Psychodermatology – a case for sensitization of pharmacists in Mumbai, India
Corresponding author: Dr. Ram H. Malkani, Jaslok Hospital, Room No. 200, Dr. G Deshmukh Marg, Mumbai - 400 026, Maharashtra, India. malkanipub@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Malkani RH, Parekh K, Karmakar S, Setia MS. Psychodermatology – a case for sensitization of pharmacists in Mumbai, India. Indian J Dermatol Venereol Leprol 2023;89:261-5.
Abstract
Background:
Though studies have looked at the attitudes of dermatologists towards psychodermatology, few have highlighted the attitudes of pharmacists towards these conditions.
Objectives:
To study the knowledge, attitudes and practices of pharmacists towards the prescription of psychotropic medications to dermatology patients.
Methods:
This cross-sectional analysis included 80 pharmacists from Mumbai, India. We used an interviewer-administered questionnaire to collect information from pharmacists on their demographics, psychotropic medications in dermatological patients, knowledge about psychocutaneous conditions and comfort about dispensing these medications.
Results:
In our study, 37 (46%) of pharmacists received prescriptions of psychotropic drugs from dermatologists; however, 24 (30%) were not comfortable dispensing them. Sixty (75%) pharmacists felt that only psychiatrists should prescribe psychotropic drugs and 37 (46%) felt that they had a right to refuse to dispense prescribed medication; of these, 15 (19%) had actually refused to give medications to patients. Pharmacists who disagreed with the statement that 'the state of mind is associated with medical conditions', were more likely to discourage psychotropic prescription from dermatologists (29% vs 11%, P = 0.04). Pharmacists with experience of more than five years were significantly more likely to refuse to dispense medications (odds ratio: 5.14, 95% confidence interval: 1.02, 25.83; P = 0.047).
Limitations:
We did not have a list of all pharmacists in Mumbai; thus, no sampling frame could be applied.
Conclusion:
Pharmacists do comment on doctors’ prescriptions, discourage certain medications and even refuse to dispense them based on their personal opinions. Since they are the last stop for patients between the doctor and the medication, their inclusion (in addition to dermatologists, psychiatrists and psychologists) in integrated awareness, training and care programs would improve the quality of care of patients with psychocutaneous disorders.
Keywords
Comments
dermatology
pharmacists
prescription
psychocutaenous
psychotropic
Introduction
Psychocutaneous conditions—involving an interaction between the mind and skin—are often neglected in clinical dermatology training and practice in India.1,2 It has been reported that 30–40% of all dermatological cases may have an underlying psychological issue.2,3 The proper management of these conditions often includes a combination of dermatological therapy and psychological therapy; the latter may include cognitive behavioral therapy, biofeedback, hypnotic therapy or psychotropic medications.4,5 If behavioral therapy is preferred, the patient would receive adequate care from the psychologist or psychiatrist. However, if psychotropic drugs are prescribed by the treating dermatologist, the role of the pharmacist becomes relevant.
The pharmacist is often the last in the healthcare chain to see the patient before the patient starts using the drugs prescribed. Neighbourhood pharmacists are accessible to patients and may be seen on several occasions between routine physician visits. Therefore, the pharmacist has an important role in ensuring the safe and appropriate use of medications by patients. This becomes even more important for psychotropic medications; the optimal involvement of pharmacists may improve adherence to psychotropic medications.6
In India, mental health may be stigmatized even among healthcare workers.7 A study from south India also found that only 13% of dermatologists were comfortable treating patients with psychocutaneous disorders.8 Some important barriers in providing pharmaceutical care in mental health are lack of knowledge, stigma and skill of the pharmacist.9-10 It has been reported that an active psychopharmacology course can change the attitudes of pharmacy students towards mental health.11 Though studies have discussed the attitudes of dermatologists toward psychodermatology, few have highlighted the attitudes of pharmacists towards these conditions.12-14 Even though a psychodermatology liaison clinic model has been proposed by Indian dermatologists, the pharmacists’ importance is often not considered; the latter’s beliefs and attitudes could affect the care of patients with psychocutaneous disorders.15
We conducted a study to understand the knowledge, attitudes and practices of pharmacists towards the prescription of psychotropic medications to dermatology patients. We also wanted to study the association between attitudes, behaviors and practices in these pharmacists.
Methods
Study population and procedures
This study was a cross-sectional analysis that included 80 pharmacists from various parts of Mumbai. The study was approved by the Ethics Committee of the local institution.
