Translate this page into:
Psoriasis: From antiquity to the present
Corresponding author: Prof. Barbara Dorocka-Bobkowska, Department of Gerodontology and Oral Pathology, Poznan University of Medical Sciences, Wielkopolska, Poland. bdorocka@ump.edu.pl
-
Received: ,
Accepted: ,
How to cite this article: Olejnik M, Adamski Z, Dorocka-Bobkowska B. Psoriasis: From antiquity to the present. Indian J Dermatol Venereol Leprol 2023;89:149-53.
Psoriasis is a chronic, autoimmune genetic disease manifesting as skin lesions and affecting approximately 2% of the global population. The incidence of psoriasis depends on the race and geographical location. The broad spectrum of clinical manifestations ranging from single lesions to involvement of the entire skin and joints (psoriatic arthritis) and the lack of a clearly defined aetiology, makes effective treatment of psoriasis a challenge for modern medicine.1-3 The aim of this article is to present the history of psoriasis over the centuries together with treatment methods from antiquity to modern times.
Definition and research on psoriasis through the ages
Antiquity
The first records of exfoliative lesions appear in the Ebers Papyrus, an ancient Egyptian medical note dating from the 15th century BC when skin diseases were divided into three groups: irritative, exfoliative and ulcerative. As for treatment, a mixture of sea salt, urine and onion or goose fat and semen was recommended. Egyptians also established the principles of modern phototherapy—they recommended systemic topical rubbing of Ammi majus (a plant of known photosensitizing effects) followed by sun exposure.2,4,5 It has also been hypothesized that the death of Hatshepsut, an Egyptian Pharaoh, may have been caused by the use of an ointment comprising a mixture of oils and a carcinogenic tar derivative.6
In ancient Greece, skin diseases were divided into the following groups: psora (pruritic, itching), lepra (epidermal exfoliation dysfunction) and leichen.7 Hippocrates (460-377 BC) in Corpus Hipocraticum provided descriptions of dermatoses. He was the first to name exfoliating, pruritic lesions on the eyelids and genitals as psora, and recommended the application of tar followed by sun exposure as treatment.5 He also used the term lopoi to describe dry, scaly, disfiguring eruptions of psoriasis, leprosy (which were confused with each other for centuries) and other skin diseases.2,4,7
The first description of psoriasis in the modern sense is probably attributed to Cornelius Celsus (ca. 25 BC-45 AD), the Roman philosopher who, in “De Re Medica Libri Octo”, described a papulosquamous disease affecting the skin of the extremities and nails as impetigo, which was treated with tar and sulphur.7,8 The term psoriasis was first introduced by Galen (133-200) to describe an itchy, exfoliative condition of the eyelids and scrotum, corresponding to the modern definition of seborrheic dermatitis, which was managed with a viper’s broth.5,8
Middle ages and renaissance
During the Middle Ages, Western medicine did not treat skin diseases. Because psoriasis and leprosy were not differentiated, patients were stigmatized, forced to wear distinctive clothing and were not allowed to touch or eat with healthy people.2,5,7 However, Arabian physicians in Persia in the 8th century AD probably distinguished psoriasis from other skin diseases, and recognizing the psychosomatic basis, treated it with psychotherapy.2,8,9
The first systematic study of skin diseases was published as “De morbis cutaneis et omnibus corporis humani excrementis” from a series of lectures by Geronimo Mercurialis (1530-1606), an Italian professor of medicine. He divided skin diseases into those involving the scalp and the whole body, describing lesions according to the colour, shape and size. He used the term lepra grecorum for psoriasis. The treatment methods recommended by Mercurialis included rubbing a mixture of wolf dung with vinegar and goat blood into the skin.10 In 1700, Bernardino Ramazzini (1633-1714) presented diseases related to various occupations in his publication “De morbis artificum diatriba”. They included occupations with skin exposure pointing out new aetiological factors.8
The 18th and 19th centuries
