Translate this page into:
Rare case of herpes zoster ophthalmicus with orbital myositis, oculomotor nerve palsy and anterior uveitis
2 Department of Neuro Ophthalmology, Aravind Eye Hospital and Postgraduate Institute of Ophthalmology, Coimbatore, Tamil Nadu, India
Corresponding Author:
Virna M Shah
Department of Neuro Ophthalmology, Aravind Eye Hospital and Postgraduate Institute of Ophthalmology, Coimbatore, Tamil Nadu
India
virna@cbe.aravind.org
| How to cite this article: Daswani M, Bhosale N, Shah VM. Rare case of herpes zoster ophthalmicus with orbital myositis, oculomotor nerve palsy and anterior uveitis. Indian J Dermatol Venereol Leprol 2017;83:365-367 |
Sir,
A 67-year-old woman, a known diabetic and hypertensive, presented to Aravind Eye Hospital, Coimbatore, with complaints of pain in the right eye since 1 month. There was no history of any other disease causing immunosuppression. She had a history of painful vesicles on the right side of forehead and right upper eyelid one month back, associated with ipsilateral eye pain, for which she took some treatment from a dermatologist at the time. However, she came to the ophthalmologist a month after the onset of symptoms. The best corrected visual acuity was 6/60 in the right eye and 6/18 in the left eye. On examination of the right eye, drooping of the upper lid was seen suggestive of ptosis, healed pigmented scars on the right side of forehead and lid [Figure - 1]. Circumcorneal congestion was seen and cornea was hazy with punctate epithelial erosions and keratic precipitates. Anterior chamber had cells and flare; posterior synechiae were present from 1 to 4 o'clock and 8 to 10 o'clock positions [Figure - 2]. Corneal sensations were absent in the right eye. The pupil was not reacting to direct and consensual light. The lens showed immature cataract. Extraocular movements were restricted on levo- and dextro-elevation. The left eye was essentially normal, except for immature cataract. The posterior segment of both eyes were normal. The patient was diagnosed as a case of herpes zoster ophthalmoplegia with pupil involving third nerve palsy. Magnetic resonance imaging showed asymmetric thickening of the right extraocular muscles, suggestive of orbital myositis, and thickening of the right oculomotor nerve.
 |
| Figure 1: External examination showing healed vesicular eruptions on the right forehead, right upper lid and right side of nose. Right upper lid shows ptosis |
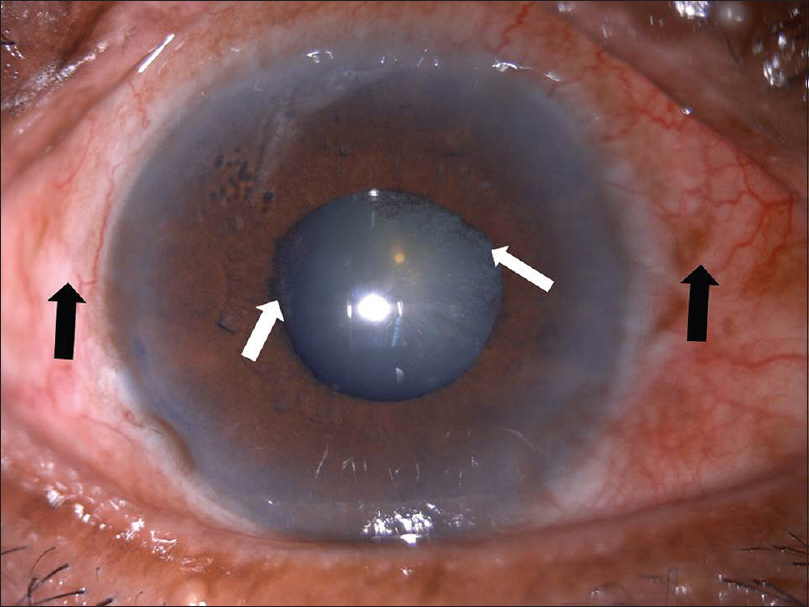 |
| Figure 2: Right eye with circumcorneal congestion (black arrows) and posterior synechiae (white arrows) |
The patient was treated with oral acyclovir 800 mg thrice a day for a week, antibiotic-steroid combination (chloramphenicol 0.5% + dexamethasone 0.1%) eye drops, acyclovir 3% eye ointment and homatropine eye drops for about a month in the right eye. As there was active inflammation in the eye, oral acyclovir was continued. One-month follow-up showed visual improvement to 6/12 in the right eye with resolving ophthalmoplegia.
