Translate this page into:
Pustular lesions in the neonate: Focused diagnostic approach based on clinical clues
Corresponding author: Dr. Rahul Mahajan, Department of Dermatology, Venereology and Leprology, Postgraduate Institute of Medical Education & Research, Chandigarh, India. drrahulpgi@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Afra T, Daroach M, Mahajan R, De D, Handa S. Pustular lesions in the neonate: Focused diagnostic approach based on clinical clues. Indian J Dermatol Venereol Leprol 2022;88:708-16.
Abstract
Pustules in a neonate can be due to various causes. Though the majority of conditions causing pustules in a neonate are benign, it is essential to clearly differentiate these from serious ones. A systematic approach based on detailed history and clinical examination of the neonate along with basic laboratory evaluation narrows down diagnostic possibilities and aids in the correct diagnosis. This review outlines a step-by-step approach so as to avoid clinical dilemmas and unnecessary intervention.
Keywords
Pustules
neonate
diagnosis
benign
infectious
Introduction
The first four weeks of extrauterine life constitute the neonatal period. Neonates may develop pustules due to innocuous causes or serious reasons. The presence of pustules in a newborn can cause apprehension in the parents and the neonatologists leading to extensive investigations to find the etiology.
The diagnostic approach to pustular lesions in a neonate should be focused as relevant to the clinical presentation. Meticulous clinical evaluation supported by simple bedside laboratory tests can narrow diagnostic possibilities and help differentiate between the benign and more sinister possibilities. This review is aimed at outlining a diagnostic approach to pustular lesions in the neonate based on clinical findings and basic laboratory evaluation [Figures 1a and b]. While this approach encompasses the more common etiologies manifesting as pustules in the neonatal period, the list herein (Table 1) is not exhaustive and we do not attempt to detail the clinical and epidemiologic characteristics of each dermatosis individually.
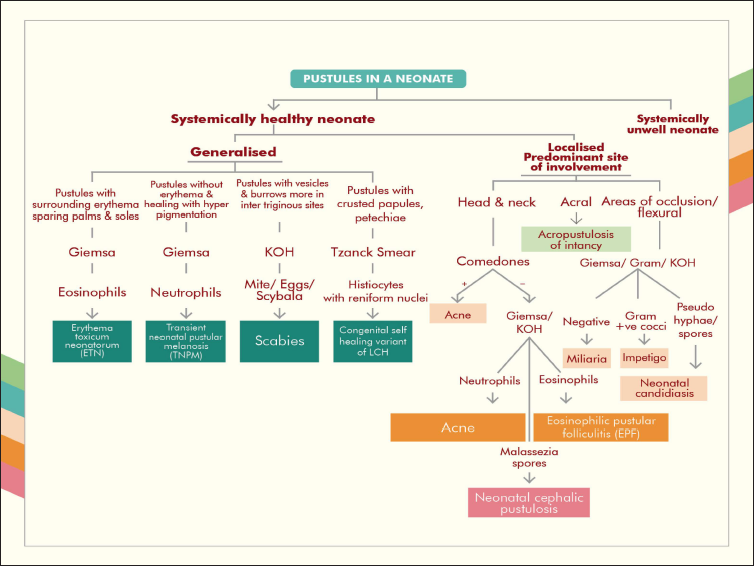
- Flowchart of the diagnostic approach to a systemically healthy neonate presenting with pustules
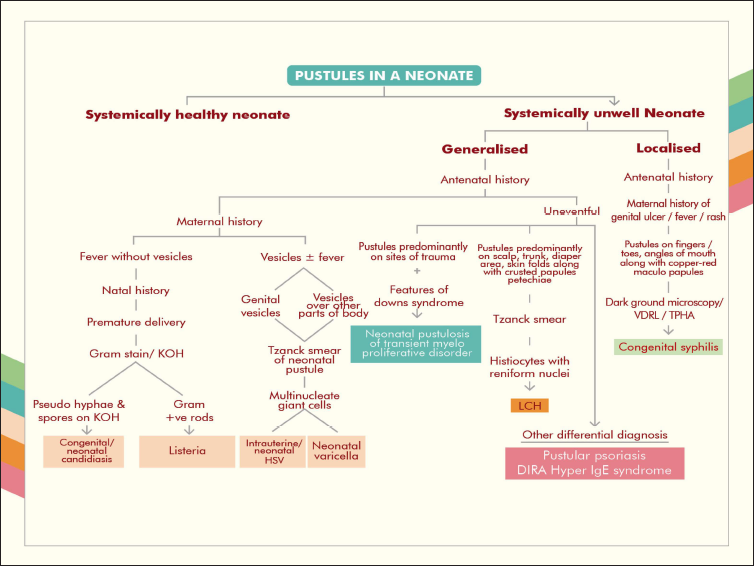
- Flowchart of the diagnostic approach to a systemically unwell neonate presenting with pustules