The 18th century brought significant progress in the development of dermatology and an increased interest in skin diseases. With the invention and subsequent improvements of the microscope, it became possible to study and describe previously unknown structures. In 1714, the surgeon Daniel Turner (1667-1741), regarded as the father of British dermatology, published his work “De morbis cutaneis a treatment of diseases incident to the skin”. In it, he described all skin conditions known at the time, making a distinction between psoriasis (called leprosy of the Greek) managed with an ointment containing mercuric amidochloride and leprosy (leprosy of the Arabian).5,8 In 1776, Joseph Jacob von Plenck (1738-1807), a Viennese surgeon and gynaecologist, in his work “Doctrina de morbis cutaneis” classified skin diseases based on the systematics of Charles Linnaeus. He assigned psoriasis to the group of exfoliative dermatoses, but named it, like Celsus before, impetigo.2,5,8 In 1777, the French physician Anne-Charles Lorry (1726-1783) published “Tractatus de morbis cutaneis”. In his publication of more than 700 pages, he tried to classify skin diseases based on their aetiology. He described the skin as a separate organ and emphasized its relationship with other systems, especially the digestive and nervous systems.5,8,11
The beginning of the 19th century brought about the final definition of psoriasis and its distinction from leprosy. British dermatologist Robert Willan (1757-1812), in his work “On cutaneous disease”, presented the morphology of 12 primary lesions and, on this basis, classified skin diseases into eight groups. He used the term psoriasis to describe a papulosquamous dermatosis, partly distinguishing psoriasis from leprosy and presented several subtypes, including guttate and diffuse. Willan also noted that the disease often begins on the elbows and knees and may affect the scalp and fingernails. To manage psoriasis, he recommended willow, elm and juniper extracts and moderate diet and baths.2,4,5,7,8 A French physician Jean Louis Alibert (1768-1837) created a different classification of dermatoses, dividing them into 12 groups based on aetiology, course duration and treatment response. Alibert used therapeutic baths to treat mild skin diseases as well as ointments with ammoniated mercury, zinc and lead oxides and sulphurated tin in more resistant cases. He also noticed the co-occurrence of psoriatic lesions and joint deformations.4,5,8
A more refined distinction between psoriasis and leprosy was possible due to Ferdinand von Hebra (1816-1880), a Viennese physician of Czech origin who in 1841 improved Robert Willan’s classification based not only on the morphology of skin lesions but also on their microscopic description. He eliminated the term lepra from the description of psoriatic lesions, which prevented the stigmatization of patients.2,5,7,8
The role of external factors in the initiation of psoriasis was also described by Henrich Koebner (1838-1904), a German dermatologist born in Breslau, who in 1872 suggested that the appearance of psoriatic lesions was due to infection or trauma. He observed new lesions on healthy skin in psoriatic patients at the site of a horse bite or tattoo. This phenomenon was later named Koebner’s phenomenon and remains a characteristic symptom indicative of psoriasis activity.5,10,11
Another characteristic psoriasis symptom was presented by Heinrich Auspitz (1835-1886), a student of Ferdinand Hebra. Auspitz described a non-specific phenomenon-the appearance of bleeding points after the scales were removed, named Auspitz’s sign. He also introduced the terms “parakeratosis” and “acanthoma” characteristic of psoriasis, to describe the histopathological images.8,10,11,12
The 20th and 21st centuries
New types of psoriasis were defined from the beginning of the 20th century. In 1910, a German physician Leo von Zumbusch (1874-1940) described a severe, generalized pustular form of psoriasis (von Zumbusch disease), with pustular eruptions accompanied by epidermal desquamation and high fever.1,7,12 In 1926, the Russian dermatologist D.L. Woronoff described a ring-like anaemisation of the skin around the psoriatic plaque, generally appearing after topical treatment or phototherapy.7,11 In 1931, the German scientist Karl Hoede (1897-1973) from Wurzburg, presented a comprehensive study of the families of psoriatic patients. He found a positive family history in 33% of his patients, which led him to conclude that “psoriasis is an irregular dominant, which is incompletely sex-limited”.2,13
