Translate this page into:
Pyoderma gangrenosum: A clinico-epidemiological study
2 Department of Dermatology, Government Medical College, Kottayam, Kerala, India
3 Department of Dermatology, Amina Hospital, Perinthalmanna, Kerala, India
4 Department of Dermatology, Lisa Skin Clinic, Kozhikode, Kerala, India
5 Department of Dermatology, Valluvanad Hospital, Ottappalam, Kerala, India
Correspondence Address:
Sarita Sasidharanpillai
'Rohini', Girish Nagar, Nallalam PO, Kozhikode - 673 027, Kerala
India
| How to cite this article: Riyaz N, Mary V, Sasidharanpillai S, Roshin RA, Snigdha O, Latheef EN, Rahima S, Bindu V, Anupama RN, Sureshan DN, Sherjeena PV. Pyoderma gangrenosum: A clinico-epidemiological study. Indian J Dermatol Venereol Leprol 2017;83:33-39 |
Abstract
Background: Pyoderma gangrenosum is a neutrophilic dermatosis of unknown etiology, with inconstant systemic associations and a variable prognosis. Aims: To study the clinical features and systemic associations of pyoderma gangrenosum and its response to treatment. Methods: All patients diagnosed to have pyoderma gangrenosum at the dermatology department of the Government Medical College, Kozhikode, from January 01, 2005 to December 31, 2014 were included in this prospective study. Results: During the 10-year study period, 61 patients were diagnosed to have pyoderma gangrenosum. A male predilection was noted. The most common clinical type was ulcerative pyoderma gangrenosum (90.2%). More than 60% of patients had lesions confined to the legs; 78.7% had a single lesion and 27.9% had systemic associations. Most patients required systemic steroids. Patients with disease resistant to steroid therapy were treated with intravenous immunoglobulin G and split-thickness skin grafts under immunosuppression induced by dexamethasone pulse therapy. All except one patient attained complete disease resolution. Limitations: The main limitation of our study was the small sample size. Conclusions: The male predilection documented by us was contrary to most previous studies. We found split-thickness skin graft to be a useful option in resistant cases. More prospective studies may enable the formulation of better diagnostic criteria for pyoderma gangrenosum and improve its management.Introduction
Pyoderma gangrenosum is a sterile inflammatory neutrophilic dermatosis characterized by recurrent painful cutaneous ulcers with undermined bluish edges and surrounding erythema.[1] The common clinical variants are ulcerative, pustular, bullous and vegetative forms. Certain rare types have also been described.[2] In more than 50% of cases, a systemic association is documented.[1],[3] Although the initial description of pyoderma gangrenosum dates back to 1916, its etiopathogenesis remains unclear to date.[4] Histology of pyoderma gangrenosum reveals neutrophilic infiltration without vasculitis or granuloma formation. At times, it is impossible to differentiate it from other ulcerative processes with dermal neutrophilia.
Not much information is available on the clinical patterns, associations of pyoderma gangrenosum and treatment response in the Indian population.
Methods
After obtaining a clearance for the study from the institutional ethics committee and with the written informed consent of each patient, all patients who attended the dermatology outpatient department of Government Medical College, Kozhikode with lesions suggestive of pyoderma gangrenosum during the 10-year study period from January 1, 2005 to December 31, 2014, were carefully evaluated. The duration, onset and evolution of the disease were recorded. Co-existing systemic diseases and a detailed drug history were noted in each case. A complete hemogram, urine microscopy, peripheral smear for atypical cells and blast forms, random blood sugar estimation, fasting lipid profile, renal and liver function tests, serum electrolytes, serum electrophoresis, serology for rheumatoid factor, human immunodeficiency virus and hepatitis A, B and C viruses, antinuclear antibody profile and thyroid function tests were performed in each patient. All patients presenting with leg ulcers were examined to identify any clinical features suggestive of arterial or venous insufficiency; a sickle cell test and Doppler studies of the arterial and venous systems were also carried out. Ophthalmologic evaluation, chest radiography, barium swallow, barium meal follow-through, colonoscopy, sigmoidoscopy, gastroduodenoscopy, endoscopic biopsy, ultrasonogram of the abdomen and pelvis, computerized tomogram of the abdomen and thorax, and bone marrow analysis were done when indicated. After excluding ulcers due to arterial and venous insufficiency and those due to infective causes and hematological dyscrasias, the remaining patients were advised to undergo pathergy testing and a wedge biopsy from the ulcer edge. Biopsy specimens were sent for culture for acid-fast bacilli as well as for histopathology. A diagnosis of pyoderma gangrenosum was made based on clinical presentation, histopathology and exclusion of other diseases that may have a similar presentation. Those diagnosed as pyoderma gangrenosum were included in the study.