| Category | Etiology |
|---|---|
| Benign self-limiting dermatoses5 |
Common causes Erythema toxicum neonatorum Transient neonatal pustular melanosis10 Miliaria/heat rash Neonatal cephalic pustulosis Neonatal acne Uncommon causes Acropustulosis of infancy Eosinophilic pustular folliculitis |
| Infections |
Bacterial Impetigo Congenital syphilis Listeria monocytogenes infection Pseudomonas aeruginosa infection Hemophilus influenzae infection Viral Herpes simplex virus infection (intrauterine, neonatal) Varicella (foetal varicella syndrome/congenital varicella/varicella embryopathy, neonatal varicella, neonatal herpes zoster) Fungal Candidiasis (congenital, neonatal) Dermatophytosis Aspergillosis Parasitic Scabies |
| Associated with neoplasm | Neonatal pustulosis of transient myeloproliferative disorder Langerhans cell histiocytosis (congenital Langerhans cell histiocytosis, Hashimoto-Pritzker disease or congenital self-healing reticulohistiocytosis) |
| Inflammatory dermatosis | Pustular psoriasis |
| Primary immunodeficiency disorders | Hyper-IgE syndrome/Job syndrome Deficiency of interleukin-1 receptor antagonist |
| Miscellaneous | Incontinentia pigmenti Autoimmune blistering diseases (neonatal pemphigus, gestational pemphigoid, pemphigus foliaceous) |
Epidemiology and etiology
There is a relative scarcity of large epidemiologic studies on pustular eruptions in neonates. In a study from India involving 100 neonates with pustular eruptions, 36 (36%) were in the early neonatal period (first week of life). The majority of these were of infectious etiology (58%) and among families of poor socioeconomic status (96%).1 In another study by Goyal et al. 18 (41%) of neonates were diagnosed with erythema toxicum neonatorum, four (9%) each with miliaria crystallina and staphylococcal pyoderma, three (6.8%) with neonatal acne, two (4.5%) each with group A streptococcal impetigo, sucking blisters and neonatal tinea faciei and one (2.3%) each with neonatal candidiasis, neonatal varicella, scabies, transient neonatal pustular melanosis, epidermolysis bullosa simplex, incontinentia pigmenti, eosinophilic pustular folliculitis, pemphigus vulgaris and neonatal herpes simplex.2 Erythema toxicum neonatorum is the commonest neonatal pustular dermatosis, seen in 16-30% of newborns.3 Impetigo is the most common primary skin infection in neonates that presents with pustules.