During the second half of the 20th century, there were numerous reports on the aetiology and pathogenesis of psoriasis. In 1960, Muhammad Aswaq postulated an autoimmune background for the disease.3 In 1963, Eugene van Scott and Thomas Ekel showed that the cell cycle of the keratinocytes in psoriatic patients is shortened to 36 hours compared to 311 hours in a healthy population. On the other hand, Gerald Weinstein in 1968 demonstrated a shortening of the turnover time of the epidermis from 27 to only 4 days.7,8 In the 1970s, evidence for the multigenic inheritance of the disease came in. It was found that the genes responsible for the onset of psoriasis are located on the chromosome 6 near the HLA genes. A link between the disturbance of the cellular immune response mediated by T-cell lymphocytes was also reported.2,7 Research by Tilo Henseler and Enno Christophers which was published in 1985, differentiated two types of psoriasis based on age of onset—type I characterized by the appearance of the disease in young subjects under 40 years of age and type II, in which lesions appear between the ages 50 and 70 years.1,8,14
Until the 1990s, a disturbance of keratinocyte proliferation was considered a primary cause of psoriatic lesions with subsequent lymphocyte activation and cytokine release. Nowadays, excessive activation of T-helper lymphocytes, which differentiates depending on the stimulus and causes excessive proliferation and differentiation of epidermal keratinocytes, is regarded as an essential factor in disease development. IL-12 is responsible for the differentiation of TH1 cells, whereas IL-23 influences the maturation of TH17 lymphocytes, which are also associated with inflammatory bowel diseases, rheumatoid arthritis, multiple sclerosis and inflammatory response in obesity. These discoveries led to the current belief that psoriasis, especially with a moderate and severe course, is a systemic inflammatory disorder, which may co-occur with an increased risk of cardiovascular events, diabetes and dyslipidaemia. This has resulted in the introduction of modern biological drugs for the management of psoriasis. The chronic inflammation in psoriasis pathogenesis leads to a higher incidence of cardiovascular disease in patients. Moreover, psoriasis has been associated with comorbidities like psoriatic arthritis, metabolic syndrome and brain diseases, requiring interdisciplinary co-ordination between many specialists to provide optimized treatments [Table 1].3,7,8,15-18
| 1808 | Robert Willan | Partial distinction of psoriasis from leprosy |
| 1841 | Ferdinad von Hebra | Complete distinction of psoriasis from leprosy |
| 1872 | Henrich Koebner | Appearance of psoriatic lesions at the site of injury—Koebner’s phenomenon |
| 1885 | Heinrich Auspitz | Appearance of bleeding points after scale removal—Auspitz’s sign |
| 1898 | William John Munro | Accumulation of neutrophils in the stratum corneum—Munro’s abscesses |
| 1910 | Leo von Zumbusch | Severe, generalised pustular psoriasis |
| 1926 | D.L. Woronoff | Ring-like anaemisation of the skin around the psoriatic plaque—Woronoff’s ring |
| 1931 | Karl Hoede | Genetic background of psoriasis |
| 1960 | Muhammad Aswaq | Autoimmune background of psoriasis |
| 1963 | Eugene van Scott and Thomas Ekel | Shortening of the keratinocytes cell cycle in psoriatic patients |
| 1985 | Tilo Henseler and Enno Christophers | Two types of psoriasis based on initial symptom onset |
History of psoriasis treatment
Although the initial attempts for topical treatment of psoriatic lesions were undertaken in antiquity, psoriasis therapy began to be effectively developed in the 19th century, when the definition of the disease was established. At the time, both systemic and topical management methods were applied.5,7,8 With the development of therapeutic strategies, it became necessary to assess the efficacy of these treatments. In 1978, the Psoriasis Area and Severity Index (PASI) and in 1994, the Dermatology Life Quality Index (DLQI) questionnaire were introduced to assess the impact of the therapy on the improvement of the quality of life of psoriatic patients.17