We approached pharmacists in their standalone pharmacies and all those who consented to be part of the study were included. We first selected a specific region and street. The sampling was not random, it was purposive. We only covered one area in a day. We only included shops that had ‘pharmacy’, ‘pharmacists’, or ‘chemists and druggists’ on their signboards. We did not include pharmacy counters in large stores. We approached the pharmacist in their shop and explained the present study; if the pharmacist consented, we proceeded with the questionnaire. The main pharmacist was approached and we did not include workers in the shop for the study. We had also decided that if there were two pharmacists in the shop, only the first one approached and who consented would be included. We then moved to the next shop in the street and repeated the procedure.
A preformed interviewer-administered questionnaire was designed to collect data on knowledge, attitudes and practices. The questionnaire was primarily designed by the primary author (RM). It was based on review of literature. The questionnaire collected the following information: 1) demographic data: age, sex, education, years of experience as a pharmacist; 2) prescription patterns in dermatology patients; 3) psychotropic drugs in dermatology patients; 4) knowledge about psychocutaneous conditions; 5) pharmacists’ attitudes towards patients who had a prescription of psychotropic medications, level of comfort in discussing the use of these medications; 6) need for these medications in dermatology patients; 7) dispensing of these medications to dermatology patients or refusal to do so; 8) any other information related to prescription of psychotropic medications to dermatology patients. Responses were collected on a five-point Likert scale (strongly disagree/disagree/neutral/ agree/strongly agree) for the statements.16 For the purpose of analyses, we combined 'strongly agree/agree' as 'agree' and 'strongly disagree/disagree' as 'disagree'. The responses were collected by one of the investigators, KP (psychologist working with the dermatologist). The same individual was involved in gathering the responses from all pharmacies.
Statistical methods
We estimated the means and standard deviations or medians and interquartile range for continuous variables and proportions for categorical variables. The proportions across groups were compared using the Chi-square test or Fisher’s exact test for low expected cell counts. We used logistic regression models to estimate the odds ratios and their 95% confidence intervals for unifactorial and multifactorial analyses. The multifactorial models included age, sex, qualification, years of experience and knowledge about psychocutaneous diseases; these were the potential confounders in the data. Data were analyzed using Stata Version 15.1 (© StataCorp, College Station, Texas, USA).
Results
The mean age (±standard deviation) of these 80 pharmacists was 32.4 (±10.9) years. In our study, 71 (89%) of the included pharmacists were male and nine (11%) were female. A majority were diploma holders (48, 60%), followed by bachelor’s degree-holders (21, 26%) and those with other qualifications (11, 14%). The median (interquartile range) years of experience as a pharmacist was five (2, 14.5) years. Work experience was greater in male than in female pharmacists, but the difference was not statistically significant (M: 6 [2, 15] vs F: 1.5 [1, 5]; P = 0.14).
We found that 37 (46%) pharmacists had received a prescription of psychotropic drugs from dermatologists; however, 24 (30%) were not comfortable dispensing them. Twenty-one (26%) pharmacists disagreed with the statement that psychological factors (such as stress or anger) may be responsible for skin conditions including eczema and itching. Sixty (75%) pharmacists agreed with the statement that only psychiatrists should prescribe psychotropic drugs. Further, 37 (46%) agreed that they have a right to refuse the prescribed medication; of these, 15 (41%) stated that they had refused to give medication to patients. Twenty-nine (36%) participants refused to give medicines to their patients. We also found that 13 (16%) of them agreed with the statement that they were cleverer than doctors. Details are presented in Figure 1.