Pustular lesions in neonates can be categorized based on etiology as: (1) benign self-limiting dermatoses, (2) infections, (3) inflammatory dermatoses, (4) neoplastic disorders, (5) primary immunodeficiency disorders and (6) miscellaneous disorders [Table 1].4-9
Approach
The initial evaluation of neonatal pustules includes the history of onset and course of the pustules, general physical examination, cutaneous examination and basic laboratory evaluation. The clinician should identify whether the cutaneous pustules are a manifestation of a systemic disease or a disease limited to the skin. The general condition of the neonate can provide insight into this. The distribution of pustules further aids the diagnosis. The causes of generalised or localized pustules in a term healthy neonate who is accepting feeds normally are mostly benign eruptions or cutaneous infections. In such a scenario, the benign neonatal pustuloses possible include erythema toxicum neonatorum, transient neonatal pustular melanosis, miliaria/heat rash, neonatal cephalic pustulosis, neonatal acne and the less common acropustulosis of infancy or eosinophilic pustular folliculitis.10 These conditions are usually transient, self-limiting and asymptomatic in a neonate. Certain cutaneous infections like impetigo, neonatal candidiasis and scabies can also present as pustules in an otherwise well child. The distribution and morphology of the pustules as well as simple laboratory tests (including Giemsa stain, Gram stain and potassium hydroxide study) on the contents of pustule establishes the diagnosis in most cases.
Along with the clues obtained during the initial evaluation a more detailed history including antenatal and natal history is to be undertaken if the condition remains undiagnosed after the first step. During this stage, a thorough cutaneous examination with systemic examination should be carried out in consultation with paediatrician and more specific laboratory tests can be ordered based on the history and examination findings. Pustules in a neonate who is premature, unwell, has difficulty feeding, maternal history of fever, rash, vesicles, vaginal candidiasis, intrauterine devices, cervical sutures, premature rupture of membranes or chorioamnionitis can be a marker of more serious systemic disease. These findings should lead to a focused evaluation for the diagnosis of systemic infections, certain inflammatory dermatoses, neoplasms, primary immunodeficiency disorders and other rare disorders.
Maternal and family history
In general, maternal history and family history are noncontributory in the scenario of cutaneous pustules in an otherwise well neonate except in a few conditions.
A history of itching, dermatophytosis or scabies in the mother or a close family member may point to a diagnosis of the same condition in the neonate.11,12 Though a rare cause of neonatal pustules, maternal pemphigus vulgaris can lead to neonatal pemphigus, which has an excellent prognosis.13
History of vesicles in the mother in the genital area during pregnancy points towards neonatal herpes simplex infection. The presence of vesicles or pustules during the last three weeks of pregnancy, especially between five days before and two days after delivery is a strong indication of neonatal varicella.14,15 If there is any suspicion of congenital syphilis, the clinician should seek the history suggestive of primary chancre or secondary syphilis in the mother and history of exposure in mother.16 History of vaginal candidiasis, intrauterine devices, cervical sutures, premature rupture of membranes or chorioamnionitis in the mother indicate risk factors for candidiasis in the neonate.17,18
The family history and pedigree chart analysis help in the diagnosis of primary immunodeficiency disorders such as Job syndrome (autosomal dominant hyper-IgE syndrome) and deficiency of the interleukin-1-receptor antagonist- (autosomal recessive) as well as incontinentia pigmenti (X-linked dominant; mother may be asymptomatic or have mosaic hypopigmented streaks on skin).8,9,19
Birth history
Erythema toxicum neonatorum is common in full term healthy male neonates with no gestational risk factors.10 Among infectious causes, neonates who have acquired the disease during their intrauterine life are usually premature and of low birth weight as in intrauterine herpes simplex virus infection and listeria infection.20,21 Premature and low birth weight infants are also at risk of developing systemic spread of cutaneous infection as in candidiasis.4
Age at onset