Topical treatment
An ointment based on mercury amidochloride was recommended from the 17th century until the 1970s when Werner Jadassohn (1897-1973) and Franjo Kogoj (1894-1983) had recommended this treatment for scalp psoriasis in 1972. In 1895, Brault injected organic mercury compounds to cure psoriatic arthritis.5,8,9,10
Formulations based on sulphur and salicylic acid have been used as a part of topical and systemic therapies for many years. Ferdinand Hebra and Moritz Kaposi (1837-1902) recommended their use in an ointment form to remove scales. Salicylic acid and urea are still prescribed for psoriatic patients to facilitate the penetration of anti-inflammatory drugs in the lesions.1,7,9,16
In older times, tar formulations of natural products (pine and birch) were applied as ointments, oils and baths. Coal tar became available as a by-product of coal gas production. At the end of the 19th century, William Goeckerman (1884-1952) observed a beneficial effect for coal tar in psoriatic lesions. In 1925, he introduced a combination of tar-based formulas with ultraviolet radiation, which was a very effective treatment and was recommended for many years.4,7,8,10,17
In 1876, Balmonno Squire used Goa powder to treat the condition of a patient. The main active ingredient of Goa powder was chrysarobin (2-methyl dithranol), which has been used in Indian medicine to treat dermatoses. However, at a concentration of 1-5% in an ointment base, it caused itching and skin discoloration and was very expensive, thus limiting its widespread use.7,8,9,10,17 However, a cheaper and safer equivalent of chrysarobin-anthralin was developed in 1916, which was used as a 0.1% ointment. Known as dithranol, it is still recommended for the topical management of psoriasis and is currently prescribed as a minute therapy at concentrations ranging from 0.5 to 2%. In 1953, Ingram suggested using dithranol as a photosensitiser with ultraviolet B radiation.1,4,8,9,16
In 1950, Philipp Hench (1896-1965), Edward Kendall (1886-1972) and Tadeusz Reichstein (1897-1996) received the Nobel Prize for their work on the chemical structure, synthesis and biochemical action of adrenocortical hormones, which revolutionized the management of autoimmune disorders. In 1952, Marion Sulzberger (1895-1983) and Victor Witten (1916-2007) described the beneficial effect of hydrocortisone in psoriasis treatment. In the 1960s, betamethasone valerate and fluocinolone acetonide were invented, leading to a significant improvement in inflammatory dermatoses therapy.17 Since then, corticosteroid-based formulas have been widely used in the treatment of psoriatic lesions.7,9,10,17
In 1985, an improvement in psoriasis lesions was reported in a patient treated systemically with high doses of vitamin D3 for osteoporosis, but the mechanism of action has not been explained until now. At the end of the 1980s, calcipotriol and tacalcitol were introduced as topical therapy. Currently, the combination of calcipotriol and betamethasone is widely recommended for topical management.5,7,16,17
Systemic treatment
One of the first drugs successfully used to treat psoriasis was Fowler’s solution, containing 1% potassium arsenite. It was introduced in medicine by Thomas Fowler (1736-1801) in 1786 and in 1806, it was recommended by Thomas Girdlestone as a systemic treatment of psoriasis. In addition, pilulae asiaticae, consisting of arsenic, black pepper, acacia and water and subcutaneous injections of arsenous acid were used at the time. Despite numerous adverse effects such as hepatotoxicity and carcinogenicity, arsenic-based agents were in use until the mid-20th century.5,7,8,9,17