A preset proforma was used to collect data regarding age, sex and evolution of the ulcer. Patients were specifically asked about the original lesion and disease progression. Site, size, number, morphology and clinical characteristics of lesions were documented. Pain experienced by each patient was graded on a visual analog scale. Data on past history of similar lesions and comorbidities as well as details of investigations done were collected. The treatment received by the patient as well as the response were recorded.
Those who responded to topical or intralesional steroids and/or inhibitors of neutrophil chemotaxis (colchicine, dapsone, minocycline or salazopyrin) were classified as having mild pyoderma gangrenosum. Patients who needed daily systemic steroids with or without immunomodulators (either neutrophil chemotaxis inhibitors or immunosuppressants such as azathioprine) were considered to have moderate disease and those who were not responsive to daily systemic steroids or in whom a coexisting disease contraindicated daily systemic steroids were categorized as having severe pyoderma gangrenosum.
Patients were followed up till complete resolution of the disease. Whenever treated patients came back to us with recurrences during the study period, details were carefully documented. The data were analyzed and clinico-epidemiological aspects, associated systemic diseases and response to treatment were studied.
Results
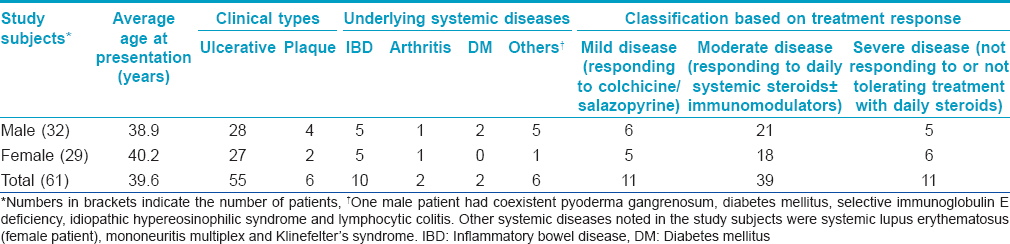
During the study period, 61 patients [Table - 1] who attended our department were diagnosed as having pyoderma gangrenosum. Of these, 32 were males and 29 were females. The age of patients ranged from 1.5 to 76 years with an average of 39.7 years.
The initial lesions observed were papules (30 patients, 49.2%), pustules (19 patients, 31.1%), erosions (10 patients, 16.4%) and plaques (2 patients, 3.3%). The most common site affected was the leg with 48 (78.7%) manifesting leg lesions and 37 (60.7%) having lesions confined to the legs [Figure - 1]a. The other areas involved included the face (4.9%), trunk (13.1%) [Figure - 1]b, upper limbs (11.5%), thighs (8.2%), buttocks (4.9%), penis (3.3%) and vulva (4.9%) [Figure - 1]c.
 |
| Figure 1a: Pyoderma gangrenosum affecting the leg |
 |
| Figure 1b: Pyoderma gangrenosum affecting the chest wall |
 |
| Figure 1c: Pyoderma gangrenosum of the vulva |
Thirty five (94.6%) of the 37 patients with lesions confined to the legs and 13 (54.2%) of the 24 with lesions on other areas had only a single lesion of pyoderma gangrenosum (78.7% of total). Clinical types observed were the ulcerative variant in 55 (90.2%) and plaque type [Figure - 2] in 6 (9.8%). Two (3.3%) children below 3 years had a generalized distribution of ulcerative pyoderma gangrenosum [Figure - 3].
 |
| Figure 2: Plaque-type pyoderma gangrenosum affecting the leg |
 |
| Figure 3a: 3-year-old child with generalized pyoderma gangrenosum |
All patients complained of lesional pain with a visual analog scale score of 3–6. Pathergy testing was positive in nine (14.8%) cases. Seventeen (27.9%) patients had an associated systemic disease [Table - 1] and in 15 (88.2%) of them, the systemic disease preceded the pyoderma gangrenosum.