Although the timing of onset of the pustular eruption is not a very specific clue , a few clinical entities may manifest more frequently in early neonatal life(first week of life) [Figure 2]. Among the benign causes, transient neonatal pustular melanosis tends to present at birth in newborns with pigmented skin whereas erythema toxicum neonatorum begins after 24-48 hours from delivery in a full-term neonate with a waxing and waning course and completely resolves in a week.22,23 Of the infectious causes, those acquired during intrauterine life present at birth itself (intrauterine herpes simplex virus infection, congenital candidiasis, congenital syphilis)14,16,24 whereas those acquired close to the time of birth (neonatal herpes simplex virus infection, neonatal varicella, neonatal candidiasis)14,15 or in the immediate postpartum period (impetigo) present a few days to two or three weeks after birth.6
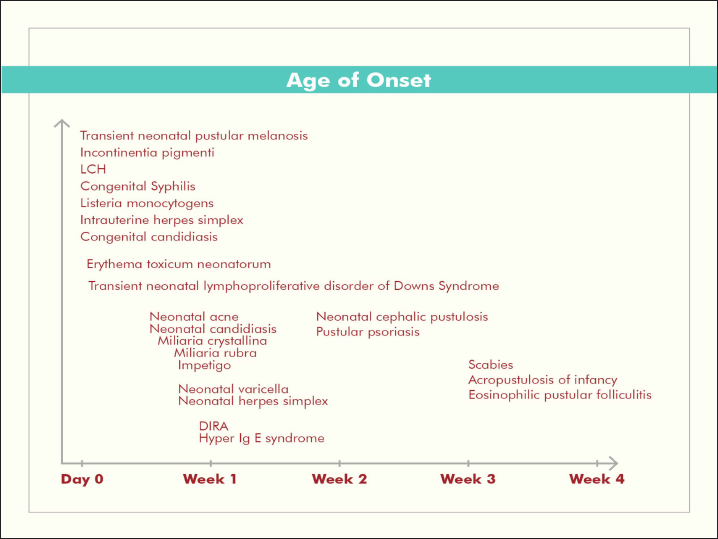
- Diagrammatic representation of the age of onset of pustular lesions in the neonate
Morphology and distribution
In most conditions, the pustules evolve from macules, papules or vesicles. The morphology and pattern of distribution of the eruption (pustules along with other skin lesions) are important in diagnosis. It should be noted if the pustules are generalised or localized. Generalised pustules in a healthy neonate are seen in erythema toxicum neonatorum, transient neonatal pustular melanosis, scabies and rarely the congenital self-healing variant of Langerhans cell histiocytosis. In these conditions, along with the morphology and distribution of the pustules, other associated lesions come into the picture. In erythema toxicum neonatorum, transient erythematous macules, wheals, vesicles, pustules and papules in varying combinations are seen all over the body except on the palms and soles, where pilosebaceous units are absent [Figure 3].5 This eruption starts on the face and then involves the proximal extremities, trunk and buttocks. The pustules in transient neonatal pustular melanosis lack surrounding erythema and they rupture leaving a collarette of scale; palms and soles may be affected. The hyperpigmented macules left behind on clearing of the pustules may last longer.23 In contrast to older children, scabies in neonates presents with vesicles and pustules along with its other classical lesions such as erythematous papules, nodules, and burrows. In neonates, the presentation is usually generalised involving the palms, soles, head and neck with lesions more concentrated on the wrists, axillae, periumbilical region, medial feet and groins [Figure 4]. Eczematisation and secondary infection can also supervene. In severe infestation, the neonate may be irritable with poor feeding and inadequate weight gain.12 Congenital self-healing Langerhans cell histiocytosis presents as red-brown macules, papules and nodules which can be solitary or generalized all over the body. Varied presentations with vesicles, pustules and blueberry muffin lesions can also be seen. Though the disease is limited to the skin, a thorough evaluation to rule out systemic involvement is needed.25

- Pustules over trunk surrounded by erythematous halos, suggestive of erythema toxicum neonatorum

- Pustules over axilla in a neonate with scabies
When the pustules are localised, some differentials can be arrived at based on the predominant area of involvement. The differential diagnosis when papulopustules are located in the head and neck region are neonatal acne, neonatal cephalic pustulosis and eosinophilic pustular folliculitis. Erythematous papulopustules on the face are seen in neonatal acne and neonatal cephalic pustulosis [Figure 5]. In newborns with neonatal acne, facial pustules are accompanied by comedones in 23-30% of cases.26,27 In eosinophilic pustular folliculitis, recurrent crops of esiculopustules occur on the face and scalp and may be associated with hemorrhagic crusts.6,28 If comedones are not seen, microscopy with Giemsa stain or a potassium hydroxide smear may aid diagnosis. A closely related condition, acropustulosis of infancy presents similar to eosinophilic pustular folliculitis, but the sites of predilection are the hands and feet.28

- Erythematous papulopustules over face and scalp without comedones in benign cephalic pustulosis
