Translate this page into:
Pyoderma gangrenosum in a two year-old child
2 Department of Pathology, NKP Salve Institute of Medical Sciences and Research Centre, Nagpur, India
Correspondence Address:
Anne R Wilkinson
37, Chitnavis Layout, Byramji Town, Nagpur 440 013
India
| How to cite this article: Sharma R, Borkar MA, Oke MA, Wilkinson AR, Maimoon SA. Pyoderma gangrenosum in a two year-old child. Indian J Dermatol Venereol Leprol 2007;73:268-270 |
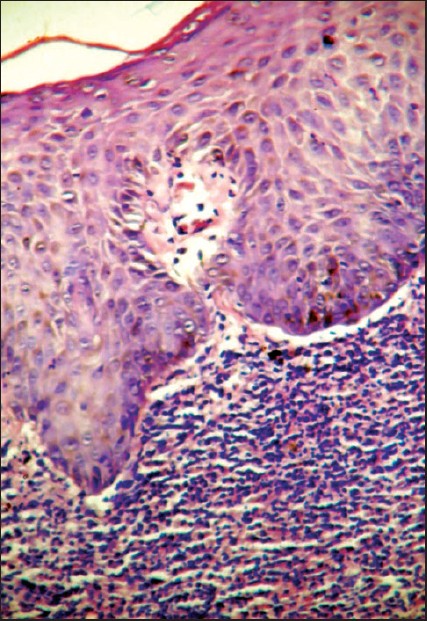 |
| Figure 2: Dense neutrophilic infiltration in the dermis (H/E, 100x) |
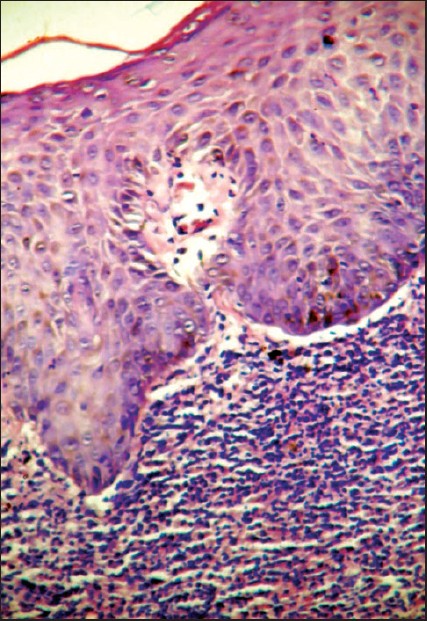 |
| Figure 2: Dense neutrophilic infiltration in the dermis (H/E, 100x) |
 |
| Figure 1: Bilateral gluteal ulcers with raised violaceous margins and central healing |
 |
| Figure 1: Bilateral gluteal ulcers with raised violaceous margins and central healing |
Sir,
Pyoderma gangrenosum is a neutrophilic dermatosis, which is seen in the fourth to fifth decade of life. Only about 4% of the patients are children and infants. [1] Although the precise pathogenesis is unknown, it is believed to be due to immune dysfunction. In about 50% of the cases, it may be associated with a variety of systemic conditions like inflammatory bowel disease, rheumatoid arthritis, hematological malignancies etc. Sometimes it may be an isolated occurrence, as in our case.
A two-year-old girl presented to the skin outpatient department (OPD) with a month-old history of nonhealing ulcers over both the gluteal regions and the left forearm. On examination, she was found to be emaciated and pale without any lymphadenopathy or any other systemic abnormality. Local examination revealed two large ulcers over both the gluteal regions, each measuring 15 x 15 cm [Figure - 1] and one ulcer measuring 9 x 4 cm on the forearm. All the ulcers had raised, undermined, boggy violaceous borders with an area of central healing and necrotic slough at the periphery. A clinical differential diagnosis of pyoderma gangrenosum, herpes simplex, amebic ulcers or deep fungal infection in an immunocompromised host was considered. She was hospitalized.