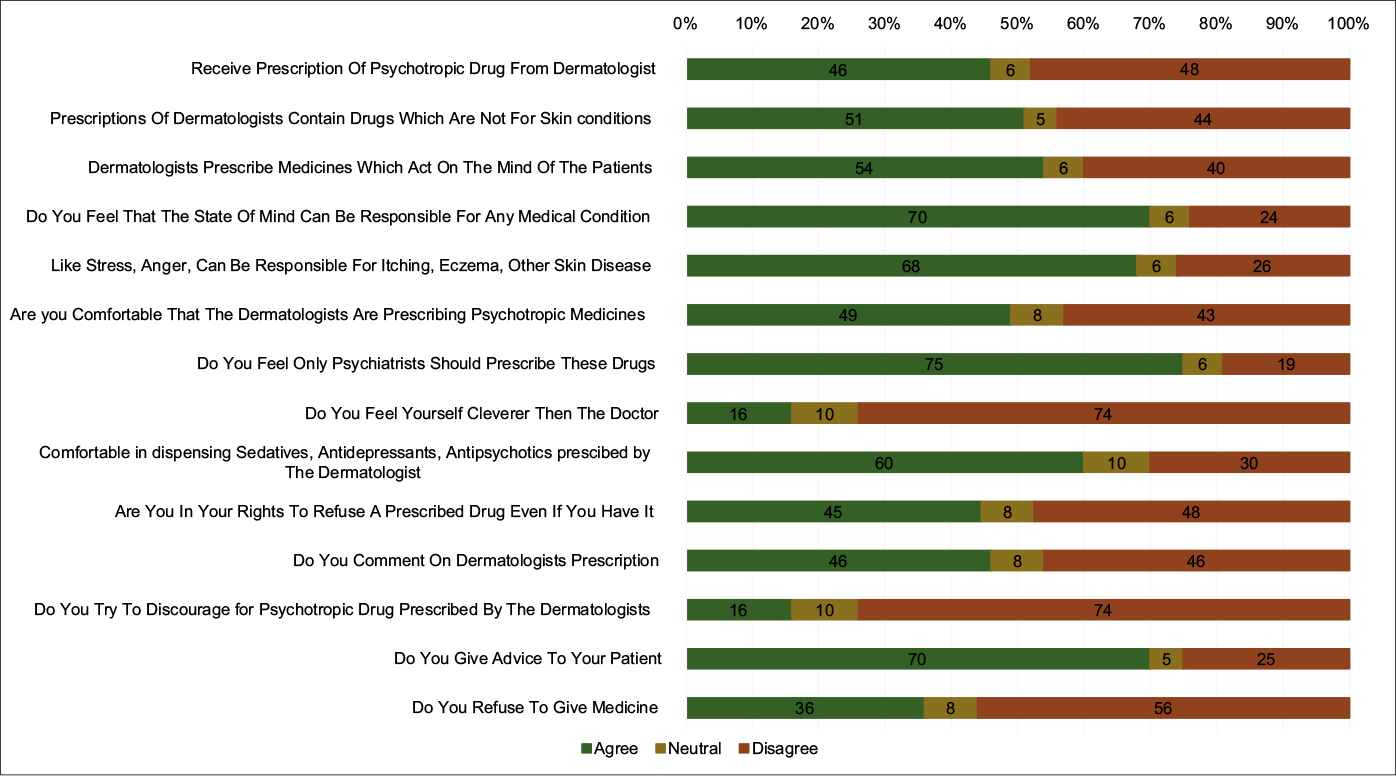
- The attitudes and behaviors of 80 pharmacists, Mumbai, India
Pharmacists who disagreed with the statement that the state of mind was associated with medical conditions were more likely to discourage psychotropic prescriptions from dermatologists (29% vs 11%, P = 0.04). In the unifactorial models, we found that those who agreed that the state of mind can be responsible for medical conditions were less likely to discourage psychotropic medications (odds ratio: 0.29, 95% confidence interval: 0.09, 0.99; P = 0.048). After adjusting for age, sex, qualification and agreement with the statement that psychological factors are associated with skin disorders, we found that pharmacists with experience of more than five years were significantly more likely to refuse to dispense medications compared with those with experience of less than five years (odds ratio: 5.14, 95% confidence interval: 1.02, 25.83; P = 0.047). Additional proportions and odds ratios are presented in Table 1.