Localised pustules are also seen in miliaria, impetigo and neonatal candidiasis. In miliaria, sites of predilection are occluded areas like the neck and back. In miliaria crystallina, clear tiny vesicles are seen over healthy skin. Multiple erythematous papules or papulovesicles on an erythematous background are seen in miliaria rubra. The contents may become pustular due to deeper obstruction (miliaria pustulosa) or due to secondary infection (periporitis).5 Bullous impetigo is common over the perineum, periumbilical area and neck creases and manifests as rapidly enlarging thin walled flaccid bullae with a narrow rim of erythema. The bullae rupture easily to form moist erosions with a collarette of scales at the edge. In nonbullous impetigo, the vesicle or pustule is transient and forms honey-coloured crusted plaques with surrounding erythema.29 It may be emphasized that while the majority of neonates with impetigo will have mild limited disease, it is important to look for any systemic signs and symptoms, lymphadenopathy, and general condition as it may spread very quickly to involve larger areas of the body or evolve into staphylococcal scalded skin syndrome.30 Beefy red erythematous moist plaques with a scalloped outline and satellite pustules in the napkin area are seen in neonatal candidiasis which is a common cause of neonatal pustules. It starts from the perianal area and spreads peripherally. It may be associated with oral thrush and localized palmar pustules as a result of inoculation of Candida from the mouth into the skin due to sucking.6
Pustules in a neonate due to an underlying systemic disease are mostly generalised. In congenital candidiasis (intrauterine infection) there is extensive involvement of the body with palms, soles and nails characteristically involved. The oral cavity and diaper region are usually spared here, in contrast to neonatal candidiasis (where the neonate acquires the infection during its passage through the infected birth tract). Disseminated involvement in neonatal candidiasis can however be seen in premature and low birth weight infants.6,31
Even though the features of herpes simplex virus infection (intrauterine and neonatal) and varicella (fetal varicella syndrome, neonatal varicella and neonatal herpes zoster) overlap, there are certain subtle cutaneous features that help to differentiate these conditions. Vesicles evolving into pustules and crusts are present in all these situations, though rare in fetal varicella syndrome. Vesicles are less extensive in neonatal herpes simplex virus infection than in neonatal varicella and lack the classical grouping.6 Cutaneous scars and aplasia cutis are characteristic features of intrauterine infections (herpes simplex virus and varicella), the dermatomal pattern being more specific for varicella.14,15 Involvement of oral or conjunctival mucosa favours the diagnosis of herpes simplex.14
In transient myeloproliferative disorder associated with Down syndrome, vesiculopustular eruptions are seen predominantly on the face but may also involve the trunk and extremities and resolve spontaneously within weeks to months. Lesions also develop at sites of minor trauma or adhesive dressings.32 Crusted papules and pustules along with nodules, petechiae, fissures and oozy lesions over the scalp, diaper area and skin folds are indicators of congenital Langerhans cell histiocytosis [Figure 6].33,34 Pustular psoriasis in neonates may present as napkin psoriasis with dissemination, generalised pustular psoriasis of von Zumbusch type or annular or circinate forms.7,35,36 Deficiency of the interleukin-1-receptor antagonist also presents similarly with generalised pustules. Onychomadesis can also be seen.9 In the hyper-IgE syndrome, papulopustules are distributed predominantly on the scalp and face along with other sites like the neck, axillae and napkin area. Eczematous lesions and cold abscesses are also seen though more common after the neonatal period.8

- Crusted papules and pustules on the back in congenital Langerhans cell histiocytosis
Pustules on the fingers, toes and at the angles of the mouth along with the typical copper-red maculopapules, vesiculobullous lesions or condyloma lata will clinch the diagnosis of early congenital syphilis in the neonate.16 Vesicles and pustules in a linear and whorled distribution corresponding to Blaschko’s lines in a female neonate are a clear indicator of incontinentia pigmenti [Figure 7].19

- Vesicles and pustules along Blaschko's lines in a female neonate with incontinentia pigmenti
Systemic features
Systemic involvement is absent in the benign self-limiting dermatoses.10 The presence of systemic features is a sign to consider more serious causes in the differential diagnosis [Table 2].