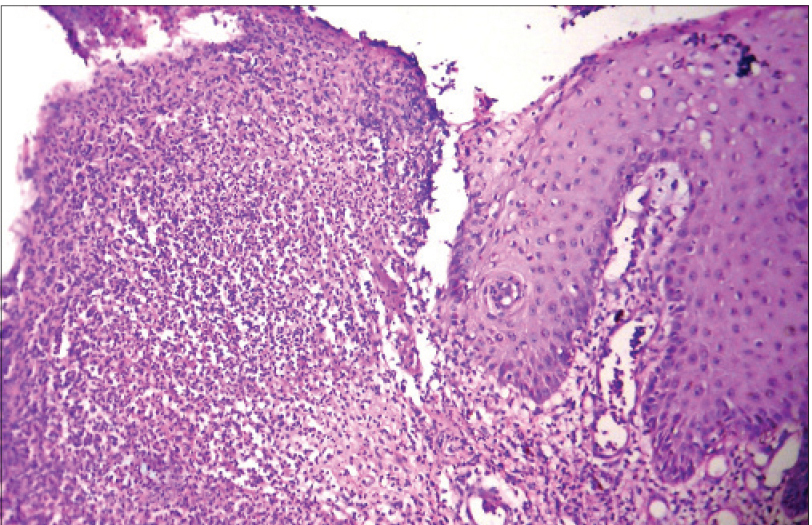
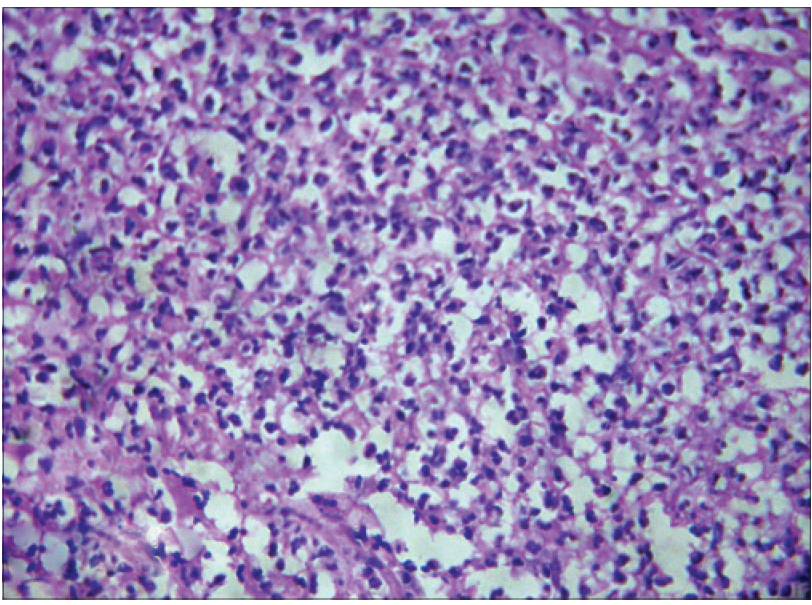
Consistent histological features observed were epidermal ulceration and a perivascular, predominantly neutrophilic inflammatory infiltrate in the dermis [Figure - 4].
 |
| Figure 3b: The same child with healed lesions following treatment with intravenous immunoglobulin G |
Depending on the treatment needed, there were 11 (18%) mild, 39 (63.9%) moderate and 11 (18%) severe cases of pyoderma gangrenosum [Table - 1]. None of our patients responded to potent topical or intralesional steroids alone. Nine (81.8%) of the eleven mild cases responded to colchicine, 0.5 mg twice daily and the remaining two, who had coexisting ulcerative colitis, responded to salazopyrin prescribed for the inflammatory bowel disease, along with local cleansing measures. Seven of the nine cases treated with colchicine developed recurrences within a year of stopping the drug which were again managed with the same drug.