| Variables | Total, (n=80; 100%), n (%) | Discourage medications | Refuse medications | |||
|---|---|---|---|---|---|---|
| n (%) | OR (95% CI) | n (%) | OR (95% CI) | |||
| Age (years) | ||||||
| 20–29 | 43 (54) | 10 (23) | Reference | 15 (35) | Reference | |
| 30–39 | 20 (25) | 2 (10) | 0.36 (0.07–1.86) | 8 (40) | 1.24 (0.42–3.71) | |
| ≥40 | 17 (21) | 1 (6) | 0.21 (0.02–1.75) | 6 (35) | 1.02 (0.31–3.30) | |
| Sex | ||||||
| Female | 9 (11) | 3 (33) | Reference | 2 (22) | Reference | |
| Male | 71 (89) | 10 (14) | 0.33 (0.07–1.53) | 27 (38) | 2.15 (0.42–11.10) | |
| Experience (years) | ||||||
| 0–5 | 42 (53) | 11 (26) | Reference | 11 (26) | Reference | |
| >5 | 38 (47) | 2 (5)* | 0.16 (0.03–0.76) | 18 (47)* | 2.53 (1.00–6.48) | |
| Qualification | ||||||
| Bachelor’s degree | 21 (26) | 3 (14) | Reference | 9 (43) | Reference | |
| Diploma | 48 (60) | 9 (19) | 1.38 (0.33–5.73) | 14 (29) | 0.55 (0.19–1.59) | |
| Others | 11 (14) | 1 (9) | 0.60 (0.05–6.56) | 6 (55) | 1.60 (0.37–6.95) | |
| State of mind can be responsible for medical condition** | ||||||
| Disagreed/neutral | 24 (30) | 7 (29) | Reference | 10 (42) | Reference | |
| Agreed | 56 (70) | 6 (11)* | 0.29 (0.09–0.99) | 19 (34) | 0.71 (0.27–1.92) | |
| Only psychiatrists should prescribe psychotropic drugs** | ||||||
| Disagreed/neutral | 20 (25) | 3 (15) | Reference | 7 (35) | Reference | |
| Agreed | 60 (75) | 10 (17) | 1.13 (0.28–4.61) | 22 (37) | 1.08 (0.37–3.10) | |
| Are you in your rights to refuse a prescription even if you have it in stock** | ||||||
| Disagreed/neutral | 44 (55) | 7 (16) | Reference | 14 (32) | Reference | |
| Agreed | 36 (45) | 6 (17) | 1.06 (0.32–3.48) | 15 (42) | 1.53 (0.61–3.83) | |
P<0.05, **Strongly agreed/agreed were included in agreed. OR: Odds ratio, CI: Confidence interval
Discussion
Psychodermatology is as much about the mind as about the skin.21-23 Reviews and training material have discussed the role of psychiatric treatment modalities therein, including psychotropic medications,2,4,5 but it is a neglected specialty and lacks scientific practice in India.1 Counseling by the dermatologist may convince the patient about the relationship between the mind and the cutaneous condition, but if the pharmacist discourages or refuses to give them the prescribed medications, it may make the patients apprehensive about this association.
We found that most of the pharmacists surveyed were aware of the role of the mind in skin conditions. In our study, pharmacists, who were aware of the role of mind in disease, were less likely to discourage psychotropic medications. Even though most of the pharmacists received prescriptions for and were comfortable in dispensing psychotropic medications, many others discouraged or refused these medications to patients. Most of them commented on the prescription and believed only psychiatrists should prescribe these medications. Pharmacists with experience of less than five years were apparently more likely to discourage psychotropic medication when prescribed by a dermatologist but those with experience of more than five years seemed significantly more likely to refuse medications. Thus, it would seem that early in their career, some pharmacists might just discourage psychotropic medications prescribed by dermatologists but as they become more experienced, they may be more confident and refuse to dispense the medications.
Studies have shown that pharmacists are reluctant to discuss medication use with patients with mental illness, in contrast to other patients.17,18 Though attitudes of pharmacists towards psychodermatology have not been studied in detail, it has been observed that there is a lack of awareness about these conditions in dermatologists themselves.8,19,20 It is likely that few dermatologists prescribe psychotropic medications and the pharmacist therefore may have apprehensions in giving these medications to the occasional patient who comes with such prescriptions from dermatologists. Better focus on psychocutaneous disorders in postgraduate dermatology training may increase appropriate psychotropic drug prescription by dermatologists; pharmacists receiving such prescriptions more frequently may then be more comfortable dispensing them.
A previous study found that poor knowledge of mental health, low demand from patients, lack of initiative and discomfort in dealing with psychiatric patients were common barriers faced by pharmacists.13 Another review found that reducing the stigma around mental health and improving pharmacists’ confidence in providing mental health services may overcome barriers for effective mental health services.12
Limitations
This was a sample of only a few pharmacists in the city of Mumbai. We did not have a complete list of pharmacists in the city; thus, no sampling frame could be applied. The questionnaire does not represent an exhaustive list of attitudes and behaviors. Due to social desirability, we may have underestimated the proportion of pharmacists who discourage or refuse medications. Working with a psychiatrist or having a mental health patient in the household may change attitudes and behaviours; these were not accounted for in the study.