| Systemic features | Diagnosis to be considered |
|---|---|
| None | Benign self-limiting dermatosis5 |
| Hepatosplenomegaly, pseudoparalysis, respiratory distress | Congenital syphilis16 |
| Microcephaly, chorioretinitis | Intrauterine herpes simplex virus infection14 |
| Central nervous system involvement, hepatitis, lethargy, poor feeding | Neonatal herpes simplex virus infection14 |
| Dermatomal scarring, aplasia cutis, neurologic defects, eye disease, skeletal anomalies | Congenital varicella syndrome15 |
| Pneumonia, hepatitis. | Neonatal varicella15 |
| Fever, respiratory distress, sepsis, deranged liver function tests | Systemic candidiasis37 |
| Features of Down syndrome, hepatosplenomegaly, high white cell count and presence of blasts | Neonatal pustulosis of transient myeloproliferative disorder32 |
| Bone pain, lymph node enlargement, hepatosplenomegaly, respiratory failure, poor appetite, irritability | Langerhans cell histiocytosis25 |
| Recurrent pneumonia with pneumatocele, osteopenia, retention of deciduous teeth, recurrent bacterial and fungal infections | Job syndrome8 |
| Multifocal aseptic osteomyelitis, periostitis | Deficiency of IL 1 receptor antagonist (DIRA)9 |
| Central nervous, ophthalmic and dental anomalies | Incontinentia pigmenti19 |
Basic laboratory evaluation
Basic laboratory tests include microscopic examination of the contents of the vesiculopustule using Gram stain, Giemsa stain/Tzanck smear and potassium hydroxide mounts. The findings of these tests taken with the clinical setting can confirm the diagnosis in most cases of pustules in neonates [Table 3].
| Investigation | Findings | Diagnosis |
|---|---|---|
| Giemsa stain | Eosinophils | Erythema toxicum neonatorum22 Eosinophilic pustular folliculitis5 |
| Neutrophils | Transient neonatal pustular melanosis5 Acropustulosis of infancy5 |
|
| Lymphocytes | Miliaria5 | |
| Fungal spores | Neonatal cephalic pustulosis38 | |
| Gram stain | Neutrophils and gram-positive cocci in clusters (Staphylococcus aureus) and in chains (Streptococcus) | Impetigo6 |
| Potassium hydroxide (KOH) preparation | Pseudohyphae and spores | Candidiasis31 |
| Hyphae | Dermatophytosis4,11 | |
| Mites, eggs and scybala | Scabies4,12 | |
| Tzanck smear | Multinucleate giant cells | Viral infections (both herpes simplex virus and varicella)6 |
| Acantholytic cells | Neonatal pemphigus39 | |
| Histiocytes with reniform nuclei and abundant cytoplasm | Langerhans cell histiocytosis40 | |
| Blast cells | Neonatal pustulosis of transient myeloproliferative disorder41 | |
| Dark field microscopy | Treponemes | Congenital syphilis16 |
Further diagnostic evaluation
Based on the initial findings, the clinician can consider more specific laboratory tests to confirm the diagnosis [Table 4].