Her hemoglobin was 8 g%; total leukocyte count was 30,000/mm3; Neutrophil count 88% and lymphocyte count 12%. A peripheral smear showed microcytic hypochromic anemia. No abnormal cells were seen. Stool test for parasite and occult blood, serum Venereal Disease Research Laboratory (VDRL), Rheumatoid (RA) Factor, antinuclear antibody (ANA) and human immunodeficiency virus (HIV) tests were all negative. Chest X-ray was normal. New pustular lesions were seen at the site of venipuncture suggesting that the pathergy test was positive. With daily wound dressings, injectable antibiotics oral hematinics and two units of blood transfusion, the slough decreased but the ulcer progressed. The left gluteal ulcer biopsy showed dense infiltration by neutrophils and lymphocytes [Figure - 2] along with a leukocytoclastic response and evidence of vasculitis in the dermis. No granuloma, parasite or fungus was seen. The findings were consistent with pyoderma gangrenosum.
The patient was treated with oral steroids (methyl prednisolone 4 mg TDS (three times a day)). After two weeks, new pustules developed close to the gluteal ulcers. Methyl prednisolone pulse therapy [20 mg/kg over one hour in 5% dextrose for three days] was started to which the ulcers showed an immediate response. Oral prednisolone 5 mg BD (twice a day) was continued along with dapsone 25 mg/day and clofazimine 50 mg on alternate days. She was discharged after one and half months of hospitalization with partial healing of the ulcers.
The diagnosis of pyoderma gangrenosum is based on the typical clinical features and exclusion of other causes of ulcerative skin disorders. In children, the head and face area is a common site, with infants having an unusual distribution in the perianal and genital areas. [1] The lesions have an indolent course-they extend slowly in a creeping fashion and heal slowly from the periphery although central healing has been seen rarely. [2] The associated vasculitis may be a consequence rather than the cause of the lesion.
Various treatment options are available of which pulse steroid therapy produces a rapid improvement of the lesions. The duration of treatment with steroids may be from 5-11 months. [3] Aggressive cases may require a combination of systemic treatments. [4] Split skin grafts have been seen to be helpful after ensuring that the disease is quiescent to avoid pathergy. [5]
The long-term outcome for patients with pyoderma gangrenosum remains unpredictable. Recurrence rates up to 46% are seen regardless of the treatment prescribed. [6] A systemic organ involvement caused by aseptic neutrophilic abscesses influences the prognosis. Pulmonary involvement and endocarditis may (rarely) lead to death of the patients.
| 1. |
Graham JA, Hansen KK, Rabinowitz LG, Esterly NB. Pyoderma gangrenosum in infants and children. Pediatr Dermatol 1994;11:10-7.
[Google Scholar]
|
| 2. |
Wolff K, Stingl G. Pyoderma Gangrenosum. In : Fitzpatrick TB, Eisen AZ, Wolff K, Freedberg IM, Austen KF, editors. Dermatology in general medicine. Volume 1. 4 th ed. McGraw-Hill: New York; 1993. p. 1171-82.
[Google Scholar]
|
| 3. |
Bennett ML, Jackson JM, Jorizzo JL, Fleischer AB Jr, White WL, Callen JP. Pyoderma gangrenosum. A comparison of typical and atypical forms with an emphasis on time to remission. Case review of 86 patients from 2 institutions. Medicine (Baltimore) 2000;79:37-46.
[Google Scholar]
|
| 4. |
Gettler S, Rothe M, Grin C, Grant-Kels J. Optimal treatment of pyoderma gangrenosum. Am J Clin Dermatol 2003;4:597-608.
[Google Scholar]
|
| 5. |
Cliff S, Holden CA, Thomas PR, Marsden RA, Harland CC. Split skin grafts in the treatment of Pyoderma gangrenosum. Dermatol Surg 1999;25:299-302.
[Google Scholar]
|
| 6. |
Mlika RB, Riahi I, Fenniche S, Mokni M, Dhaoui MR, Dess N, et al. Pyoderma gangrenosum: A report of 21 cases. Int J Dematol 2002;41:65-8.
[Google Scholar]
|
Fulltext Views
4,410
PDF downloads
1,320





