Translate this page into:
Purpuric paradigm: Multiple purpuric lesions on palms
Corresponding author: Dr. Sanjeev Handa, Department of Dermatology, Venereology and Leprology, PGIMER, Chandigarh, India. handa_sanjeev@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Sharma A, Baskaran N, Chatterjee D, Handa S. Purpuric paradigm: Multiple purpuric lesions on palms. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_478_2024
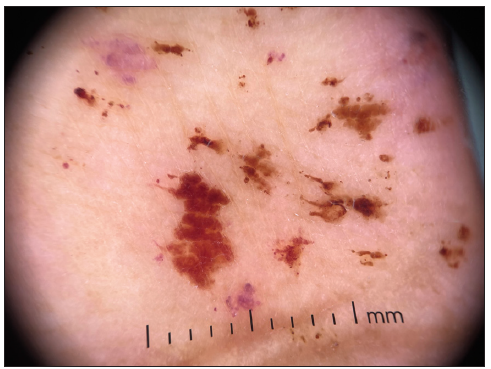
A 67-year-old man presented with a 2-month history of asymptomatic, pinpoint, reddish to brownish lesions predominantly on the palmar aspects of both hands. The patient had a history of coronary angioplasty with stenting performed a year back due to obstructive coronary artery disease, after which his condition had stabilised. There were no significant systemic symptoms, and his general physical examination was unremarkable, with normal vital signs. Cutaneous examination revealed the presence of multiple, discrete, dark reddish to brownish purpuric macules present on the palmar surfaces of both hands, mainly on the index and middle fingers, slightly extending to the dorsal aspects [Figure 1]. Dermoscopic examination revealed violaceous and erythematous dots (recent petechial lesions) along with erythematous and brown dots and globules (old petechial lesions) [Figure 2]. The rest of the systemic examination was within normal limits.

- Multiple, discrete, dark reddish to brownish purpuric macules on the palmar aspects of both hands, mainly on the index and middle fingers slightly extending onto the dorsal aspect.
- Violaceous and erythematous dots (recent petechial lesions); erythematous and brown dots and globules (old petechial lesions) (DermLite™ DL4; x10 polarised mode).
Histopathological findings
Histopathological examination of the lesions revealed the epidermis showing compact orthokeratosis, spongiosis, and mild lymphocytic exocytosis. In the papillary dermis, collections of polymorphonuclear cells were observed. The upper dermis showed perivascular lymphomononuclear inflammatory infiltrate, along with histiocytes. Vasculitic changes were evident, characterised by prominent endothelial cell swelling, RBC extravasation, and angiocentric neutrophilic infiltration [Figures 3a and 3b]. Direct immunofluorescence (DIF) showed granular deposits of IgA (2+) along the tips of the dermal papillae [Figure 3c].
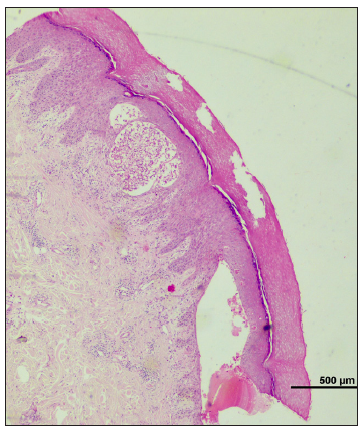
- Epidermis displays compact orthokeratosis and spongiosis. The upper dermis shows perivascular infiltrate of lymphomononuclear cells and histiocytes with evidence of vasculitis. (Haematoxylin and eosin, 40x).
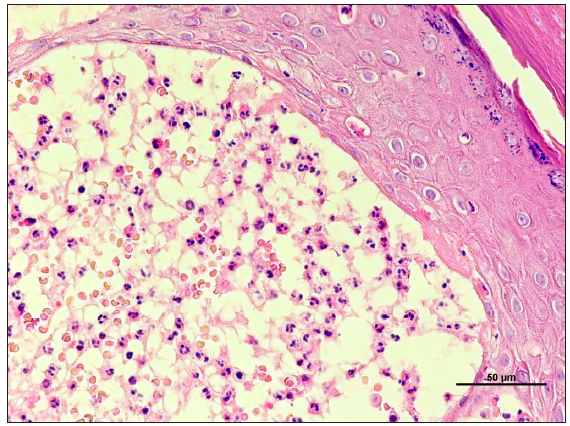
- The upper dermis showing perivascular lymphomononuclear inflammatory infiltrate, and evidence of vasculitis in the form of prominent endothelial cells, extravasation of red blood cells, and neutrophilic infiltration. (Haematoxylin and eosin, 400x).