| Suspected diagnosis | Diagnostic evaluation |
|---|---|
| Impetigo | Culture of pustular contents6 |
| Congenital syphilis | Serology, complete hemogram with differential count, liver function tests, X-rays of the chest and joints, CSF analysis, auditory, ophthalmologic and neurologic evaluation16 |
| Herpes simplex virus and varicella | Maternal type-specific serology (HSV), viral specific staining techniques, PCR and cultures14 |
| Candidiasis | Culture of pustular contents, blood, urine, cerebrospinal fluid (if dissemination/systemic infection suspected), liver function tests42 |
| Neonatal pustulosis of transient myeloproliferative disorder. | Skin biopsy, full blood count, peripheral smear32 |
| Langerhans cell histiocytosis | Skin biopsy, full blood counts, serum electrolytes, renal function tests, liver function tests, coagulation studies, ESR, C-reactive protein, skeletal survey, bone marrow studies, chest X-ray, MRI of the brain, HRCT of the chest, abdominal ultrasound, liver biopsy (as indicated)25 |
| Pustular psoriasis | Skin biopsy, full blood counts, ESR and C-reactive protein36 |
| Job syndrome | Serum IgE, full blood counts, systemic evaluation as indicated8 |
| Deficiency of IL-1 receptor antagonist (DIRA) | Skin biopsy, full blood counts and acute-phase reactants9 |
HSV: Herpes simplex virus, PCR: Polymerase chain reaction, ESR: Erythrocyte sedimentation rate, MRI: Magnetic resonance imaging, HRCT: High resolution computed tomography
Conclusion
Even though there are numerous causes for pustules in a neonate, these are benign in a large proportion and resolve without much intervention and without any complications. Most of the common causes can be diagnosed during the initial clinical evaluation. Extensive laboratory evaluation may be needed if the clinical presentation is suggestive of a more serious or systemic disease presenting as pustules in the neonatal period and can be managed accordingly. Overenthusiastic labeling of a benign condition as serious can lead to unnecessary parental distress and iatrogenic complications, and should be avoided.
Acknowledgement
We thank the parents of the patients for granting permission for clinical photography. We also thank Mr. Sansin Dulkifl, Bachelor of Multimedia Communication for the technical assistance in flow chart preparation and Dr.Vinay Keshavmurthy for providing Figure 6.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
References
- Analytical study of pustular eruptions in neonates. Pediatr Dermatol. 2002;19:210-5.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence of vesicobullous and erosive disorders of neonates: Where and how much to worry? Indian J Pediatr. 2021;88:574-8.
- [CrossRef] [PubMed] [Google Scholar]
- Prospective study of erythema toxicum neonatorum: Epidemiology and predisposing factors. Pediatr Dermatol. 2012;29:166-8.
- [CrossRef] [PubMed] [Google Scholar]
- Vesicles and pustules in the neonate. Semin Perinatol. 2013;37:8-15.
- [CrossRef] [PubMed] [Google Scholar]
- Benign skin disease with pustules in the newborn. An Bras Dermatol. 2016;91:124-34.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis and treatment of pustular disorders in the neonate. Pediatr Dermatol. 1997;14:131-43.
- [CrossRef] [PubMed] [Google Scholar]
- Generalized pustular psoriasis in childhood. Pediatr Dermatol. 2010;27:349-54.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous manifestations of hyper-IgE syndrome in infants and children. J Pediatr. 2002;141:572-5.
- [CrossRef] [PubMed] [Google Scholar]
- Monogenic autoinflammatory diseases: Concept and clinical manifestations. Clin Immunol. 2013;147:155-74.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology and predisposing factors for erythema toxicum neonatorum and transient neonatal pustular: A multicenter study. Pediatr Dermatol. 2017;34:422-6.
- [CrossRef] [PubMed] [Google Scholar]
- Neonatal autoimmune blistering disease: A systematic review. Pediatr Dermatol. 2016;33:367-74.
- [CrossRef] [PubMed] [Google Scholar]
- Neonatal herpes simplex virus infection: Epidemiology and treatment. Clin Perinatol. 2015;42:47-59.
- [CrossRef] [PubMed] [Google Scholar]
- Treponemal infections in the pediatric population. Clin Dermatol. 2000;18:687-700.
- [CrossRef] [PubMed] [Google Scholar]
- Candida chorioamnionitis diagnosed by amniocentesis with subsequent fetal infection. Am J Perinatol. 1986;3:213-8.
