, Wen YW, Tsai YW, Tsai TF. Increased risk of arrhythmia in patients with psoriatic disease: A nationwide population-based matched cohort study. J Am Acad Dermatol 2015;73:429-38.
[Google Scholar]
|
| 21. |
Egeberg A, Khalid U, Gislason GH, Mallbris L, Skov L, Hansen PR. Association between depression and risk of atrial fibrillation and stroke in patients with psoriasis: A Danish nationwide cohort study. Br J Dermatol 2015;173:471-9.
[Google Scholar]
|
| 22. |
Shahwan KT, Kimball AB. Psoriasis and Cardiovascular Disease. Med Clin North Am 2015;99:1227-42.
[Google Scholar]
|
| 23. |
Lip GY, Tse HF, Lane DA. Atrial fibrillation. Lancet 2012;379:648-61.
[Google Scholar]
|
| 24. |
Ryder MI, Saghizadeh M, Ding Y, Nguyen N, Soskolne A. Effects of tobacco smoke on the secretion of interleukin-1beta, tumor necrosis factor-alpha, and transforming growth factor-beta from peripheral blood mononuclear cells. Oral Microbiol Immunol 2002;17:331-6.
[Google Scholar]
|
| 25. |
Okubo Y, Koga M. Peripheral blood monocytes in psoriatic patients overproduce cytokines. J Dermatol Sci 1998;17:223-32.
[Google Scholar]
|
| 26. |
Frustaci A, Chimenti C, Bellocci F, Morgante E, Russo MA, Maseri A. Histological substrate of atrial biopsies in patients with lone atrial fibrillation. Circulation 1997;96:1180-4.
[Google Scholar]
|
| 27. |
Hu YF, Chen YJ, Lin YJ, Chen SA. Inflammation and the pathogenesis of atrial fibrillation. Nat Rev Cardiol 2015;12:230-43.
[Google Scholar]
|
| 28. |
Issac TT, Dokainish H, Lakkis NM. Role of inflammation in initiation and perpetuation of atrial fibrillation: A systematic review of the published data. J Am Coll Cardiol 2007;50:2021-8.
[Google Scholar]
|
| 29. |
Conway DS, Buggins P, Hughes E, Lip GY. Prognostic significance of raised plasma levels of interleukin-6 and C-reactive protein in atrial fibrillation. Am Heart J 2004;148:462-6.
[Google Scholar]
|
| 30. |
Peña JM, MacFadyen J, Glynn RJ, Ridker PM. High-sensitivity C-reactive protein, statin therapy, and risks of atrial fibrillation: An exploratory analysis of the JUPITER trial. Eur Heart J 2012;33:531-7.
[Google Scholar]
|
| 31. |
Liu T, Li G, Li L, Korantzopoulos P. Association between C-reactive protein and recurrence of atrial fibrillation after successful electrical cardioversion: A meta-analysis. J Am Coll Cardiol 2007;49:1642-8.
[Google Scholar]
|
| 32. |
Dernellis J, Panaretou M. C-reactive protein and paroxysmal atrial fibrillation: Evidence of the implication of an inflammatory process in paroxysmal atrial fibrillation. Acta Cardiol 2001;56:375-80.
[Google Scholar]
|
| 33. |
Rudolph V, Andrié RP, Rudolph TK, Friedrichs K, Klinke A, Hirsch-Hoffmann B, et al. Myeloperoxidase acts as a profibrotic mediator of atrial fibrillation. Nat Med 2010;16:470-4.
[Google Scholar]
|
| 34. |
Liao CH, Akazawa H, Tamagawa M, Ito K, Yasuda N, Kudo Y, et al. Cardiac mast cells cause atrial fibrillation through PDGF-A-mediated fibrosis in pressure-overloaded mouse hearts. J Clin Invest 2010;120:242-53.
[Google Scholar]
|
| 35. |
Musa H, Kaur K, O'Connell R, Klos M, Guerrero-Serna G, Avula UM, et al. Inhibition of platelet-derived growth factor-AB signaling prevents electromechanical remodeling of adult atrial myocytes that contact myofibroblasts. Heart Rhythm 2013;10:1044-51.
[Google Scholar]
|
| 36. |
Lee SH, Chen YC, Chen YJ, Chang SL, Tai CT, Wongcharoen W, et al. Tumor necrosis factor-alpha alters calcium handling and increases arrhythmogenesis of pulmonary vein cardiomyocytes. Life Sci 2007;80:1806-15.
[Google Scholar]
|
Fulltext Views
4,915
PDF downloads
4,052