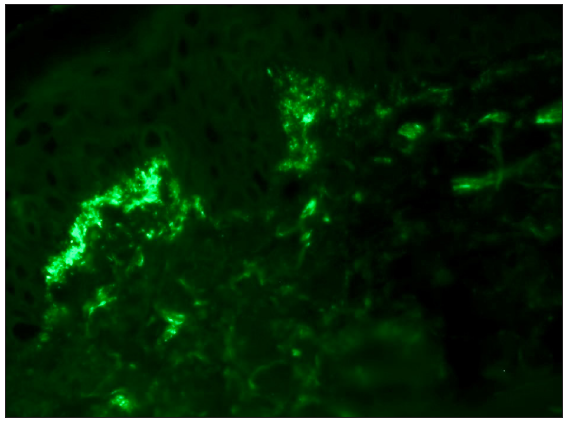
- Direct immunofluorescence shows granular IgA deposition along the tip of dermal papillae. (Fluorescein isothiocyanate, 400x).
Question
What is your diagnosis?
Answer
Dermatitis herpetiformis (DH).
Discussion
Dermatitis herpetiformis (DH), also known as Duhring-Brocq disease, is a chronic inflammatory bullous disorder associated with gluten-sensitive enteropathy. It typically presents as itchy erythematous grouped excoriated vesicles and papules, symmetrically involving the extensor of limbs, shoulder, and buttocks.1 Lesions may also be haemorrhagic and may exhibit surface crusting. Atypical presentations, including palmoplantar hyperkeratosis, chronic urticaria, and prurigo-like forms, have also been reported.2
The purpuric lesions observed in our patient align with previous reports of DH-associated vasculitis-associated purpura on hands.3 Immunopathologically, the convergence of IgA deposition and immune complex dynamics in the dermal microvasculature contributes to a hypersensitivity vasculitis, unveiling the intricate interplay of immune dysregulation. Our case highlights both the diagnostic challenges and the persistent link between gluten sensitivity and cutaneous vasculitis.4,5 The hands are a rare but documented site for DH lesions, and the presence of purpura in this location adds to the complexity of the disease spectrum. Important differential diagnoses include IgA vasculitis, sub-acute bacterial endocarditis (SABE)-associated vasculitis, papular-purpuric glove-and-sock syndrome, and acral haemorrhagic Darier disease, each in an appropriate clinical setting. IgA vasculitis and SABE-associated vasculitis predominantly present as purpuric lesions predominantly affecting distal lower extremities with associated systemic features, demonstrating leukocytoclastic small vessel vasculitis on histopathology. Acral haemorrhagic Darier disease presents as haemorrhagic macules, papules, and/or vesicles over the extremities, demonstrating dyskeratosis and suprabasal acantholysis with haemorrhagic lacunae on histopathology.
Histopathology classically demonstrates a neutrophilic papillary tip micro abscess in the subepidermal location, which was present in our case. Perilesional DIF shows granular or fibrillar deposits of IgA, which are pathognomonic for DH. Notably, patients with DH rarely manifest with overt gastrointestinal symptoms of Celiac disease, as seen in our patient. Management of DH typically involves a gluten-restricted diet and dapsone, which are the cornerstone of treatment and usually lead to complete resolution of pruritus and skin lesions.1 In this case, the patient had significant improvement after 3 months of treatment and continues to be under follow-up.
The current case of DH with purpuric lesions on the hands contributes to the evolving understanding of this dermatological condition. Clinicians should remain vigilant for vasculitic manifestations in DH, especially when purpuric lesions are evident, to ensure timely diagnosis and appropriate management in the spectrum of gluten-sensitive dermatoses.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Dermatitis herpetiformis: An update on diagnosis and management. Am J Clin Dermatol. 2021;22:329-38.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Newly described clinical and immunopathological feature of dermatitis herpetiformis. Clin Dev Immunol. 2012;2012:967-74.
- [Google Scholar]
- Acral purpura as leading clinical manifestation of dermatitis herpetiformis: Report of two adult cases with a review of the literature. Dermatology. 2013;227:1-4.
- [CrossRef] [PubMed] [Google Scholar]
- [Pseudopurpuric palmar localizations of herpetiform dermatitis] Ann Dermatol Venereol. 1983;110:121-6.
- [PubMed] [Google Scholar]
- Palmar petechiae in dermatitis herpetiformis: a case report and clinical review. Cutis. 2002;70:217-23.
- [PubMed] [Google Scholar]