- [CrossRef] [PubMed] [Google Scholar]
- Congenital cutaneous candidiasis associated with respiratory distress and elevation of liver function tests: A case report and review of the literature. J Am Acad Dermatol. 1997;37:817-23.
- [CrossRef] [PubMed] [Google Scholar]
- Incontinentiapigmenti: A comprehensive review and update. Ophthalmic Surg Lasers Imaging Retina. 2015;46:650-7.
- [CrossRef] [PubMed] [Google Scholar]
- Segmental vitiligo associated with generalized vitiligo (mixed vitiligo): A retrospective case series of 19 patients. J Am Acad Dermatol. 2011;65:965-71.
- [CrossRef] [PubMed] [Google Scholar]
- Listeriosis in pregnancy: A review. Obstet Gynecol Surv. 2019;74:362-8.
- [CrossRef] [PubMed] [Google Scholar]
- Approach to dermatologic disorders in black children. Semin Dermatol. 1995;14:15-20.
- [CrossRef] [PubMed] [Google Scholar]
- Congenital cutaneous candidiasis. J Am Acad Dermatol. 1982;6:926-8.
- [CrossRef] [PubMed] [Google Scholar]
- Langerhans cell histiocytosis in children - a disease with many faces. Recent advances in pathogenesis, diagnostic examinations and treatment. Postepy Dermatol Alergol. 2018;35:6-17.
- [CrossRef] [PubMed] [Google Scholar]
- Acne neonatorum: A study of 22 cases. Int J Dermatol. 1999;38:128-30.
- [CrossRef] [PubMed] [Google Scholar]
- Acne neonatorum in the eastern Saudi Arabia. Indian J Dermatol Venereol Leprol. 2008;74:298.
- [CrossRef] [PubMed] [Google Scholar]
- Infantile eosinophilic pustular folliculitis. Dermatology. 1994;189:133-8.
- [CrossRef] [PubMed] [Google Scholar]
- Congenital staphylococcal scaled skin syndrome: Report of a case. Pediatr Infect Dis J. 1992;11:413-4.
- [PubMed] [Google Scholar]
- Congenital cutaneous candidiasis: Case report and review. Pediatr Dermatol. 1995;12:355-8.
- [CrossRef] [PubMed] [Google Scholar]
- Neonatal vesiculopustular eruption associated with transient myeloproliferative disorder: Report of four cases. Int J Dermatol. 2013;52:1202-9.
- [CrossRef] [PubMed] [Google Scholar]
- Langerhans cell histiocytosis of the skin. Hematol Oncol Clin North Am. 1998;12:269-86.
- [CrossRef] [Google Scholar]
- Congenital self-healing reticulohistiocytosis: Concern for a poor prognosis. Dermatol Online J. 2012;18:2.
- [PubMed] [Google Scholar]
- Intertriginous pustular psoriasis. J Am Acad Dermatol. 2009;60:679-83.
- [CrossRef] [PubMed] [Google Scholar]
- Congenital cutaneous candidiasis: Clinical presentation, pathogenesis, and management guidelines. Pediatrics. 2000;105:438-44.
- [CrossRef] [PubMed] [Google Scholar]
- Is common neonatal cephalic pustulosis (neonatal acne) triggered by Malassezia sympodialis? Arch Dermatol. 1998;134:995-8.
- [CrossRef] [PubMed] [Google Scholar]
- Neonatal pemphigus vulgaris: Role of passively transferred pemphigus antibodies. Br J Dermatol. 1982;106:465-7.
- [CrossRef] [PubMed] [Google Scholar]
- Congenital Langerhans cell histiocytosis: The utility of the Tzanck test as a diagnostic screening tool. Arch Dermatol. 1998;134:1039-40.
- [CrossRef] [PubMed] [Google Scholar]
- Tzanck smear for quick screening of transient myeloproliferative disorder in neonates with vesiculopapular eruptions. Int J Dermatol. 2015;54:e251-3.
- [CrossRef] [PubMed] [Google Scholar]