The therapeutic effect of sunlight on psoriatic lesions was known in older times. In 1895, Niels Finsen (1860-1904) used an arc lamp to treat lupus vulgaris lesions, introducing phototherapy with artificial light.5 In 1973, the efficacy of UVA light in combination with oral photosensitizers to achieve remission of psoriasis was reported.17 However, the potential for skin cancer led to a search for safer methods. In 1981, John Parish and Kurt Jaenicke were able to overcome this problem with the use of ultraviolet B radiation in the range 300-313 nm.5,7,8,10 More recently, excimer laser, at a wavelength of 308 nm, directed selectively onto the lesions, has provided long-term remission.4
In 1948, Boston physician Sidney Farber (1903-1973) used aminopterin, the folic acid antagonist, to treat acute leukaemia. In 1951, Richard Gubner (1914-1995) noticed an improvement in the skin condition of a psoriatic patient treated with aminopterin for rheumatoid arthritis. Subsequently, in 1958, methotrexate, a safer and more stable derivative was introduced and received Food and Drug Administration approval in 1972 as a treatment for psoriasis. It remains one of the most effective agents in psoriasis and psoriatic arthritis therapy.8,10,16,17
In the late 1950s, the German chemist Walter Schweckendiek used fumaric acid esters to treat psoriasis as he postulated that it was the deficiency of fumaric acid that led to the onset of psoriasis. In 1969, John Yarbro reported the efficacy of hydroxyurea in clearing refractory psoriasis.17,19
Simultaneously, in the 1960s, retinoids were introduced for the treatment of acne and keratinization disorders. Twelve years later, isotretinoin was used for the first time in psoriasis therapy, followed by its derivatives etretinate and acitretin, which are currently recommended as the drugs of choice in generalised pustular psoriasis. The third generation of retinoids now includes tazarotene, which is available for topical therapy.5,7,10,16,17
Cyclosporine was first isolated in 1969, and in 1976, its immunosuppressive effect was discovered, which allowed its widespread use in transplantology for the prevention of graft rejection. In 1979, it was shown that cyclosporine improved the clinical condition of patients with psoriasis and psoriatic arthritis. In 1997, Food and Drug Administration approved it for psoriasis treatment, but it is generally prescribed for a short course due to nephrotoxicity.1,7,10,16,17
The understanding of the immunological background of the disease and the development of biotechnology enabled the introduction of new drugs—proteins with a targeted effect on the selected stage of the immune response. The first of which, etanercept, a tumour necrosis factor inhibitor, was approved for psoriatic arthritis treatment in 2002 and two years later, for plaque psoriasis. Tumour necrosis factor inhibitors also include adalimumab, a human monoclonal antibody introduced in the therapy in 2005; infliximab, a chimeric (human-mouse) monoclonal antibody that was approved a year later; golimumab; and the newest- certolizumab pegol—a Fab fragment of antibody conjugated to polyethylene glycol, which has been used to treat psoriatic arthritis since 2013 and plaque psoriasis since 2018.7,8,10,16,17 Psoriasis was the first inflammatory disease, to be treated using ustekinumab, approved by FDA in 2009. This human monoclonal antibody binds to the p40 subunit of both IL-12 and IL-23 and is highly effective and safe.16,17 Recent biologic agents introduced after 2015 include the IL-17 inhibitors (secukinumab, ixekizumab and brodalumab) and IL-23 inhibitors (guselkumab, risankizumab and tildrakizumab).16,17 New molecules including inhibitors of IL-1, IL-6 or IL-8 are currently being evaluated.20
In 2014, apremilast was introduced as a therapy for psoriasis and psoriatic arthritis with a favourable safety profile for oral administration. Another novel drug, tofacitinib, an oral Janus kinase inhibitor targeting JAK1 and JAK3, has been successfully used in psoriasis. Tofacitinib regulates the immune response via the interruption of intracellular signalling pathways, which are involved in the pathogenesis of psoriasis. It seems to be well tolerated and may also be administered as topical therapy for both psoriasis and atopic dermatitis.17
Many supportive methods and lifestyle modalities such as diet modification, helio-marinotherapy in health resorts such as Dead Sea region and balneocosmetics have been introduced as adjunctive therapy for psoriasis.8,21
Figure 1 shows the development of psoriasis therapy.