Ocular complications are observed in 20%–70% of the cases of herpes zoster ophthalmicus and include follicular conjunctivitis, epithelial or interstitial keratitis, dendritic keratitis, uveitis, scleritis or episcleritis, chorioretinitis, optic neuropathy and ocular motility disorders.[1] The virus often involves the cornea reducing corneal sensitivity causing neurotrophic ulceration and decreased vision secondary to scarring. Hutchinson's sign, that is the presence of rash at the tip of the nose signifies nasociliary nerve involvement, suggests an increased risk of corneal and ocular sequelae.[2]
Ophthalmoplegia is rare and self-limiting and is usually seen in 7%–31% of cases, more common in the elderly patients. Among them, the third nerve is most commonly involved and the fourth cranial nerve is least commonly involved.[3] Ophthalmoplegia occurs within 1–3 weeks of the onset of rash.[4] Pathogenesis of ophthalmoplegia in herpes zoster can be due to the direct cytopathic effect of the virus or a reactive immunologic response to the virus. Other mechanisms include occlusive vasculitis induced by the virus or activation of another latent neuropathic virus by the zoster virus.[5] Orbital myositis can also be a cause for the ophthalmoplegia. On reviewing the literature it is found that, ophthalmoplegia occurs as a result of either nerve or muscle involvement. In our patient, the restriction of ocular movements was a result of simultaneous nerve and muscle inflammation. Postherpetic neuralgia is one of the most common complications. It can be defined as clinically significant pain or painful sensations that persist 3 months or more after the onset of rash. The risk increases with advancing age and has been known to develop in patients with associated keratitis, conjunctivitis and uveitis. The treatment goal is the administration of an antiviral drug that crosses the blood–brain barrier. Acyclovir, valacyclovir, and famciclovir have been used for treating the skin lesions, bringing down the viral load and decreasing the risk of ocular involvement. If keratitis or episcleritis is present, topical antiviral and steroid drops can be used. Ophthalmoplegia, being self-limiting, has a good prognosis. The time taken for its resolution varies between 2 and 18 months. Diplopia, if present, recovers within 1 year.[3]
Patients can present with ophthalmoplegia following an episode of herpes zoster ophthalmicus. Simultaneous features of myositis, oculomotor nerve palsy, keratitis and anterior uveitis can also occur, as seen in our case. This case highlights the importance of timely referral of all patients with herpes zoster ophthalmicus to an ophthalmologist, to avoid ocular complications, which can lead to permanent blindness.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient has given her consent for her images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. | Chhabra MS, Golnik KC. Recovery of ocular motor cranial nerve palsy after herpes zoster ophthalmicus. J Neuroophthalmol 2014;34:20-2. [Google Scholar] |
| 2. | Zaal MJ, Völker-Dieben HJ, D'Amaro J. Prognostic value of Hutchinson's sign in acute herpes zoster ophthalmicus. Graefes Arch Clin Exp Ophthalmol 2003;241:187-91. [Google Scholar] |
| 3. | Chaker N, Bouladi M, Chebil A, Jemmeli M, Mghaieth F, El Matri L. Herpes zoster ophthalmicus associated with abducens palsy. J Neurosci Rural Pract 2014;5:180-2. [Google Scholar] |
| 4. | Horton JC. Neurovisual manifestations of herpesviruses. Int Ophthalmol Clin 2002;42:33-41. [Google Scholar] |
| 5. | Sanjay S, Chan EW, Gopal L, Hegde SR, Chang BC. Complete unilateral ophthalmoplegia in herpes zoster ophthalmicus. J Neuroophthalmol 2009;29:325-37.2 [Google Scholar] |
Fulltext Views
3,865
PDF downloads
2,505