Forty eight of the remaining fifty patients received prednisolone, 1 mg/kg/day orally. Two patients had co-existing diseases that could be worsened by daily steroid treatment. Thirty-nine of the 48 patients who received daily systemic steroids, including a 1½-year-old child, responded to treatment. Thirty-six of them required an additional immunomodulator to overcome the flares on tapeirng steroid (colchicine in 19, dapsone in 2, minocycline in 3, salazopyrin in 9 and azathioprine in 3 patients). Patients were tapered off steroids in 4–8 months whereas the steroid-sparing agents were continued for another 3–4 months.
The nine patients who failed to show an adequate response to daily systemic steroids and the two patients in whom co-existing diseases contraindicated daily steroid therapy were considered as having severe pyoderma gangrenosum. One was a 3-year-old female child who manifested generalized pyoderma gangrenosum [Figure - 3]a that did not respond to oral prednisolone. Administration of two pulses of intravenous immunoglobulin G (400 mg/kg body weight/day for 5 days) 28 days apart achieved complete resolution of lesions after which she was administered three more pulses [Figure - 3]b.
 |
| Figure 4a: Skin biopsy from ulcerated pyoderma gangrenosum showing ulcerated epidermis and dermal inflammatory infiltrate (H and E, ×100) |
 |
| Figure 4b: Higher magnification revealed the infiltrate to be predominantly composed of neutrophils (H and E, ×400) |
Dexamethasone pulse therapy (dexamethasone 100 mg in 500 ml 5% dextrose once in 28 days) was tried in the remaining 10 severe cases. Seven out of these 10 patients responded to pulse therapy (7–10 pulses) and 4 of them needed interval steroids and colchicine (0.5 mg twice daily) to manage the flare-ups in between pulses. Colchicine was slowly tapered over 4–6 months following completion of pulse therapy.
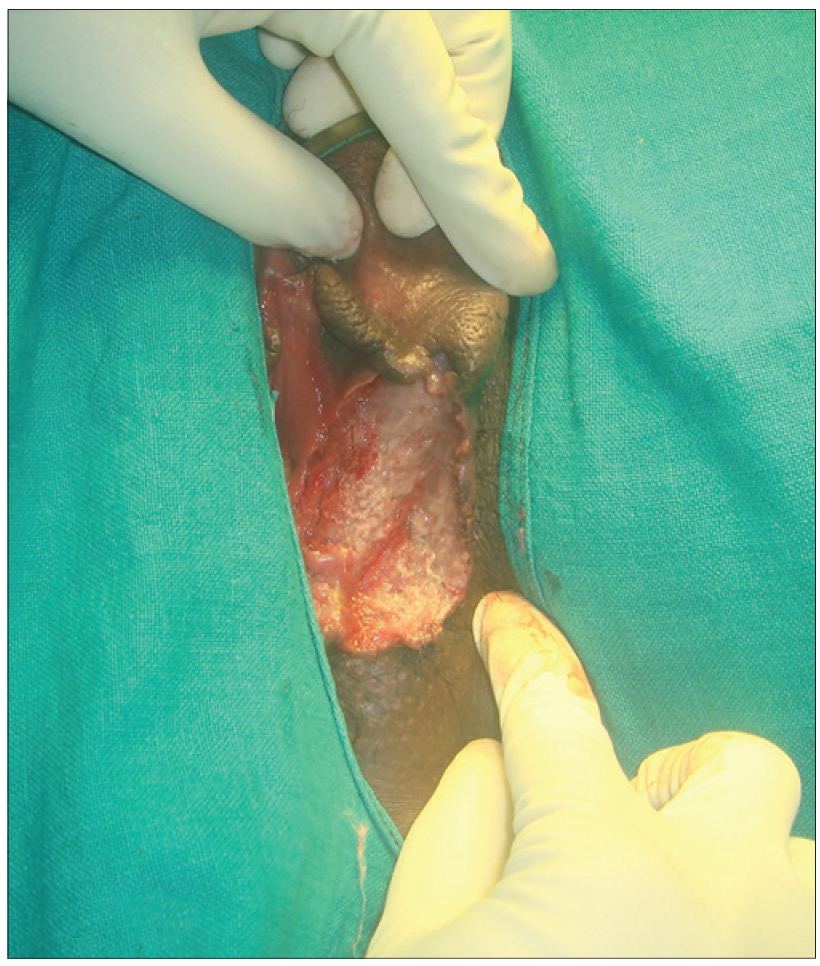
Split-thickness skin grafting was attempted in 3 patients, 1 man with diabetes mellitus and 2 women, one of whom had systemic lupus erythematosus. These patients had responded only partially to dexamethasone pulse therapy along with interval steroids and immunomodulators. Grafting was carried out within a week of dexamethasone pulse therapy and three more pulses were given to ensure immunosuppression during graft uptake. This allowed a satisfactory response in two patients, but the graft was not taken up in the patient with systemic lupus erythematosus. This last patient was being maintained on daily prednisolone 20 mg, azathioprine 50 mg and colchicine 0.5 mg twice daily; the ulcer had not healed completely at the time of this report.