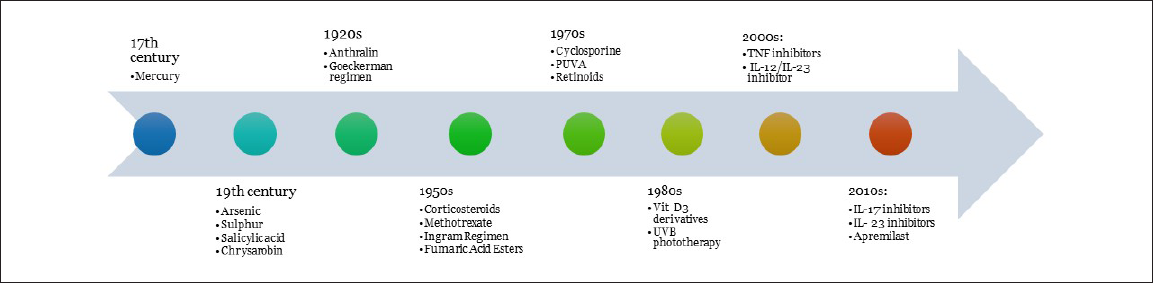
- Development of psoriasis therapy
Conclusion
Psoriasis has been known since ancient times and has been investigated for centuries by eminent scientists. Scientific research into the disease began in the 19th century and continues until today. Although newer effective drugs are being developed every year, due to the incompletely defined aetiology of the disease, the search for a cure has proved elusive for millions of patients worldwide.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Aspekty kliniczne i epidemiologiczne zaburzeń ogólnoustrojowych u chorych na łuszczycę [doctoral dissertation] Poznań: Poznan University of Medical Sciences; 2011.
- [Google Scholar]
- Historical development of local therapy of psoriasis vulgaris. Acta Dermatovenerol Croat. 2004;12:191-5.
- [PubMed] [Google Scholar]
- From Arsenic to Biologicals: A 200 Year History of Psoriasis. Beckenham: Garner Press; 2008.
- [Google Scholar]
- Did Skin Cream Kill Egypt’s Queen Hatshepsut? 2011. [accessed 2020 Oct 10]. Available from:
- [Google Scholar]
- Introduction: History of psoriasis and psoriasis therapy. In: Von Weinberg WJ, ed. Treatment of Psoriasis. Basel: Birkhauser Verlag AG; 2008. p. :1-9. In red.
- [Google Scholar]
- History of psoriasis. 2012. Psoriasis—A Systemic Disease. InTech; In editor Available from:
- [Google Scholar]
- Psoriasis treatment yesterday, today, and tomorrow. Acta Dermatovenerol Croat. 2004;12:30-4.
- [PubMed] [Google Scholar]
- History of psoriasis. In: Von Weinberg JM, Lebwohl M, eds. Advances in Psoriasis: A Multisystemic Guide. London: Springer Verlag; 2014. p. :1-8. In red.
- [CrossRef] [Google Scholar]
- Lepra vulgaris. History of psoriasis. J Turk Acad Dermatol. 2014;8:1483r1.
- [CrossRef] [Google Scholar]
- A genetic and statistical study of psoriasis. Am J Hum Genet. 1951;3:267-81.
- [PubMed] [PubMed Central] [Google Scholar]
- Presentation of early onset psoriasis in comparison with late onset psoriasis: A clinical study from Pakistan. Indian J Dermatol Venereol Leprol. 2009;75:36-40.
- [CrossRef] [PubMed] [Google Scholar]
- Psoriasis. Diagnostic and therapeutic recommendations of the Polish Dermatological Society. Part 2. Dermatol Rev. 2020;107:110-37.
- [CrossRef] [Google Scholar]
- Psoriasis and treatment: Past, present and future aspects. Acta Derm Venereol. 2020;100:adv00032.
- [CrossRef] [PubMed] [Google Scholar]
- Psoriasis and co-morbidity. Acta Derm Venereol. 2020;100:adv00033.
- [CrossRef] [PubMed] [Google Scholar]
- Hydroxyurea as an alternative therapy for psoriasis. Indian J Dermatol Venereol Leprol. 2004;70:13-7.
- [PubMed] [Google Scholar]