Conclusion
This study provides useful information on the attitudes and behaviors of pharmacists toward dispensing psychotropic medications to patients with dermatological prescriptions. Pharmacists comment on doctors’ prescriptions, discourage certain medications and may sometimes even refuse them based on their personal opinion. Since pharmacists are the last stop for the patient between the doctor and the medication, their inclusion (in addition to dermatologists, psychiatrists and psychologists) in integrated awareness, training and care programs might improve the quality of care of patients with psychocutaneous disorders.24
Acknowledgments
The study was presented as a poster at the ESDaP Congress Giessen, Germany 2019.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Psychodermatology: An Indian perspective. Clin Dermatol. 2018;36:737-42.
- [CrossRef] [PubMed] [Google Scholar]
- Psychodermatology: A comprehensive review. Indian J Dermatol Venereol Leprol. 2013;79:176-92.
- [CrossRef] [PubMed] [Google Scholar]
- Psychodermatological disorders: Recognition and treatment. Int J Dermatol. 2011;50:1309-22.
- [CrossRef] [PubMed] [Google Scholar]
- A survey assessment of the recognition and treatment of psychocutaneous disorders in the outpatient dermatology setting: how prepared are we? J Am Acad Dermatol. 2013;68:47-52.
- [CrossRef] [PubMed] [Google Scholar]
- The knowledge, awareness, and practice patterns of dermatologists toward psychocutaneous disorders: Results of a survey study. Int J Dermatol. 2010;49:784-9.
- [CrossRef] [PubMed] [Google Scholar]
- Awareness of psychodermatology in Indian dermatologists: A South Indian perspective. Dermatol Ther. 2020;33:e14024.
- [CrossRef] [Google Scholar]
- New roles for pharmacists in community mental health care: A narrative review. Int J Environ Res Public Health. 2014;11:10967-90.
- [CrossRef] [PubMed] [Google Scholar]
- Perception of community pharmacists in Malaysia about mental healthcare and barriers to providing pharmaceutical care services to patients with mental disorders. Community Ment Health J. 2020;56:88-98.
- [CrossRef] [PubMed] [Google Scholar]
- Positive attitude change toward psychiatry in pharmacy students following an active learning psychopharmacology course. Acad Psychiatry. 2008;32:515-7.
- [CrossRef] [PubMed] [Google Scholar]
- Community pharmacy services to optimise the use of medications for mental illness: A systematic review. Aust New Zealand Health Policy. 2005;2:29.
- [CrossRef] [PubMed] [Google Scholar]
- Knowledge of and attitudes toward clinical depression among health providers in Gujarat, India. Ann Glob Health. 2014;80:89-95.
- [CrossRef] [PubMed] [Google Scholar]
- Attentiveness of dermatologists in the middle east to psychocutaneous medicine. Prim Care Companion CNS Disord. 2017;19:2080.
- [CrossRef] [PubMed] [Google Scholar]
- Psychodermatology liaison clinic in India: a working model. Trop Doct. 2018;48:7-11.
- [CrossRef] [PubMed] [Google Scholar]
- Methodology series module 8: Designing questionnaires and clinical record forms. Indian J Dermatol. 2017;62:130-4.
- [CrossRef] [PubMed] [Google Scholar]
- Community pharmacists' attitudes toward and professional interactions with users of psychiatric medication. Psychiatr Serv. 2004;55:1434-6.
- [CrossRef] [PubMed] [Google Scholar]
- Attitudes of pharmacists toward mental illness and providing pharmaceutical care to the mentally Ill. Ann Pharmacother. 2005;39:1450-5.
- [CrossRef] [PubMed] [Google Scholar]
- Psychodermatology: Knowledge, awareness and attitudes of Dermatologists in Eastern Europe. Milan 2019
- [Google Scholar]
- Psychodermatology: Psychological and psychiatrical aspects of dermatology. Przegl Lek. 2008;65:244-8.
- [Google Scholar]
- Psychodermatology: An association of primary psychiatric disorders with skin. Rev Colomb Psiquiatr. 2019;48:50-7.
- [CrossRef] [PubMed] [Google Scholar]
- The need of dermatologists, psychiatrists and psychologists joint care in psychodermatology. An Bras Dermatol. 2017;92:63-71.
- [CrossRef] [PubMed] [Google Scholar]