Discussion
Pyoderma gangrenosum is an inflammatory disease characterized by neutrophil infiltration involving the skin and other organs. The disease usually affects the age group of 40–60 years.
The slight male predilection noted in our study was contrary to most previous studies.[1],[5],[6] The mean age of our study population was much lower than the observations of Ye and Ye and Al Ghazal et al. (58–62 years) but was consistent with certain other reports.[1],[3],[5] Though Bhat et al. noted a high percentage of childhood cases (27%), our findings were comparable to the data in other reports.[5],[7]
In concordance with most previous studies, ulcerative pyoderma gangrenosum was the most common variant in our study.[5],[6],[7] The absence of pustular pyoderma gangrenosum in our study population was surprising since the common underlying systemic disease in our subjects was inflammatory bowel disease. The clinical types and sites of involvement documented by us were consistent with previous reports.[2],[5],[6],[8] Positive pathergy documented in 14.8% of our study group was lower than the previously reported 20–50%.[2],[9] Whether pyoderma gangrenosum affecting areas other than the legs is at high risk for developing multiple ulcers (as observed by us) needs further evaluation.
We found systemic associations in 27.9% of cases, lower than in earlier reports.[1],[3],[8] Idiopathic hypereosinophilic syndrome, selective immunoglobulin E deficiency and lymphocytic colitis diagnosed in one of our patients are hitherto unreported associations with pyoderma gangrenosum.[10] In contrast to previous reports, associated arthritis was not found to be a poor prognostic factor in our study.[6]
The diagnostic challenge in the patient with systemic lupus erythematosus was in differentiating pyoderma gangrenosum from vasculitic ulceration of systemic lupus erythematosus. Perivascular neutrophilic infiltrate in the absence of fibrinoid necrosis in the biopsy specimen was more in favour of pyoderma gangrenosum whereas vasculitis in systemic lupus erythematosus manifests with a lymphocytic infiltrate and fibrinoid necrosis.
Pyoderma gangrenosum affecting the penis and vulva was distinguished from Behcet's disease by the absence of oral ulcers at the time of presentation or in the past, and after a thorough ophthalmologic evolution ruled out eye lesions suggestive of Behcet's disease. Moreover, Behcet's disease tends to produce ulceration over the scrotal skin rather than the penis.
Efficacy of inhibitors of neutrophil chemotaxis in pyoderma gangrenosum was demonstrated by the response to monotherapy with colchicine or salazopyrin in eleven (18%) of our patients. Similar to previous studies, steroids were the mainstay of treatment in our study as well.[5],[8] None of our patients showed a satisfactory response to topical or intralesional steroids, perhaps because patients attending a tertiary referral center such as ours generally have more severe disease. Systemic steroids (either as daily treatment or as pulse therapy) achieved disease control in most instances (75.4%) but most patients required other immunomodulators as well, to prevent flare-ups on tapering dose of systemic steroids. We found colchicine to be an effective drug in less severe pyoderma gangrenosum and a useful adjunct to systemic steroids in severe forms. However, we cannot comment on whether colchicine is better than other neutrophil chemotaxis inhibitors and only well-designed randomized controlled studies can answer this question. Intravenous immunoglobulin G (IVIG) and split-thickness skin grafting were tried in resistant cases; others have also found them to be beneficial in pyoderma gangrenosum.[3],[6],[11] Intravenous immunoglobulin G (IVIG) probably acts through the presence of antibodies against inflammatory mediators such as tumor necrosis factor-α, interleukins and interferon γ, and T-cell receptors.
The main limitation of our study was the relatively small sample size. We also cannot comment on the comparative efficacy of different drugs as this was not a randomized controlled study. Whenever treated patients came back to us with recurrent lesions, it was carefully documented, but we do not have reliable data on the recurrence rates following different modalities of treatment.
Conclusion
Male predilection and involvement in a younger age group were notable findings in our study. Whether pyoderma gangrenosum affecting body parts other than the legs is associated with a greater risk of extensive disease warrants further study. A major hindrance to a better understanding of pyoderma gangrenosum is its low prevalence. Multicentre studies on the clinical pattern, treatment response and systemic associations can throw light on the less-known aspects of this disease.
Acknowledgment
We express our sincere gratitude to all faculty and the postgraduates who were part of the Department of Dermatology, Government Medical College, Kozhikode, during the study period for their invaluable help.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Bhat RM. Management of pyoderma gangrenosum – An update. Indian J Dermatol Venereol Leprol 2004;70:329-35.
[Google Scholar]
|
| 2. |
Mamta A, Joshi A, Gulati A, Bansal R, Pathak VP. Localized granulomatous pyoderma gangrenosum. Indian J Dermatol Venereol Leprol 2003;69 Suppl S1:80-2.
[Google Scholar]
|
| 3. |
Ye MJ, Ye JM. Pyoderma gangrenosum: A review of clinical features and outcomes of 23 cases requiring inpatient management. Dermatol Res Pract 2014;2014:461467.
[Google Scholar]
|
| 4. |
Brocq L. A new contribution to the study of geometric phagedenism. Ann Dermatol Syphiligr 1916;9:1-39.
[Google Scholar]
|
| 5. |
Al Ghazal P, Herberger K, Schaller J, Strölin A, Hoff NP, Goerge T, et al. Associated factors and comorbidities in patients with pyoderma gangrenosum in Germany: A retrospective multicentric analysis in 259 patients. Orphanet J Rare Dis 2013;8:136.
[Google Scholar]
|
| 6. |
Wollina U. Pyoderma gangrenosum – A review. Orphanet J Rare Dis 2013;8:136.
[Google Scholar]
|
| 7. |
Bhat RM, Nandakishore B, Sequeira FF, Sukumar D, Kamath GH, Martis J, et al. Pyoderma gangrenosum: An Indian perspective. Clin Exp Dermatol 2011;36:242-7.
[Google Scholar]
|
| 8. |
Bhat RM. Pyoderma gangrenosum: An update. Indian Dermatol Online J 2012;3:7-13.
[Google Scholar]
|
| 9. |
Brooklyn T, Dunnill G, Probert C. Diagnosis and treatment of pyoderma gangrenosum. BMJ 2006;333:181-4.
[Google Scholar]
|
| 10. |
Riyaz N, Sasidharanpillai S, Rahima S, Bindu V, Shaan M, Raghavan NT, et al. Pyoderma gangrenosum in association with microscopic colitis, idiopathic hypereosinophilic syndrome, selective IgE deficiency and diabetes mellitus. Clin Exp Dermatol 2015;40:629-32.
[Google Scholar]
|
| 11. |
Cummins DL, Anhalt GJ, Monahan T, Meyerle JH. Treatment of pyoderma gangrenosum with intravenous immunoglobulin. Br J Dermatol 2007;157:1235-9.
[Google Scholar]
|
Fulltext Views
6,373
PDF downloads
3,239





